Given the pronounced hypoglycemic effect of GLP-1, pharmaceutical companies have focused their efforts on creating drugs that support or imitate the effect of this hormone. As a result, 2 groups of drugs were created:
- substances that mimic the action of GLP-1 (GLP-1 agonists);
- substances that prolong the action of endogenous GLP-1 ( DPP-4 ).
Native GLP-1 is rapidly destroyed by the enzyme dipeptidyl peptidase-4 (DPP-4): when administered intravenously, the half-life of GLP-1 is only 1.5-2.0 minutes (Fig. 7).
Therefore, drugs have been synthesized (GLP-1 mimetic and analogues) that are resistant to the destructive effect of DPP-4, which increases the duration of their action to 12 hours (GLP-1 mimetic - Exenatide) or 24 hours (human GLP-1 analogue - liraglutide) . GLP-1 agonists slow gastric emptying and promote faster satiety, which leads to weight loss. GLP-1 receptor agonists have been reported to improve myocardial function in people who have had myocardial infarction, as well as improve endothelial function and reduce systolic blood pressure.
The second method of overcoming the destructive effect of DPP-4 was the creation of inhibitors of this enzyme. These drugs are taken orally and interfere with the process of destruction of the body's own GLP-1.
Below is a comparison of DPP-4 inhibitors and GLP-1 agonists on a number of parameters:
- DPP-4 i: Route of administration: orally
- GLP-1 concentration: physiological (can be increased by 2 times)
- GIP concentration: increase
- Side effects from the gastrointestinal tract: rare
- Effect on body weight: negligible
- Frequency of hypoglycemia: low
- Decrease in HbA1c: — 0.5% — 1.1%
- Effect on β-cell mass*: increases
- Method of administration: subcutaneously
* — in an animal experiment
The first of the group of human GLP-1 analogues is liraglutide (Victoza). In July 2009, this drug was approved for use in Europe, in January 2010 - in the USA, in Russia Victoza was registered in May 2010.
The molecule of the drug liraglutide is 97% homologous in amino acid composition to native human GLP-1, while the similarity of the incretin mimetic Exenatide (Byeta) with human GLP-1 is only 53%. Next, we will describe the effects of a group of GLP-1 agonists using the example of a human analogue.
Mechanism of action
The liraglutide molecule was obtained by modifying human GLP-1 by replacing one amino acid (arginine with lysine) at position 34 and adding palmitic acid to the C16 lysine at position 26 (Fig. 8).
These changes provided protection of liraglutide from degradation by DPP-4, as well as the ability to bind to plasma albumin and form micelle-like aggregates in subcutaneous fat. These aggregates are slowly absorbed from the subcutaneous depot and circulate in the blood for a long time. The half-life of liraglutide is 10-14 hours, which ensures its stable concentration when administered once a day after 3 consecutive injections.
As an analogue of human GLP-1, liraglutide has effects similar to human GLP-1:
- Glucose-dependent stimulation of insulin secretion and suppression of glucagon secretion. Against the background of hyperglycemia, liraglutide stimulates insulin secretion and suppresses glucagon secretion, and with normal or low glycemic values these effects are not observed.
- This mechanism helps prevent the development of hypoglycemic conditions.
Description of the drug VICTOZA®
Hypoglycemic agent. Liraglutide is a human GLP-1 analogue produced by recombinant DNA biotechnology using a Saccharomyces cerevisiae strain that has 97% homology to human GLP-1, which binds to and activates GLP-1 receptors in humans. The GLP-1 receptor serves as a target for native GLP-1, an endogenous incretin hormone that stimulates glucose-dependent insulin secretion in pancreatic beta cells. Unlike native GLP-1, the pharmacokinetic and pharmacodynamic profiles of liraglutide allow it to be administered to patients subcutaneously once daily.
The long half-life of the drug from plasma is ensured by three mechanisms:
- self-association, which results in delayed absorption of the drug, binding to albumin and a higher level of enzymatic stability in relation to dipeptidyl peggidase-4 (DPP-4) and the enzyme neutral endopeptidase (NEP).
Liraglutide interacts with GLP-1 receptors, resulting in increased concentrations of cyclic adenosine monophosphate (cAMP). Thus, under the influence of liraglutide, glucose-dependent stimulation of insulin secretion and improvement of the function of pancreatic beta cells occurs. At the same time, under the influence of liraglutide, glucose-dependent suppression of excessively high glucagon secretion occurs. Thus, with an increase in blood glucose concentration, insulin secretion is stimulated and glucagon secretion is suppressed. On the other hand, at low blood glucose concentrations, liraglutide reduces insulin secretion but does not suppress glucagon secretion. The mechanism for lowering glycemic levels also includes a slight delay in gastric emptying. Liraglutide reduces body weight and reduces body fat mass through mechanisms that cause a decrease in hunger and a decrease in energy expenditure.
GLP-1 is a physiological regulator of appetite and calorie intake, and GLP-1 receptors are located in several areas of the brain involved in appetite regulation.
In animal studies, peripheral administration of liraglutide resulted in drug uptake into specific regions of the brain, including the hypothalamus, where liraglutide, through specific activation of GLP-1 receptors, increased satiety signals and decreased hunger signals, thereby leading to weight loss. GLP-1 receptors are also present in specific areas of the heart, blood vessels, immune system and kidneys. Human and animal studies have shown that activation of GLP-1 receptors by liraglutide may have cardiovascular and microcirculatory effects, including reducing inflammation. Animal studies have shown that liraglutide slows the development of atherosclerosis.
Experimental animal studies using prediabetic models showed that liraglutide slows the progression of diabetes mellitus. In vitro diagnostics showed that liraglutide is a potent factor in specifically stimulating the proliferation of pancreatic beta cells and preventing beta cell death (apoptosis) induced by cytokines and free fatty acids. In vivo, liraglutide increases insulin biosynthesis and increases pancreatic beta cell mass in experimental animal models of diabetes. When glucose concentrations return to normal, liraglutide stops increasing pancreatic beta cell mass.
Release form and dosage regimen
The drug liraglutide is available as a solution for subcutaneous administration, in a pre-filled syringe pen. Each pen can be designed to deliver 15 doses of 1.2 mg or 10 doses of 1.8 mg. The pen should be stored in the refrigerator at a temperature of +2 to +8°C. After the first use, it can be kept at room temperature (below 30°C) or in the refrigerator (2-8°C) for a month. The handle must not be frozen.
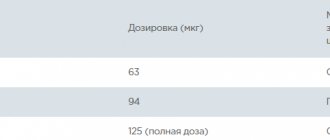
Liraglutide is injected once daily subcutaneously into the abdomen, thigh, or upper arm at any time of the day. Within 1 week from the start of treatment, the dose of liraglutide should be 0.6 mg per day to ensure optimal tolerability of the drug. From the second week, the daily dose must be increased to 1.2 mg. If it is impossible to achieve target values at this dose of the drug, the amount of liraglutide administered can be increased to a maximum of 1.8 mg per day.
Mode of application
Victoza cannot be administered intravenously or intramuscularly.
The drug Victoza is administered once a day at any time, regardless of meals. It can be injected subcutaneously into the anterior abdominal wall, thigh or shoulder. The place and time of injections can be changed without dose adjustment. However, it is advisable to administer Victoza at approximately the same, most convenient time of day.
Additional recommendations for administration are presented in the instructions for using the syringe pen for the drug Victoza.
Efficacy of liraglutide in clinical studies
The phase III liraglutide research program “Study of the Effect and Action of Liraglutide in Diabetes (LEAD™)” included about 6,500 patients from 41 countries, including Russia. Among them, approximately 4,445 patients received liraglutide. The goal of the program was to determine the indications for the use of liraglutide for the treatment of T2DM in monotherapy and in combination with traditional glucose-lowering drugs. The LEAD program compared the efficacy and safety of liraglutide with sulfonylureas, glitazones, insulin glargine, and exenatide. (Fig. 9).
The effects of liraglutide compared with sitagliptin in combination with metformin in patients with T2DM were assessed in an international, multicenter, 26-week, randomized, open-label, parallel-group study.
- The dynamics of HbAlc reduction in these studies averaged -1.6%. Two years of liraglutide monotherapy (1.8 and 1.2 mg) demonstrated significant and sustained improvements in glycemic control (-1.1 and -0.9%, respectively, compared with -0.6% on glimepiride) and body weight ( -2.7 kg and -2.1 kg compared with + 1.1 kg on glimepiride) against the background of a low risk of hypoglycemia (6 times less often) compared with motor therapy with glimepiride.
- The maximum reduction in HbA1c when adding liraglutide to metformin monotherapy was 2.74% in the subgroup of patients with an initial HbA1c level >9.5%.
According to the study results, while taking liraglutide, 52-65% of patients achieve HbA1c levels <7% with a minimal risk of hypoglycemia. Liraglutide also causes rapid and sustained weight loss, a clinically significant reduction in systolic blood pressure, and an improvement in β-cell function.
Victoza solution for subcutaneous administration 6 mg/ml 3 ml syringe pen 2 pcs. in Moscow
Mechanism of action
Liraglutide is a human glucagon-like peptide-1 (GLP-1) analog produced by recombinant DNA biotechnology using a strain of Saccharomyces cerevisiae
, which has 97% homology with human GLP-1, which binds and activates GLP-1 receptors in humans. The GLP-1 receptor serves as a target for native GLP-1, an endogenous incretin hormone that stimulates glucose-dependent insulin secretion in pancreatic beta cells. Unlike native GLP-1, the pharmacokinetic and pharmacodynamic profiles of liraglutide allow it to be administered to patients once a day.
The long-acting profile of liraglutide by subcutaneous injection is ensured by three mechanisms: self-association, which results in delayed absorption of the drug; binding to albumin and a higher level of enzymatic stability in relation to dipeptidyl peptidase-4 (DPP-4) and the enzyme neutral endopeptidase (NEP), thereby ensuring a long T1/2 of the drug from plasma. Liraglutide acts through interaction with specific GLP-1 receptors, resulting in an increase in cAMP levels. Under the influence of liraglutide, there is a glucose-dependent stimulation of insulin secretion and an improvement in the function of pancreatic beta cells. At the same time, liraglutide suppresses excessively high glucose-dependent glucagon secretion. Thus, with an increase in blood glucose concentration, insulin secretion is stimulated and glucagon secretion is suppressed. On the other hand, during hypoglycemia, liraglutide reduces insulin secretion but does not suppress glucagon secretion. The mechanism for lowering glycemic levels also includes a slight delay in gastric emptying. Liraglutide reduces body weight and reduces adipose tissue through mechanisms that cause a decrease in hunger and energy expenditure.
Studies in animal models of prediabetes have shown that liraglutide slows the progression of diabetes mellitus. In vitro diagnostics
showed that liraglutide is a potent factor in specifically stimulating the proliferation of pancreatic beta cells and preventing the formation of cytokines and free fatty acids that induce beta cell death (apoptosis).
In vivo
, liraglutide increases insulin biosynthesis and increases beta cell mass in an experimental animal model of diabetes. When glucose concentrations return to normal, liraglutide stops increasing pancreatic beta cell mass.
Liraglutide has a long-lasting 24-hour effect and improves glycemic control by reducing fasting and postprandial blood glucose concentrations in patients with type 2 diabetes mellitus.
Glucose-dependent insulin secretion.
As blood glucose concentrations increase, liraglutide increases insulin secretion. When a graded glucose infusion is used, insulin secretion after a single dose of liraglutide in patients with type 2 diabetes mellitus increases to a level comparable to that in healthy subjects (Fig. 1).
Picture 1.
Pancreatic beta cell function.
Liraglutide improves the function of pancreatic beta cells, as evidenced by the first and second phases of the insulin response and the maximum secretory activity of beta cells. Pharmacodynamic studies in patients with type 2 diabetes mellitus showed restoration of the first phase of insulin secretion (IV insulin), improvement of the second phase of insulin secretion (hyperglycemic clamp test) and maximum insulin secretory activity (arginine stimulation test).
During 52 weeks of therapy with Victoza®, there was an improvement in pancreatic beta cell function, which was confirmed by assessment of the homeostatic model of pancreatic beta cell function (HOMA index) and the insulin to proinsulin ratio.
Glucagon secretion.
Liraglutide, by stimulating insulin secretion and suppressing glucagon secretion, reduces blood glucose concentrations. Liraglutide does not suppress the glucagon response to low glucose concentrations. In addition, with liraglutide, lower production of endogenous glucose is observed.
Gastric emptying.
Liraglutide causes a slight delay in gastric emptying, which leads to a decrease in the rate of postprandial glucose entering the blood.
Body weight, body composition and energy expenditure.
In overweight subjects enrolled in long-term clinical studies of liraglutide, liraglutide produced significant weight loss. Computed tomography (CT) and dual-energy X-ray absorptiometry (DXA) scans showed that the weight loss was primarily due to the loss of fat tissue in the patients. These results are explained by the fact that during treatment with liraglutide, patients experience a decrease in hunger and energy expenditure.
Electrophysiology of the heart (ECS).
The effect of liraglutide on the repolarization process in the heart was tested in the EFS study. The use of liraglutide at equilibrium concentration in a daily dose of up to 1.8 mg does not prolong EFS.
Clinical effectiveness.
3992 patients with type 2 diabetes were randomized in 5 double-blind safety and efficacy clinical trials designed to evaluate the effect of Victoza® on glycemic control. Treatment with Victoza® causes clinically and statistically significant improvements in HbA1c, fasting glucose and postprandial glucose compared to placebo.
Glycemic control.
The drug Victoza® in the form of monotherapy for 52 weeks causes a statistically significant (p<0.0014) and long-lasting decrease in HbA1c compared with the same indicator in patients receiving glimepiride therapy. At the same time, the noted decrease in HbA1c below the level of 7% persists for 12 months (Fig. 2).
Figure 2.
In patients with HbA1c above 9.5% at baseline, this indicator decreased by 2.1% during monotherapy with Victoza®, while in patients participating in combination clinical trials of Victoza®, the average HbA1c level decreased by 1.1–2.5%.
The drug Victoza® during 26-week combination therapy with metformin, sulfonylureas or metformin and a thiazolidinedione causes a statistically significant (p < 0.0001) and long-lasting decrease in HbA1c levels compared with that in patients receiving placebo.
In patients who did not achieve adequate glycemic control on Victoza® and metformin therapy, the addition of insulin detemir provided greater efficacy compared to Victoza® and metformin therapy after 26 weeks of treatment (0.52% reduction in HbA1c levels). It has been proven that the effectiveness of Victoza® at a dose of 0.6 mg in combination with sulfonylureas or metformin is superior to placebo, but at the same time is lower compared to dosages of 1.2 and 1.8 mg.
Proportion of patients achieving a reduction in HbA1c levels.
During the 52-week study, during the 52-week study, the number of patients achieving an HbA1c level of <7% increased statistically significantly (p≤0.0007) compared to the number of patients receiving glimepiride. At the 26th week of using Victoza® in combination with metformin, sulfonylurea drugs or a combination of metformin with thiazolidinediones, the number of patients achieving an HbA1c level of ≤6.5% increased statistically significantly (p≤0.0001) relative to the number of patients who received therapy with hypoglycemic drugs without the addition of Victoza®.
In groups of patients who did not achieve adequate glycemic control on therapy with Victoza® and metformin, the percentage of patients who achieved the target HbA1c level (<7 and ≤6.5%) was significantly higher during therapy with insulin detemir + liraglutide 1.8 mg + metformin , compared with therapy with liraglutide 1.8 mg + metformin (p≤0.0001/p=0.0016).
In a 26-week combination study of Victoza®, it was possible to achieve HbA1c levels <7% in more patients receiving the drug as combination therapy compared to the number of patients receiving it as monotherapy.
Fasting blood glucose level.
Fasting glucose concentrations decreased by 13–43.5 mg% (0.72–2.42 mmol/l) while taking Victoza®, both as monotherapy and in combination with one or two oral hypoglycemic agents. This decrease was observed already within the first two weeks of treatment.
Postprandial glycemic level.
The use of the drug Victoza® for 3 days of eating a standard meal helped reduce the concentration of postprandial glucose by 31–49 mg% (1.68–2.71 mmol/l).
Body mass.
52-week monotherapy with Victoza® was associated with sustained weight loss.
Throughout the clinical study period, sustained weight loss was also associated with the use of Victoza® in combination with metformin and in combination with combinations of metformin with sulfonylureas or metformin with thiazolindione.
Weight loss in patients receiving Victoza® in combination with metformin was also observed after the addition of insulin detemir.
The greatest reduction in body weight was observed in patients who had an increased body mass index (BMI) at the starting point of the study.
Monotherapy with Victoza® for 52 weeks caused a decrease in average waist circumference by 3–3.6 cm.
Weight loss was observed in all patients treated with Victoza®, regardless of whether or not they experienced an adverse reaction in the form of nausea.
The drug Victoza® as part of combination therapy with metformin reduced the volume of subcutaneous fat by 13–17%.
Non-alcoholic steatohepatosis.
Liraglutide reduces the severity of steatohepatosis in patients with type 2 diabetes mellitus.
Blood pressure indicators.
Long-term clinical studies have shown that Victoza® reduces SBP by an average of 2.3–6.7 mmHg. in the first 2 weeks of treatment. The drug Victoza®, acting on ATP III, reduces the incidence of metabolic syndrome. The decrease in SBP occurred before the onset of weight loss.
Other clinical data.
In a comparative study of the effectiveness and safety of the drug Victoza® (at doses of 1.2 and 1.8 mg) and the DPP-4 inhibitor sitagliptin at a dose of 100 mg in patients who did not achieve adequate control on metformin therapy, after 26 weeks of treatment, a better reduction in the indicator was proven HbA1c when using the drug Victoza® at both doses compared with sitagliptin (-1.24, -1.5% compared to -0.9%, p < 0.0001). Significantly more patients achieved HbA1c levels below 7% with Victoza® compared to sitagliptin (43.7% vs. 56% vs. 22%, p<0.0001). Weight loss in patients receiving Victoza® was significantly greater compared with patients receiving sitagliptin (-2.9 and -3.4 kg versus -1 kg, p < 0.0001).
Compared with patients receiving sitagliptin, patients receiving Victoza® were more likely to experience nausea. However, the nausea was transient. The incidence of mild hypoglycemia was not significantly different between treatment with Victoza® and sitagliptin (0.178 and 0.161 compared with 0.106 cases/patient per year). A decrease in HbA1c levels and an advantage of Victoza® compared to sitagliptin was observed after the 26th week of treatment with Victoza® (1.2 and 1.8 mg) and was confirmed after the 52nd week of treatment (-1.29 and -1.51 % versus -0.88%, p<0.0001). After 52 weeks of sitagliptin use, patients were switched to Victoza®, which led to an additional and statistically significant decrease in HbA1c at 78 weeks of treatment (0.24 and 0.45%, 95 C1: from 0.41 to 0.07 and -0.67 to 0.23), but no control group of patients was available.
In a comparative study of the effectiveness and safety of Victoza® (at a dose of 1.8 mg) and exenatide (at a dose of 10 mcg 2 times a day) in patients who did not achieve adequate control on therapy with metformin and/or sulfonylurea derivatives, after 26 weeks of use of the drug Victoza® showed a greater reduction in HbA1c compared to exenatide (-1.12% versus -0.79%, p<0.0001).
Significantly more patients achieved HbA1c levels below 7% on Victoza® therapy compared with exenatide (54.2% versus 43.4%, p=0.0015). Both treatments showed an average weight loss of approximately 3 kg. The number of patients reporting nausea was lower in the group of patients receiving Victoza® compared to exenatide. The incidence of mild hypoglycemia was significantly lower in the group of patients receiving Victoza® compared to exenatide (1.932 versus 2.6 cases/patient per year, p = 0.01). After 26 weeks of using exenatide, patients were switched to Victoza®, which led to an additional decrease in HbA1c at week 40 of treatment (-0.32%, p < 0.0001), 13% of patients managed to achieve an HbA1c level below 7% .
Treatment with Victoza® for 52 weeks improved insulin sensitivity compared with that of sulfonylureas, as determined by the HOMA-IR homeostatic model for assessing insulin resistance.
Antihyperglycemic effect of liraglutide
Studies have shown that liraglutide was more effective than other drugs in reducing HbA1c levels in all series of trials. At the same time, the maximum decrease in HbA1c during monotherapy was 1.6% compared to the initial value.
- In monotherapy, liraglutide at a dose of 1.8 mg per day demonstrated significantly greater efficacy than at a dose of 1.2 mg per day (HbA1c levels decreased by 1.6 and 1.2%, respectively), and significantly greater efficacy than glimepiride monotherapy in dose of 8 mg per day (HbA1c decreased by 0.9%) over 52 weeks of treatment (Fig. 10).
- After 1 year of treatment, the number of patients achieving treatment goals (HbA1 < 7%) was significantly higher among those taking liraglutide at both doses (58% and 62% at doses of 1.2 mg and 1.8 mg, respectively) compared with glimepiride at a dose of 8 mg (31%).
- In all of these LEAD studies, liraglutide provided rapid and sustained reductions in fasting hyperglycemia, greater than glimepiride and rosiglatizone and comparable to insulin glargine.
- When compared with the GLP-1 mimetic exenatide, liraglutide was significantly more effective in reducing HbA1c levels (by 1.1% versus 0.8%) and fasting hyperglycemia. However, hyperglycemia after breakfast and dinner was better reduced when taking exenatide due to its twice-daily administration.
- Mild hypoglycemia also occurred less frequently in patients receiving liraglutide compared with patients receiving exenatide (1.93 with liraglutide versus 2.60 events per patient per year with exenatide).
The Lancet in 2010 published the results of the first international multicenter 26-week randomized, open-label study of liraglutide compared with sitagliptin in combination with metformin in patients with type 2 diabetes.
- Liraglutide provided significantly greater reductions in HbA1c, fasting plasma glucose (FPG) and body weight compared with sitagliptin (Januvia) with similar or higher overall treatment satisfaction.
- Using liraglutide at a dose of 1.8 mg and 1.2 mg, 54.6 and 43.4% of patients, respectively, achieved treatment goals, and in the sitagliptin 100 mg group - 22.4% of patients (Fig. 11).
Key results comparing liraglutide and sitagliptin therapy in terms of hypoglycemic effect are as follows:
- The drug liraglutide provided a greater reduction in HbA1c levels (-1.50% and -1.24% at dosages of 1.8 mg and 1.2 mg, respectively) compared to sitagliptin (-0.90%).
- The mean reduction in fasting plasma glucose was significantly greater in the liraglutide-treated group.
- The study also assessed patient satisfaction with treatment using the Diabetes Treatment Satisfaction Questionnaire (DTSQ), which is used in many diabetes drug trials: The increase in overall treatment satisfaction was greater with liraglutide 1.8 mg than with liraglutide 1.8 mg. during therapy with sitagliptin.
- There were no differences in perceived comfort of treatment (oral versus injectable route).
Victoza®
Mechanism of action
Liraglutide is a human glucagon-like peptide-1 (GLP-1) analog produced by recombinant DNA biotechnology using a strain of Saccharomyces cerevisiae
, which has 97% homology with human GLP-1, which binds and activates GLP-1 receptors in humans. The GLP-1 receptor serves as a target for native GLP-1, an endogenous incretin hormone that stimulates glucose-dependent insulin secretion in pancreatic beta cells. Unlike native GLP-1, the pharmacokinetic and pharmacodynamic profiles of liraglutide allow it to be administered to patients once a day.
The long-acting profile of liraglutide when administered subcutaneously is provided by three mechanisms: self-association, which results in delayed absorption of the drug, binding to albumin and a higher level of enzymatic stability in relation to dipeptidyl peptidase-4 (DPP-4) and the enzyme neutral endopeptidase (NEP), behind This ensures a long half-life of the drug from plasma. The action of liraglutide is due to interaction with specific GLP-1 receptors, resulting in an increase in the concentration of cyclic adenosine monophosphate (cAMP). Under the influence of liraglutide, there is a glucose-dependent stimulation of insulin secretion and an improvement in the function of pancreatic beta cells. At the same time, under the influence of liraglutide, glucose-dependent suppression of excessively high glucagon secretion occurs. Thus, with an increase in blood glucose concentration, insulin secretion is stimulated and glucagon secretion is suppressed. On the other hand, during hypoglycemia, liraglutide reduces insulin secretion but does not suppress glucagon secretion. The mechanism of lowering glycemic levels also includes a slight delay in gastric emptying.
Liraglutide reduces body weight and reduces body fat mass through mechanisms that cause a decrease in hunger and a decrease in energy expenditure.
GLP-1 is a physiological regulator of appetite and calorie intake, and GLP-1 receptors are located in several areas of the brain involved in appetite regulation.
In animal studies, peripheral administration of liraglutide resulted in drug uptake into specific regions of the brain, including the hypothalamus, where liraglutide, through specific activation of GLP-1 receptors, increased satiety signals and decreased hunger signals, thereby leading to weight loss.
Studies in animal models of prediabetes have shown that liraglutide slows the progression of diabetes mellitus. In vitro diagnostics
showed that liraglutide is a potent factor in specifically stimulating the proliferation of pancreatic beta cells and preventing beta cell death (apoptosis) induced by cytokines and free fatty acids.
In vivo
, liraglutide increases insulin biosynthesis and increases beta cell mass in experimental animal models of diabetes mellitus. When glucose concentrations return to normal, liraglutide stops increasing pancreatic beta cell mass.
Pharmacodynamics
The drug Victoza® has a long-term 24-hour effect and improves glycemic control by reducing fasting and postprandial blood glucose concentrations in patients with type 2 diabetes mellitus.
Glucose-dependent insulin secretion
As the concentration of glucose in the blood increases, the drug Victoza® increases insulin secretion. When using a staged glucose infusion, insulin secretion after a single dose of Victoza® in patients with type 2 diabetes mellitus increases to a level comparable to that in healthy subjects (Fig. 1).
Pancreatic beta cell function
The drug Victoza® improved the function of pancreatic beta cells, as evidenced by the first and second phases of the insulin response and the maximum secretory activity of beta cells. Pharmacodynamic studies in patients with type 2 diabetes mellitus showed restoration of the first phase of insulin secretion (intravenous insulin), improvement of the second phase of insulin secretion (hyperglycemic clamp test) and maximum insulin secretory activity (arginine stimulation test).
During 52 weeks of therapy with Victoza®, there was an improvement in pancreatic beta cell function, which was confirmed by assessment of the homeostatic model of pancreatic beta cell function (HOMA index) and the insulin to proinsulin ratio.
Glucagon secretion
The drug Victoza®, by stimulating insulin secretion and suppressing glucagon secretion, reduces the concentration of glucose in the blood. The drug Victoza® does not suppress the glucagon response to low glucose concentrations. In addition, with the drug Victoza®, lower production of endogenous glucose was observed.
Gastric emptying
The drug Victoza® causes a slight delay in gastric emptying, which leads to a decrease in the rate of postprandial glucose entering the blood.
Body weight, body composition and energy expenditure
In overweight subjects included in long-term clinical studies of Victoza®, the latter caused a significant reduction in body weight. Computed tomography (CT) and dual-energy X-ray absorptiometry (DXA) scans showed that the weight loss was primarily due to the loss of fat tissue in the patients. These results are explained by the fact that during therapy with Victoza®, patients experience a decrease in hunger and energy expenditure.
Cardiac electrophysiology (ECP)
The effect of the drug Victoza® on the process of repolarization in the heart was tested in the EFS study. The use of the drug Victoza® at equilibrium concentration in a daily dose of up to 1.8 mg does not prolong the corrected QT interval.
Clinical effectiveness
3992 patients with type 2 diabetes mellitus were randomized in 5 double-blind clinical safety and efficacy studies designed to evaluate the effect of Victoza® on glycemic control. Treatment with Victoza® caused clinically and statistically significant improvements in HbA1C, fasting glucose and postprandial glucose compared to placebo. These studies included 3978 treated patients (2501 patients treated with Victoza®), 53.7% men and 46.3% women, 797 patients (508 treated with Victoza®) were aged ≥ 65 years, 113 patients ( 66 received therapy with Victoza®) age was ≥ 75 years.
Glycemic control
The drug Victoza® in the form of monotherapy for 52 weeks caused a statistically significant (p < 0.0014) and long-lasting decrease in HbA1C compared with the same indicator in patients receiving glimepiride therapy. At the same time, the noted decrease in HbA1C below 7% persisted for 12 months (Fig. 2).
In patients with HbA1C above 9.5% at baseline, this indicator decreased by 2.1% during monotherapy with Victoza®, while in patients participating in clinical trials of the combined use of Victoza®, the average HbA1C decreased by 1.1-2.5%.
Victoza®, during 26 weeks of combination therapy with metformin, sulfonylureas or metformin and a thiazolidinedione, caused a statistically significant (p < 0.0001) and long-lasting decrease in HbA1C compared with that in patients receiving placebo.
In patients who did not achieve adequate glycemic control on Victoza® and metformin therapy, the addition of insulin detemir provided greater efficacy compared with Victoza® and metformin therapy after 26 weeks of treatment (0.52% reduction in HbA1C).
It has been proven that the effectiveness of Victoza® at a dose of 0.6 mg in combination with sulfonylureas or metformin is superior to placebo, but at the same time lower compared to doses of 1.2 mg and 1.8 mg.
Proportion of patients who achieved a decrease in HbA1C
During the 52-week study, during the 52-week study, the number of patients achieving HbA1C < 7% increased statistically significantly (p ≤ 0.0007) compared to the number of patients receiving glimepiride. At week 26 of using the drug Victoza® in combination with metformin, sulfonylurea drugs or a combination of metformin with a thiazolidinedione, the number of patients who achieved HbA1C ≤ 6.5% increased statistically significantly (p ≤ 0.0001) in relation to the number of patients who received therapy with oral hypoglycemic drugs without the addition of Victoza®.
In groups of patients who did not achieve adequate glycemic control on therapy with Victoza® and metformin, the percentage of patients who achieved the target HbA1C (< 7% and ≤ 6.5%) was significantly higher during therapy with insulin detemir + liraglutide 1.8 mg + metformin, compared with liraglutide 1.8 mg + metformin therapy (p ≤ 0.0001 / p = 0.0016).
During a 26-week combination study of Victoza®, it was possible to achieve HbA1C < 7% in more patients receiving the drug as combination therapy compared to the number of patients receiving it as monotherapy.
Use in patients with impaired renal function
In a double-blind study of the efficacy and safety of Victoza® 1.8 mg compared with placebo as an adjunct to insulin and/or oral antihyperglycemic agents in patients with type 2 diabetes mellitus and moderate renal impairment, Victoza® was more effective in reducing HbA1C level after 26 weeks (-1.05% versus -0.38%, p < 0.0001). A significantly larger number of patients achieved an HbA1C value of less than 7% when using the drug Victoza® compared to using placebo (52.8% compared to 19.5%; p < 0.0001). Patients receiving Victoza® showed a statistically significant decrease in body weight compared to patients receiving placebo (-2.41 kg versus -1.09 kg, p = 0.0052). The risk of developing hypoglycemic episodes was comparable between the two treatment groups. The safety profile of Victoza® was generally similar to that observed in other studies of Victoza®.
Fasting blood glucose level
Fasting glucose concentration decreased by 13-43.5 mg% (0.72-2.42 mmol/l) with the use of the drug Victoza®, both as monotherapy and in combination with one or two oral hypoglycemic drugs. This decrease was observed already within the first two weeks of treatment.
Postprandial glycemic level
When using the drug Victoza®, a decrease in the concentration of postprandial glucose after each of three daily meals was observed by 31-49 mg% (1.68-2.71 mmol/l).
Body mass
52-week monotherapy with Victora® was associated with sustained weight loss.
Throughout the clinical study period, sustained weight loss was also associated with the use of Victoza® in combination with metformin and in combination with the combination of metformin with sulfonylurea derivatives or the combination of metformin with a thiazolidinedione.
Weight loss in patients receiving Victoza® in combination with metformin was also observed after the addition of insulin detemir.
The greatest reduction in body weight was observed in patients who had an increased body mass index (BMI) at the starting point of the study.
Monotherapy with Victoza® for 52 weeks caused a decrease in average waist circumference by 3.0-3.6 cm.
Weight loss was observed in all patients treated with Victoza®, regardless of whether or not they experienced an adverse reaction in the form of nausea.
The drug Victoza® as part of combination therapy with metformin reduced the volume of subcutaneous fat by 13 - 17%.
Non-alcoholic steatohepatosis
The drug Victoza® reduces the severity of steatohepatosis in patients with type 2 diabetes mellitus.
Immunogenicity
Considering the possibility of immunogenic effects of protein and peptide drugs, the use of Victoza® in patients may lead to the formation of antibodies to liraglutide. Antibody formation is observed in an average of 8.6% of patients. The formation of antibodies does not lead to a decrease in the effectiveness of the drug Victoza®.
Assessment of the effect on the cardiovascular system
Long-term clinical studies have shown that Victoza® reduces systolic blood pressure by an average of 2.3-6.7 mm Hg. in the first two weeks of treatment. The drug Victoza® reduced the incidence of metabolic syndrome in accordance with the definition of the III report of the expert group on the treatment of adults (ATPIII). The decrease in systolic blood pressure occurred before the decrease in body weight.
In a retrospective analysis of serious cardiovascular adverse events (cardiovascular death, myocardial infarction, stroke) from all long-term and intermediate-duration phase II and III studies (26 to 100 weeks), including 5607 patients (3651 patients received Victoza®), there was no increase in cardiovascular risk (incidence ratio ratio 0.75 (95% CI 0.35, 1.63) for the combined endpoint with Victoza® compared with all comparator drugs (metformin, glimepiride, rosiglitazone, insulin glargine, placebo)). Patients at high cardiovascular risk were excluded from the studies and the incidence of serious cardiovascular events in the studies was low (6.02 per 1000 patient-years in patients receiving Victoza® and 10.45 in patients receiving all comparators), which prevents drawing clear conclusions.
Other clinical data
In an open-label study comparing the efficacy and safety of Victoza® at a dose of 1.8 mg and lixisenatide at a dose of 20 mcg in 404 patients with unsatisfactory glycemic control during metformin therapy (mean HbA1C 8.4%), Victoza® was more effectively reduced HbA1C levels compared to lixisenatide after 26 weeks of therapy (-1.83% versus -1.21%, p < 0.0001). Significantly more patients achieved an HbA1C value of less than 7% with Victoza® compared with lixisenatide (74.2% versus 45.5%, p < 0.0001), as well as a target HbA1C value of 6.5% or less (54.6% vs. 26.2%, p < 0.0001). A significantly greater reduction in fasting plasma glucose concentrations was achieved with Victoza® compared to lixisenatide (-2.85 versus -1.70 mmol/L, p < 0.0001). A decrease in body weight was noted in both treatment groups (-4.3 kg with Victoza® and -3.7 kg with lixisenatide). The safety profile of Victoza® and lixisenatide was generally comparable. No new safety information has been identified with the use of Victoza®.
In a comparative study of the effectiveness and safety of the drug Victoza® (at doses of 1.2 mg and 1.8 mg) and the dipeptidyl peptidase-4 inhibitor sitagliptin at a dose of 100 mg in patients who did not achieve adequate control on metformin therapy, after 26 weeks of treatment, a better reduction was proven HbA1C indicator when using the drug
Victoza® at both doses compared with sitagliptin (- 1.24%, - 1.50% compared with - 0.90%, p < 0.0001). Significantly more patients achieved HbA1C levels below 7% with Victoza® compared to sitagliptin (43.7% vs. 56.0% vs. 22.0%, p < 0.0001). Weight loss in patients receiving Victoza® was significantly greater compared to patients receiving sitagliptin (-2.9 kg and -3.4 kg versus -1.0 kg, p < 0.0001). Compared with patients receiving sitagliptin, patients receiving Victoza® were more likely to experience nausea. However, the nausea was transient. The incidence of mild hypoglycemia was not significantly different between treatment with Victoza® and sitagliptin (0.178 and 0.161, compared with 0.106 cases/patient per year). The reduction in HbA1C and the advantage of Victoza® compared to sitagliptin, observed after 26 weeks of treatment with Victoza® (1.2 mg and 1.8 mg), persisted after 52 weeks of treatment (- 1.29% and - 1.51% compared to - 0.88%, p < 0.0001). After 52 weeks of sitagliptin use, patients were switched to Victoza®, which led to an additional and statistically significant decrease in HbA1C at 78 weeks of treatment (0.24% and 0.45%, 95 CI: 0.41 to 0. 07 and -0.67 to 0.23), but no control group of patients was available.
In a comparative study of the effectiveness and safety of Victoza® (at a dose of 1.8 mg) and exenatide (at a dose of 10 mcg twice a day) in patients who did not achieve adequate control on therapy with metformin and/or sulfonylurea derivatives, after 26 weeks of use of the drug Victoza® showed a greater decrease in HbA1C compared to exenatide (- 1.12% versus - 0.79%, p < 0.0001). Significantly more patients achieved HbA1C levels below 7% with Victoza® compared to exenatide (54.2% versus 43.4%, p = 0.0015). Both treatments showed an average weight loss of approximately 3 kg. The number of patients reporting nausea was lower in the group of patients receiving Victoza® compared to exenatide. The incidence of mild hypoglycemia was significantly lower in the group of patients receiving Victoza® compared to exenatide (1.932 versus 2.600 events/patient year, p=0.01). After 26 weeks of using exenatide, patients were switched to Victoza®, which led to an additional decrease in HbA1C at week 40 of treatment (- 0.32%, p < 0.0001), with 13% of patients achieving an HbA1C lower 7%.
Treatment with Victoza® for 52 weeks improved insulin sensitivity compared with that of sulfonylureas, as determined by the HOMA-IR homeostatic model for assessing insulin resistance.
Effect of liraglutide on body weight of patients with T2DM
Various studies have shown that liraglutide leads to a significant reduction in body weight, both as monotherapy and as part of combination therapy, compared with glitazones and insulin glargine, which traditionally cause weight gain (Fig. 12).
Weight loss occurred in the first 16 weeks of treatment and was maintained at the achieved level throughout the year of treatment. The decrease in weight was more pronounced the higher the initial body mass index (from 2 to 7 kg per year). Body weight loss occurred mainly due to visceral fat, which was confirmed by both a decrease in waist circumference (-3-3.6 cm) and a study of body composition using computed tomography.
Treatment with liraglutide in a comparative study with sitagliptin was also accompanied by a more significant decrease in body weight: -3.38 kg and -2.86 kg for dosages, respectively, of 1.8 mg and 1.2 mg, compared with -0.96 kg for sitagliptin.
The high effectiveness of liraglutide in reducing body weight suggests the possibility of its use in the future for the treatment of obesity (the drug is currently registered only for the treatment of T2DM).
Note!
Description of the drug Victoza solution d/in. 6 mg/ml cart. 3ml syringe pen No. 2 on this page is a simplified author’s version of the apteka911 website, created on the basis of the instructions for use.
Before purchasing or using the drug, you should consult your doctor and read the manufacturer's original instructions (attached to each package of the drug). Information about the drug is provided for informational purposes only and should not be used as a guide to self-medication. Only a doctor can decide to prescribe the drug, as well as determine the dose and methods of its use.
Effect of liraglutide on the cardiovascular system
A number of studies have shown that liraglutide “inherited” from GLP-1 not only the glucose-lowering effect, but also cardioprotective properties. The studies noted a significant decrease in systolic blood pressure, which was observed approximately 2 weeks from the start of treatment and reached a maximum of -6.6 mm Hg. Art. at a dose of 1.2 mg and -5.5 mmHg. Art. at a dose of 1.8 mg (Fig. 13).
The antihypertensive effect of the drug is probably associated with a vasodilatory effect due to stimulation of the production of endothelial nitric oxide synthase (NOS). A hypothesis has also been put forward about the natriuretic or diuretic effect of the drug.
In phase II clinical studies, the highest dose reduced levels of three cardiovascular risk biomarkers (triglycerides, plasminogen activator inhibitor-1, and B-type natriuretic peptide), supporting a direct cardioprotective effect of liraglutide.
Effect of liraglutide on β-cell mass and function
To date, the only way to assess the functional activity of beta cells in vivo is the HOMA-B homeostasis model assessment model: using a special formula, the ratio of fasting glucose and plasma insulin levels is calculated.
According to a series of studies, the use of liraglutide was accompanied by a significant increase in HOMA-B by 40-71%, as well as a change in the proinsulin/insulin ratio, which may indirectly reflect the drug’s ability to restore the functional activity of pancreatic beta cells.
- Improvement in β-cell function, as assessed by the HOMA-B index, was significantly greater with liraglutide at both doses compared with placebo and rosiglitazone and comparable to that with glimepiride.
- Liraglutide at a dose of 1.8 mg once caused a significantly greater increase in the HOMA-B index (by 32%) compared with exenatide at a dose of 10 mcg twice a day (by 3%).
- In a 26-week, randomized, open-label study of liraglutide versus sitagliptin in combination with metformin in patients with type 2 diabetes, improvement in β-cell function as measured by HOMA-B was significantly greater with liraglutide at both doses compared with sitagliptin.
Safety of use and side effects of GLP-1 analogues
The most commonly reported side effects when taking liraglutide are gastrointestinal. In the LEAD studies, the incidence of nausea ranged from 11 to 29% (with liraglutide monotherapy it was 27%). Nausea was transient and almost completely disappeared after 12 weeks of treatment. The dose of liraglutide did not affect the frequency and severity of nausea. Nausea was significantly less severe with liraglutide compared with exenatide.
- The incidence of hypoglycemic events on liraglutide is 0.03 events per year at the 1.2 mg dose, 0.09 events per year at the 1.8 mg dose, which is lower than that observed in patients on placebo (0.13 events per year), and significantly lower than with glimepiride (1.23 events per year). Only in combination of liraglutide with SM drugs may the frequency of hypoglycemic conditions increase, which must be taken into account when prescribing these drugs in combination. To avoid hypoglycemia in this case, the dose of SM must be reduced.
- These data suggest that treatment with liraglutide will maintain satisfactory long-term glycemic control because there will be no escape effect from the drug due to antibody formation.
- These values do not exceed the incidence of pancreatitis in the general healthy population and are significantly lower than in the general population of patients with type 2 diabetes.
Indications for use of the drug liraglutide in patients with type 2 diabetes
- Patients with T2DM with overweight or obesity who do not achieve therapeutic goals on traditional PSSP (HbA1c > 7%);
- Patients with type 2 diabetes who are unable to strictly adhere to the diet (the drug can be administered during the day at any time, regardless of food intake);
- Patients with T2DM who prefer a single dose of the drug;
- Patients with T2DM at high risk of hypoglycemia;
- As a step prior to the prescription of insulin therapy, in the absence of severe decompensation of diabetes (HbA1c level <8.0-8.5%), if weight loss is the desired goal.
Storage conditions
Keep out of the reach of children.
Store in the refrigerator (2°C - 8°C) away from the freezer. Do not freeze.
After first use, store at temperatures below 30°C or in the refrigerator (2°C - 8°C). Do not freeze.
To prevent exposure to light, store the pen with the cap closed.
Shelf life: 30 months.
Product description certified by the manufacturer Novo Nordisk
.
Verified by
Likar Turumkulova Irina
Liraglutide: achieving comprehensive diabetes treatment goals
- Liraglutide has an effect similar to human GLP-1: against the background of hyperglycemia, it stimulates insulin secretion and suppresses glucagon secretion, and at normal or low glycemia these effects are not observed. This mechanism helps prevent the development of hypoglycemic conditions.
- Liraglutide also improves β-cell function, slows gastric emptying and reduces postprandial hyperglycemia, accelerates satiety, and has beneficial cardiovascular effects.
- The use of the drug liraglutide leads to a significant reduction in body weight both in monotherapy and as part of combination therapy. Weight loss occurs in the first weeks of treatment and is maintained at the achieved level throughout the year of treatment. The higher the initial body mass index, the more pronounced the weight loss. Body weight loss occurs mainly due to visceral fat.
- A meta-analysis of these studies showed that the addition of liraglutide injections to previous antihyperglycemic therapy resulted in a reduction in HbA1c levels by 1.26-1.36%, thus setting the average HbA1c endpoint at 6.96-7.05%. At the same time, the proportion of patients who achieved the target HbA1c level <7% during combination therapy with liraglutide was 71% (Fig. 14).
- A meta-analysis of LEAD studies showed the following advantages of liraglutide in comparison with representatives of all classes of hypoglycemic drugs: the odds ratio of achieving control of HbAlc and body weight without hypoglycemia for liraglutide is 2.0 - 10.3 times higher than in patients receiving comparator drugs. All results are statistically significant.
- Thus, with the use of the drug liraglutide, the percentage of patients who manage to achieve control of HbA1c, body weight and SBP is higher than with therapy with any comparison drugs (Fig. 15).
Sources:
- Ametov AS First GLP-1 analog liraglutide: the result of clinical trails on efficacy / AS Ametov, LL Kamynina // Diabetes Mellit. – 2011. – T. – No. 4 – 39 p.
- Shestakova M.V. LIRAGLUTIDE POSSIBILITIES OF AN INTEGRATIVE THERAPEUTIC APPROACH IN THE THERAPY OF TYPE 2 DM / Shestakova M.V. // Diabetes mellitus – 2009. – No. 5.