13 May 2020
185258
3
3.9 out of 5
Sciatica is sometimes also called lumbosacral radiculitis - a chronic neurological disease in which the sciatic nerve passing through the buttock and leg is compressed. This is accompanied by severe pain and a number of other disorders. It can occur at any age in people of both sexes, often occurs in pregnant women, but is most often diagnosed in people 40–60 years old. Although sciatica is not life-threatening, it can significantly reduce the quality of life and deprive a person of ability to work. Therefore, when the first signs appear, you should contact a neurologist and begin treatment immediately. In this case, it will be as easy as possible, effective and will allow you to quickly eliminate both the signs of the disease and the causes of its occurrence.
What is sciatica
Sciatica is a non-inflammatory disease that occurs due to compression of the sciatic nerve in any area. The concept of “sciatic nerve sciatica” is not used either in the literature or in everyday life, since the term “sciatica” is used exclusively to describe cases of compression of the sciatic nerve and no other.
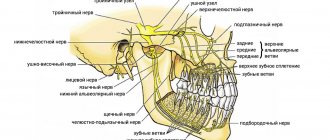
The sciatic nerve itself is paired and is one of the largest nerves in the human body. Its two branches begin at the sacral nerve plexus, located in close proximity to the vertebrae and sacrum, and run symmetrically along the buttocks, down the back of the thighs and reaching the legs.
The sacral nerve plexus is formed by closely intertwined nerves that run along both sides of the spine from its outer side.
In the upper part of the leg, the sciatic nerve is divided into 2 large branches: the peroneal and tibial. They pass along the back of the lower leg on the right and left.
Thus, the sciatic nerves are quite long, so sciatica can be caused by a huge variety of different causes. And depending on the area where the nerve fiber was compressed, there are 3 types of sciatica:
- upper – the cord or spinal roots at the level of the lumbar vertebrae of the spine are subjected to compression;
- middle (plexitis) – the sciatic nerve is pinched in the area of the sacral nerve plexus;
- lower - pinched nerve fiber is observed in any part along its entire length from the buttock to the foot.
Most often, it is lower sciatica, which is often called neuritis. But since the latter term describes an inflammatory lesion of the nerve, its use as a synonym for sciatica is not entirely correct. Indeed, with sciatica, pain is caused solely by compression of a nerve in one area or another, while with neuritis it can be involved in the inflammatory process or be pinched by hyperemic tissues.
You should not let the course of the disease take its course. Non-intervention and ignoring the symptoms of sciatica is fraught with changes in the lower extremities, which can ultimately lead to loss of performance and the ability to care for oneself independently.
How to make a diagnosis
The disease is determined by a neurologist based on the results of motor tests that reveal the presence of the syndromes described above. But laboratory and instrumental studies are still necessary. As a rule, they are limited to x-rays in two planes. It may be necessary to obtain a more clear picture of the condition of the spine. In this case, a tomography will be prescribed. A radioisotope scan is done if a tumor is suspected.
When a person has inflammation of the sciatic nerve, treatment at home is not always acceptable, because the disease can manifest itself in such a serious form that the patient is prescribed bed rest in a hospital setting. Nerve-related illnesses must be taken seriously or you may lose your ability to move.
An immediate visit to a doctor is necessary in the following cases:
- severe numbness that prevents you from moving;
- increased body temperature;
- transfer of pain to other locations;
- incontinence of metabolic products;
- swelling in the lower part of the ridge.
Causes
Compression of the sciatic nerve can occur in a variety of different cases. This can occur due to injuries to the legs, pelvis and back, during pregnancy, prolonged immobility, pinched nerves by fibrous cords or neoplasms, etc.
Most often, sciatica becomes a complication of various spinal diseases, including:
- lumbar osteochondrosis - degeneration of large intervertebral discs of the lumbar spine is the main prerequisite for the development of other spinal diseases and pinching of nerve fibers of different sizes;
- the formation of intervertebral hernias is the most common complication of osteochondrosis, manifested by protrusion of the disc, which leads to compression and damage to the spinal roots;
- spondylolisthesis – displacement of the vertebrae relative to the underlying one by different amounts, which can provoke pinching of the nerve roots;
- facet syndrome - nerve fibers are pinched in the narrow natural openings of the spine as a result of deformation of the vertebrae, the formation of osteophytes, or other disorders.
Another common cause of sciatica is spasm of the piriformis muscle located in the buttock. Since the sciatic nerve passes through it, an increase in its tone leads to stretching and irritation of the nerve fiber, which immediately results in severe pain.
Other prerequisites for the development of sciatica include:
- excessive physical activity;
- spinal tumors of various natures from hemangiomas to malignant neoplasms;
- arthritis;
- thrombosis of blood vessels;
- hypothermia and the development of inflammatory processes in anatomical structures adjacent to the spine at the level of the lumbosacral region;
- infectious gynecological and other diseases, including influenza, tuberculosis, typhoid fever, sepsis (released toxins affect the sheath of the sciatic nerve);
- spinal deformities (scoliosis, etc.).
Why does pathology occur?
Doctors consider primary and secondary neuropathy. The primary cause is injuries, infectious diseases and hypothermia. The list of reasons that can cause a secondary type of illness is much more extensive. These include:
- disc displacement;
- neoplasms of any nature;
- osteochondrosis;
- protrusion;
- osteophytes;
- spasmodic muscles;
- curvature of the ridge;
- tunnel syndrome;
- intervertebral hernia;
- post-injection suppuration.
Symptoms
As a rule, the development of sciatica occurs gradually. The first signs are of a mild discomfort and are often perceived by people as a manifestation of banal fatigue after performing physical work. Initially, there may be slight pain in the lumbar region, which radiates to the buttock. In this case, slight discomfort occurs in the leg along the back of the thigh.
The belief of patients that such symptoms are a consequence of overwork and the fact that they occur mainly after physical exertion and disappear without a trace after a short rest are rooted. This condition can persist for several years and is already perceived by the patient as normal.
But sooner or later, lifting an object that is too heavy, hypothermia, or simply careless movement provokes an attack. A person is constrained by pain. It interferes with normal mobility and is often accompanied by autonomic and neurological symptoms.
A specific symptom of sciatica is unilateral pain affecting only one of the buttocks and one leg. As a result of the progression of pathological changes, it increasingly differs in functionality and even appearance from a healthy leg: it is cold to the touch, smaller than healthy, the skin is pale and dry.
The nature of the disorders directly depends on which of the fibers of the sciatic nerve are affected as a result of infringement: motor or sensory. Thus, patients may suffer from:
- decreased sensitivity of the skin of the affected lower limb; sometimes, on the contrary, there is increased sensitivity of the outer edge of the foot;
- muscle weakness in the legs and feet;
- changes in tissue nutrition, which leads to pale skin and thinning;
- disorders of the pelvic organs, which may be accompanied by loss of control over the process of urination and defecation;
- bowel dysfunction, etc.
Sciatica typically has a paroxysmal course with periodic exacerbations.
Manifestations of the disease may vary in intensity and nature. In some cases, acute pain comes to the fore, in others, patients will complain more about limited mobility or other symptoms, mentioning pain only in passing. Thus, sciatica can manifest itself in varying degrees of pain, motor, sensory and neurological impairment. Let's take a closer look at each group of symptoms separately.
Sciatica pain
The nature of pain when the sciatic nerve is pinched can be different. During an attack they are sharp, powerful, burning and shooting. Patients describe them as being struck with a knife or electric shock. Literally any movement or change in body position is extremely painful, and bending or sitting leads to a sudden aggravation of the pain syndrome. Often the pain does not subside even when lying down.
With chronic sciatica, the pain may not be so severe. They are often nagging, aching, present constantly or appear after physical activity. Just as with an attack, they tend to get worse during bending, lifting a leg, or prolonged sitting or standing.
With sciatica, the epicenter of pain is in the lumbosacral spine or directly in the area where the sciatic nerve is pinched. But a typical feature of the disease is the spread of pain along the nerve, i.e., along the buttock, back of the thigh, lower leg, and sometimes even to the toes. To reduce pain, a person takes a forced body position. He leans forward and to the side.
When you try to turn the affected leg bent inward at the hip and knee, a sharp pain occurs in the buttock.
Motor and sensory disorders
The sciatic nerve is formed by sensory and motor fibers. It is responsible for providing sensitivity and mobility to the muscles of the back of the legs. Therefore, when it is compressed, both motor and sensory disorders may occur. They can manifest themselves in varying degrees, be combined with pain or be isolated. In most cases, one or more of the following symptoms are present. Combinations can be different, so different patients with sciatica rarely have the same clinical picture:
- decreased sensitivity of the skin along the lateral and posterior surface of the lower leg and throughout the entire foot;
- the presence of tingling, numbness, goosebumps;
- violations of flexion and extension of the muscles of the back of the thigh and lower leg, which negatively affects the work of the knee and ankle joints and, accordingly, gait (it seems that a person does not bend his leg at all when walking);
- difficulties when bending;
- weakness in the foot, which can literally hang completely motionless on the shin;
- reduction in muscle size due to their gradual atrophy;
- complete paralysis of the muscles of the foot and the back of the thigh and lower leg (with severe sciatica);
- dryness, peeling, thinning, paleness or, conversely, redness of the skin of the lower extremities;
- increased sweating;
- thinning and brittle toenails.
Over time, it becomes increasingly difficult for the patient to walk, since the affected leg loses stability and cannot fully perform its supporting function. There is progressive weakness and lameness.
Impaired nerve conduction can lead to insufficient tissue trophism, which can result in osteoporosis. In such cases, fractures often occur, even under the influence of factors that are normally unable to disrupt the integrity of the bones.
Osteoporosis is a disease in which bone tissue becomes porous, loses its normal strength and becomes brittle.
Symptoms - neurological manifestations
Since the sciatic nerve is pinched in one place or another, this is accompanied by impaired conduction of nerve impulses and a decrease in the intensity or complete loss of reflexes. It is the presence of such symptoms that most often helps a neurologist make the correct diagnosis.
With sciatica, the following are practically not manifested or are completely absent:
- Achilles tendon reflex - a blow with a hammer or the edge of the palm to the Achilles tendon when a person takes a lying position on his stomach normally provokes the foot to move back to a position as if the person is standing on tiptoes;
- knee reflex - hitting a point under the knee with a hammer or the edge of the palm normally leads to extension of the knee joint if a person sits on the edge of the bed with his legs hanging freely;
- plantar reflex - passing the tip of a milk or any other blunt object along a relaxed foot from the heel to the toes provokes its flexion.
Also a clear neurological sign of sciatica is the occurrence of severe pain in the lower back, buttock and thigh when trying to lift a straight leg while lying on your back. When bending the leg, its intensity decreases.
In addition, at some points the sciatic nerve runs very close to the skin: in the subgluteal fold, the back of the knee, the center of the lower leg and in the area of the Achilles tendon. Such points are called Vallee points. Therefore, pressing on them provokes an attack of pain in the presence of sciatica.
Sciatic nerve neuropathy. Piriformis syndrome
Diseases of the peripheral nervous system are one of the most common causes of disability in patients of working age. In the structure of these diseases, pain syndromes occupy a predominant place (N. N. Yakhno, 2003; G. R. Tabeeva, 2004). The reasons for the development of neuropathic pain syndrome can be different: diabetes mellitus, paraneoplastic processes, HIV, herpes, chronic alcoholism (A. M. Vein, 1997; I. A. Strokov, A. N. Barinov, 2002).
When the peripheral nervous system is damaged, two types of pain are distinguished: dysesthesia and truncal. Superficial dysesthetic pain is usually observed in patients with predominant damage to small nerve fibers. Truncal pain occurs with compression of the spinal roots and tunnel neuropathies.
In patients with this type of pain syndrome, it is impossible to choose the optimal treatment strategy without identifying the pathophysiological mechanisms. Therefore, when determining treatment tactics, it is necessary to take into account the localization, nature and severity of clinical manifestations of pain.
Compression-ischemic (tunnel) neuropathy refers to non-inflammatory lesions of the peripheral nerve that develop under the influence of compression or ischemic influences.
In the area of compression of the corresponding nerve, painful compactions or thickening of tissue are often found, leading to a significant narrowing of the musculoskeletal sheaths through which the neurovascular trunks pass.
Currently, many variants of compression neuropathies are known. Their clinical picture consists of three syndromes: vertebral (in cases where the factor of the same name is involved), neural peripheral, reflex-myotonic or dystrophic. Vertebral syndrome at any stage of exacerbation, and even in remission, can cause changes in the walls of the “tunnel”. The myodystrophic focus, acting as a implementing link, causes neuropathy against the background of its clinical peak. The neurological picture of compression neuropathies consists of symptoms of damage of varying severity in the corresponding myo- and dermatomes. The diagnosis of compression neuropathies is made in the presence of pain and paresthesia in the area of innervation of this nerve, motor and sensory disorders, as well as pain in the area of the receptors of the corresponding channel and Tinel’s vibration symptom. If there are difficulties in diagnosis, electroneuromyographic studies are used: lesions of the peripheral neuron corresponding to a given nerve are determined, and the degree of decrease in the speed of impulse transmission along the nerve distal to the place of its compression. Piriformis syndrome is the most common tunnel neuropathy. Pathological tension of the piriformis muscle due to compression of the L5 or S1 root, as well as with unsuccessful injections of medicinal substances, leads to compression of the sciatic nerve (or its branches at high origin) and the accompanying vessels in the infrapiriformis space.
To choose the right treatment strategy, it is necessary to clearly know the main clinical symptoms of damage to a particular area. The main clinical manifestations of damage to the nerves of the sacral plexus:
- compression of nerves in the pelvis or above the gluteal fold;
- piriformis syndrome;
- damage to the sciatic nerve below the exit from the pelvis (at the level of the hip and below) or damage to the sciatic nerve in the pelvic cavity;
- sciatic nerve syndrome;
- tibial nerve syndrome;
- syndrome of the piriformis, internal obturator nerves and quadratus femoris nerve;
- superior gluteal nerve syndrome;
- inferior gluteal nerve syndrome.
The most difficult in terms of diagnosis are lesions in the pelvic area or above the gluteal fold - due to the presence of somatic or gynecological pathology in patients. Clinical symptoms of lesions in the pelvis or above the gluteal fold consist of the following types of disturbances of motor and sensory functions.
- Decrease and loss of function n. peroneus and n. tibialis communis, paralysis of the foot and fingers, loss of the Achilles and plantar reflexes, hypoesthesia (anesthesia) of the leg and foot.
- Reduction or loss of function of the biceps femoris, semimembranosus and semitendinosus muscles, leading to impaired flexion of the leg.
- Reduction or loss of function of the posterior cutaneous nerve of the thigh, leading to hypoesthesia (anesthesia) along the posterior surface of the thigh.
- Difficulty in external rotation of the hip.
- Presence of positive symptoms in Lasegue, Bonnet.
- The presence of vasomotor and trophic disorders (hypo-, hyperhidrosis, formation of trophic ulcers in the heel and outer edge of the foot, changes in nail growth, hypo- and hypertrichosis).
Damage to the sciatic nerve at the level of the infrapiriform foramen can be observed in two variants:
- damage to the trunk of the sciatic nerve itself;
- piriformis syndrome.
Compression of the sciatic nerve and adjacent vessels is characterized by the following clinical manifestations: a feeling of constant heaviness in the leg, dull, “cerebral” pain. There is no increase in pain when coughing or sneezing. There is no atrophy of the gluteal muscles. The zone of hypoesthesia does not extend above the knee joint.
Piriformis syndrome occurs in at least 50% of patients with discogenic lumbosacral radiculitis. If the patient is diagnosed with this, the assumption of the presence of piriformis muscle syndrome may arise in the presence of persistent pain along the sciatic nerve that does not decrease with drug treatment. It is much more difficult to determine the presence of this syndrome if there is only pain in the buttock area, which is limited in nature and associated with certain positions (movements) of the pelvis or when walking. Piriformis muscle syndrome is often recorded in gynecological practice. With piriformis syndrome it is possible:
- compression of the sciatic nerve between the altered piriformis muscle and the sacrospinous ligament;
- compression of the sciatic nerve by the altered piriformis muscle as the nerve passes through the muscle itself (a variant of the development of the sciatic nerve).
The clinical picture of piriformis syndrome consists of local symptoms and symptoms of compression of the sciatic nerve. Local includes aching, nagging, “braining” pain in the buttock, sacroiliac and hip joints, which intensifies when walking, standing, adducting the hip, and also in a squatting position; subsides somewhat when lying down and sitting with legs apart. With good relaxation of the gluteus maximus muscle, a dense and painful when stretched (Bonnet-Bobrovnikova symptom) piriformis muscle is felt underneath it. With percussion at the point of the piriformis muscle, pain appears on the back of the leg (Vilenkin's symptom). The clinical picture of compression of the vessels and the sciatic nerve in the infrapiriform space consists of the topographic-anatomical “relationship” of its tibial and fibular branches with the surrounding structures. Pain during compression of the sciatic nerve is dull, “brainy” in nature with a pronounced vegetative coloring (sensations of chilliness, burning, stiffness), with irradiation throughout the leg or mainly along the zone of innervation of the tibial and peroneal nerves. Provoking factors are heat, weather changes, and stressful situations. Sometimes the Achilles reflex and superficial sensitivity decrease. With the predominant involvement of the fibers from which the tibial nerve is formed, the pain is localized in the posterior group of muscles of the leg. Pain appears in them when walking, during the Lasègue test. Palpation reveals pain in the soleus and gastrocnemius muscles. In some patients, compression of the inferior gluteal artery and the vessels of the sciatic nerve itself is accompanied by a sharp transient spasm of the vessels of the leg, leading to intermittent claudication. The patient is forced to stop, sit down or lie down when walking. The skin of the leg turns pale. After resting, the patient can continue walking, but soon the same attack recurs. Thus, in addition to intermittent claudication with obliterating endarteritis, there is also infrapiriform intermittent claudication. An important diagnostic test is infiltration of the piriformis muscle with novocaine and assessment of the positive changes that occur. Reflex tension in the muscle and neurotrophic processes in it are caused, as a rule, by irritation not of the fifth lumbar, but of the first sacral root. Certain manual tests help recognize this syndrome.
- The presence of pain on palpation of the upper internal region of the greater trochanter of the femur (the place of attachment of the piriformis muscle).
- Pain on palpation of the lower part of the sacroiliac joint is a projection of the attachment site of the piriformis muscle.
- Passive adduction of the hip with simultaneous internal rotation (Bonnet-Bobrovnikova symptom; Bonnet symptom).
- A test to examine the sacrospinous ligament, which allows you to simultaneously diagnose the condition of the sacrospinous and iliosacral ligaments.
- Tapping the buttock (on the sore side). This causes pain that spreads along the back of the thigh.
- Grossman's sign. When struck with a hammer or folded fingers on the lower lumbar or upper sacral spinous processes, the gluteal muscles contract.
Since painful tension of the piriformis muscle is most often associated with irritation of the first sacral root, it is advisable to alternately carry out novocaine blockade of this root and novocainization of the piriformis muscle. A significant reduction or disappearance of pain along the sciatic nerve can be considered a dynamic test showing that the pain is caused by the compressive effect of the spasmed muscle.
Sciatic nerve lesions
Lesions of the sciatic nerve below the exit from the pelvis (at the level of the hip and below) or in the pelvic cavity are characterized by the following signs.
- Impaired flexion of the leg at the knee joint (paresis of the semitendinosus, semimembranosus and biceps femoris muscles).
- Specific gait: the straightened leg is carried forward when walking (due to the predominance of the tone of the antagonist muscle of the quadriceps femoris).
- Straightening the leg at the knee joint is a contraction of the antagonist (quadriceps femoris muscle).
- Lack of active movements in the foot and fingers as a result of their paresis.
- Atrophy of paralyzed muscles, which often masks the pastiness of the limb.
- Hypoesthesia along the posterior surface of the leg, dorsum of the foot, sole and toes.
- Impaired muscle-articular sensitivity in the ankle joint and interphalangeal joints of the toes.
- Lack of vibration sensitivity in the area of the outer ankle.
- Pain along the sciatic nerve - at the Valle and Gar points.
- Positive Lasegue symptom.
- Reduction or disappearance of the Achilles and plantar reflexes.
- The presence of burning pain that intensifies when lowering the leg.
In addition to the clinical symptoms described above, the development of vasomotor and trophic disorders is likely: increased skin temperature on the affected leg. The lower leg and foot become cold and cyanotic. Hyperhidrosis or anhidrosis, hypotrichosis, and hyperkeratosis are often found on the sole. Changes in the color and shape of the nails, trophic disorders on the heel, dorsum of the toes, and the outer edge of the foot appear, a decrease in strength is recorded, as well as atrophy of the muscles of the foot and lower leg. The patient cannot stand on his toes or heels. The semitendinosus, semimembranosus, and biceps femoris strength tests can be used to determine initial sciatic nerve involvement.
Sciatic nerve syndrome (ischemic-compressive neuropathy of the sciatic nerve). Depending on the level (height) of the lesion, different variants of sciatic nerve syndrome are possible.
A very high level of damage (in the pelvis or above the gluteal fold) is characterized by: paralysis of the foot and toes, loss of the Achilles and plantar reflexes; anesthesia (hypoesthesia) of almost the entire lower leg and foot, except for zone n. sapheni; loss of function of the biceps femoris, semitendinosus, semimembranosus muscles; hypoesthesia (anesthesia) along the posterior surface of the thigh; inability to rotate the hip outward; the presence of positive symptoms of tension (Lasegue, Bonnet); the presence of vasomotor and trophic disorders (hyper- or hypotrichosis, hypo- or hyperhidrosis, changes in nail growth, the formation of trophic ulcers in the heel area and the outer edge of the foot).
A lesion at the level of the infrapiriformis foramen consists of two groups of symptoms - damage to the piriformis muscle itself and the sciatic nerve. The first group of symptoms includes: pain on palpation of the upper internal part of the greater trochanter of the femur (the place of attachment of the piriformis muscle to the capsule of this joint); pain on palpation in the lower part of the sacroiliac joint; Bonnet's symptom (passive adduction of the hip with its inward rotation, causing pain in the gluteal region, less often in the zone of innervation of the sciatic nerve); pain on palpation of the buttock at the point where the sciatic nerve exits from under the piriformis muscle. The second group includes symptoms of compression of the sciatic nerve and blood vessels. Painful sensations due to compression of the sciatic nerve are characterized by a feeling of constant heaviness in the leg, a dull, “cerebral” nature of the pain, no increase in pain when coughing and sneezing, as well as atrophy of the gluteal muscles; the hypoesthesia zone does not rise above the knee joint.
A lesion at the level of the hip (below the exit from the pelvis) and up to the level of division into the peroneal and tibial nerves is characterized by: impaired flexion of the leg at the knee joint; specific gait; lack of active movements in the foot and toes, which sag moderately; atrophy of paralyzed muscles that joins after 2–3 weeks, often masking the pastiness of the leg; hypoesthesia (anesthesia) on the posterior surface of the leg, dorsum of the foot, sole and toes; impairment of joint-muscular sensitivity in the ankle joint and interphalangeal joints of the toes; lack of vibration sensitivity on the outer ankle; pain along the sciatic nerve - at the points of Valle and Gar; positive Lasegue symptom; disappearance of the Achilles and plantar reflexes.
The syndrome of incomplete damage to the sciatic nerve is characterized by the presence of pain of a causalgic nature (“burning” pain, intensified when lowering the leg, provoked by a light touch); severe vasomotor and trophic disorders (for the first 2–3 weeks, the skin temperature on the affected leg is 3–5 °C higher (“hot skin”) than on the healthy leg, then the lower leg and foot become cold and cyanotic). Hyperhidrosis or anhidrosis, hypotrichosis, hyperkeratosis, changes in the shape, color and growth rate of nails are often found on the plantar surface. Sometimes trophic ulcers occur on the heel, the outer edge of the foot, and the dorsum of the toes. X-rays reveal osteoporosis and decalcification of the foot bones.
Initial sciatic nerve injury syndrome can be diagnosed by using tests to determine the strength of the semitendinosus and semimembranosus muscles.
Sciatic nerve syndrome most often appears as a result of damage to this nerve through the mechanism of tunnel syndrome when the piriformis muscle is involved in the pathological process. The trunk of the sciatic nerve can be affected by injuries, fractures of the pelvic bones, inflammatory and oncological diseases of the pelvis, lesions and diseases of the gluteal region, sacroiliac joint and hip joint. In sciatic nerve syndrome, the differential diagnosis often has to be made with discogenic compressive radiculitis LV-SII (Table).
Syndrome of the piriformis, internal obturator and quadratus femoris nerves. Complete piriformis, obturator internus, and quadratus femoris nerve syndrome is characterized by impaired lateral rotation of the hip. The syndrome of partial damage to this group of nerves can be diagnosed based on the use of tests to determine the range of motion and strength of the subject.
Superior gluteal nerve syndrome. Complete superior gluteal nerve syndrome is characterized by impaired abduction of the hip with partial impairment of hip rotation and difficulty maintaining an upright position of the torso. With bilateral paralysis of these muscles, it is difficult for the patient to stand (stands unsteadily) and walk (the so-called “duck walk” appears with waddling from side to side). Partial superior gluteal nerve syndrome can be identified with a gluteal strength test. Based on the degree of decrease in strength compared to the healthy side, a conclusion is made about partial damage to the superior gluteal nerve.
Inferior gluteal nerve syndrome. Complete inferior gluteal nerve syndrome is characterized by difficulty in straightening the leg at the hip joint, and in a standing position - difficulty in straightening a tilted pelvis (the pelvis is tilted forward, with compensatory lordosis observed in the lumbar spine). Difficulty getting up from a sitting position, climbing stairs, running, jumping. With prolonged damage to this nerve, hypotonia and hypotrophy of the gluteal muscles are observed. Partial inferior gluteal nerve syndrome can be diagnosed using a test to determine the strength of the gluteus maximus muscle. Based on the degree of decrease in the volume and strength of the indicated movement (and in comparison with the healthy side), a conclusion is made about the degree of dysfunction of the inferior gluteal nerve.
Treatment
Therapy of sciatic nerve neuropathy requires knowledge of the etiological and pathogenetic mechanisms of the development of the disease. Treatment tactics depend on the severity and rate of progression of the disease. Pathogenetic therapy should be aimed at eliminating the pathological process and its long-term consequences. In other cases, treatment should be symptomatic. Its goal is to prolong stable remission and improve the quality of life of patients. The main criterion for the optimal therapeutic effect on the patient is the combination of medicinal and non-medicinal methods. Among the latter, the leading ones are physiotherapeutic techniques and post-isometric relaxation methods.
If the function of the muscles of the pelvic girdle and lower limb is impaired, it is recommended to use one of the manual therapy techniques - post-isometric relaxation (PIR), i.e. stretching the spasmodic muscle to its physiological length after maximum tension. The basic principles of drug therapy for lesions of the peripheral nervous system are early initiation of treatment, pain relief, and a combination of pathogenetic and symptomatic therapy. Pathogenetic therapy is aimed primarily at combating oxidative stress, affecting the microvasculature, improving blood supply to the affected area, and relieving signs of neurogenic inflammation. For this purpose, antioxidant, vasoactive and nonsteroidal anti-inflammatory drugs (NSAIDs) are used. The complexity of drug therapy is associated in most cases with the intricate anatomical and physiological hierarchy of structures involved in the pathological process. This is partly due to the structure and functioning of the structures of the lumbosacral plexus. At the same time, the basic mechanism underlying the development of neuropathy is a clear correlation between compression and ischemia of the nerve and the development of oxidative stress.
Oxidative stress is an imbalance between the production of free radicals and the activity of antioxidant systems. The developed imbalance leads to increased production of compounds (neurotransmitters) released by damaged tissues: histamine, serotonin, ATP, leukotrienes, interleukins, prostaglandins, nitric oxide, etc. They lead to the development of neurogenic inflammation, increasing the permeability of the vascular wall, and also promote the release mast cells and leukocytes of prostaglandin E2, cytokines and biogenic amines, increasing the excitability of nociceptors.
Currently, clinical studies have appeared on the use of drugs that improve the rheological properties of blood and endothelium-dependent reactions of the vessel wall in patients with compression neuropathies. Drugs such as thioctic acid derivatives (thiogamma, thioctacid) and ginkgo biloba (tanakan) are successfully used to reduce the manifestations of oxidative stress. However, the use of drugs with a polyvalent mechanism of action (Cerebrolysin, Actovegin) is more pathogenetically justified.
The priority of using Actovegin is due to the possibility of its use for therapeutic blockades and its good compatibility with other drugs. For compression-ischemic neuropathies, both in the acute and subacute stages of the disease, it is advisable to use Actovegin, especially if there is no effect from other treatment methods. A drip of 200 mg of the drug is prescribed for 5 days, followed by a transition to oral administration.
In the mechanisms of development of diseases of the peripheral nervous system, an important place is occupied by hemodynamic disorders in the structures of the peripheral nervous system, ischemia, microcirculation disorders, energy exchange disorders in ischemic neurons with a decrease in aerobic energy exchange, ATP metabolism, oxygen and glucose utilization. Pathological processes occurring in nerve fibers during neuropathies require correction with vasoactive drugs. In order to improve microcirculation processes and activate metabolic and glycolysis processes in patients with tunnel neuropathies, Cavinton, Halidor, Trental, and Instenon are used.
Instenon is a combined drug with neuroprotective action, including a vasoactive agent from the group of purine derivatives, affecting the state of the ascending reticular formation and cortical-subcortical relationships, as well as the processes of tissue respiration under hypoxic conditions, physiological mechanisms of autoregulation of cerebral and systemic blood flow. For neuropathies, instenon is used intravenously, 2 ml in 200 ml of saline, for 2 hours, 5–10 procedures per course. Then oral administration of instenon forte continues, 1 tablet 3 times a day for a month. For neuropathies with sympathetic syndrome, the use of instenon 2 ml intramuscularly once a day for 10 days is indicated. For compression-ischemic (tunnel) neuropathies, a similar technique is used. This helps improve microcirculation and metabolism in the ischemic nerve. A particularly good effect is observed with the combined use of Actovegin (drops) and instenon (intramuscular injections or oral administration).
Halidor (bencyclane fumarate) is a drug with a wide spectrum of action, which is due to the blockade of phosphodiesterase, antiserotonin effect, and calcium antagonism. Halidor is prescribed in a daily dose of 400 mg for 10–14 days.
Trental (pentoxifylline) is used 400 mg 2-3 times a day orally or 100-300 mg intravenously in 250 ml of saline.
Prescribing combination drugs that include large doses of vitamin B, anti-inflammatory drugs and hormones is inappropriate.
NSAIDs remain the first-line drugs for pain relief. The main mechanism of action of NSAIDs is inhibition of cyclooxygenase (COX-1, COX-2), a key enzyme in the arachidonic acid metabolic cascade, leading to the synthesis of prostaglandins, prostacyclins and thromboxanes. Due to the fact that COX metabolism plays a major role in the induction of pain at the site of inflammation and the transmission of nociceptive impulses to the spinal cord, NSAIDs are widely used in neurological practice. There is evidence that 300 million patients take them (G. Ya. Schwartz, 2002).
All anti-inflammatory drugs have anti-inflammatory, analgesic and antipyretic effects, are able to inhibit the migration of neutrophils to the site of inflammation and platelet aggregation, and also actively bind to serum proteins. Differences in the action of NSAIDs are quantitative (G. Ya. Schwartz, 2002), but they determine the severity of the therapeutic effect, tolerability and the likelihood of side effects in patients. The high gastrotoxicity of NSAIDs, which correlates with the severity of their sanogenetic effect, is associated with indiscriminate inhibition of both isoforms of cyclooxygenase. In this regard, for the treatment of severe pain syndromes, including long-term ones, drugs are needed that have anti-inflammatory and analgesic effects with minimal gastrotoxic reactions. The most well-known and effective drug from this group is xefocam (lornoxicam).
Xefocam is a drug with a pronounced antianginal effect, which is achieved through a combination of anti-inflammatory and strong analgesic effects. It is today one of the most effective and safe modern analgesics, which has been confirmed by clinical studies. The effectiveness of oral administration according to the following regimen: 1st day - 16 and 8 mg; Days 2–4 - 8 mg 2 times a day, day 5 - 8 mg/day - for acute back pain has been reliably proven. The analgesic effect at a dose of 2–16 mg 2 times a day is several times higher than that of napraxen. For tunnel neuropathies, it is recommended to use the drug in a dose of 16–32 mg. The course of treatment is at least 5 days with a one-time daily procedure. It is recommended to use the drug Xefocam for the treatment of piriformis muscle syndrome according to the following method: in the morning - 8 mg intramuscularly, in the evening - 8-16 mg orally, for 5-10 days, which allows you to achieve a quick and accurate effect on the source of inflammation with complete anesthesia with minimal risk development of adverse reactions. It is possible to carry out regional intramuscular blockades in the paravertebral region, 8 mg per 4 ml of 5% glucose solution daily for 3–8 days. Symptomatic therapy is the method of choice for relieving algic manifestations. Most often, therapeutic blockades with anesthetics are used to treat tunnel neuropathies. Persistent pain lasting more than 3 weeks indicates a chronic process. Chronic pain is a complex therapeutic problem that requires an individual approach.
First of all, it is necessary to exclude other causes of pain, after which it is advisable to prescribe antidepressants.
M. V. Putilina , Doctor of Medical Sciences, Professor of Russian State Medical University, Moscow
Diagnostics
A neurologist diagnoses and treats sciatica. It is this specialist who should be contacted if any of the above symptoms occur. Already during the first appointment, based on the patient’s complaints and examination, the doctor may suspect compression of the sciatic nerve. But in order to find the most effective treatment, you need to find out why this happened. For this purpose, the patient is prescribed a set of studies, thanks to which the condition of the intervertebral discs, joints, bones, etc. can be assessed.
Therefore, as part of the diagnosis of sciatica and the causes of its occurrence, the following are used:
- X-ray of the sore leg, sacrum and lower back - the results of the study show the condition of the vertebrae and partly the intervertebral discs;
- MRI – provides comprehensive information about the condition of the intervertebral discs and spinal cord;
- CT is an informative method that allows you to detect pathologies of the sacrum and lumbar vertebrae;
- Electroneuromyography – provides data on the quality of transmission of nerve impulses to the muscles of the lower extremities and their contractility.
The most informative method for diagnosing diseases of the cartilage tissue from which intervertebral discs are formed, as well as pathologies of the spinal cord, is MRI. It is this method that allows you to thoroughly examine the discs, assess their size, position, and detect the slightest hernia and other disorders.
Diagnosis of sciatic nerve pain
Is your sciatic nerve hurting and you don’t know how to treat it? Seek medical help! Specialists at the CELT Pain Clinic will find out the cause that caused this disease and prescribe its effective treatment. Before starting it, our doctors examine the patient, check reflexes and determine skin sensitivity and collect anamnesis. In addition, it is prescribed:
- X-ray examination;
- CT scan;
- Magnetic resonance imaging.
If the presence of a tumor in the spine is suspected, a radioisotope diagnostic study is prescribed.
Conservative treatment of sciatica
One can hope for a lasting improvement in the condition and elimination of pain in the buttock, back of the thigh and lower leg only if the factor that caused the pinching of the sciatic nerve is eliminated. Otherwise, all attempts to improve the patient’s condition will either be ineffective or will produce a weak, short-term effect. The modern level of development of medicine makes it possible to eliminate, conservatively or surgically, almost any disorder that provokes compression of the sciatic nerve. But the sooner they are detected and treatment started, the better the prognosis will be.
Therefore, patients are always prescribed complex treatment, consisting of symptomatic and etiotropic therapy, selected according to the detected cause of sciatica. In this way, it is possible to improve the patient’s condition and eliminate the risk of relapse of the disease.
In most cases, conservative therapy is initially prescribed. Only in particularly advanced cases, when severe pathologies of the spine are detected, is surgical intervention immediately recommended to the patient. As part of conservative treatment, patients are prescribed:
- drug therapy;
- physiotherapy;
- exercise therapy;
- manual therapy.
Also, with sciatica, wearing fixation belts has a positive effect on the patient’s condition.
But conservative therapy, unfortunately, does not always give the desired results and in certain cases it is impossible to eliminate the causes of sciatica without surgery. Then patients are recommended to undergo surgical intervention appropriate to the situation.
Drug therapy
Directly to improve the patient’s condition with sciatica, the following are prescribed:
- NSAIDs and non-narcotic analgesics are used to relieve pain, and drugs from the NSAID group additionally provide an anti-inflammatory effect;
- corticosteroids - used to eliminate severe inflammatory processes and quickly reduce the swelling of soft tissues caused by them;
- muscle relaxants – help eliminate muscle spasms that occur in response to attacks of pain and help break the vicious circle of “pain - spasm - pain”;
- antioxidants, B vitamins - are used to improve tissue trophism and normalize nerve conduction along the sciatic nerve, which allows for improved sensitivity and elimination of numbness;
- angioprotectors and microcirculation stimulants - help improve microcirculation, and therefore prevent muscle atrophy and restore the sciatic nerve;
- metabolic drugs - used to improve the quality of nutrition of nerve fibers and their restoration;
- products for topical use - ointments with bee, snake venom, other warming and irritating substances, as well as containing NSAIDs, help reduce pain and stimulate local blood circulation.
If, despite conservative therapy, acute pain does not go away or a new attack occurs, patients may be given novocaine or lidocaine blockades. Such procedures are performed only in a medical facility, since they require compliance with sterile conditions and thorough mastery of special skills. When performing a blockade, anesthetics are injected directly into the area where the nerve bundles pass. This prevents the passage of painful nerve impulses and quickly leads to improvement. But the blockade does not affect the causes of pain, but only temporarily eliminates them.
In severe cases, when pain is not relieved by any other methods, patients are prescribed opioid analgesics. They are taken in short courses under the supervision of a doctor, as they quickly cause addiction and drug dependence.
Etiotropic therapy is selected strictly individually based on the nature of the detected pathologies. So, for example, when infectious diseases are detected, treatment will necessarily include antibacterial and antiviral agents, etc.
Physiotherapy
Physiotherapeutic procedures are widely used for sciatica. They help to activate blood circulation in the affected area, reduce pain, restore sensitivity and relieve swelling. The most effective are:
- diadynamic currents;
- darsonvalization;
- laser therapy;
- magnetic therapy;
- UV therapy;
- ultrasound therapy.
Electrophoresis is often indicated for sciatica. The essence of the method is to deliver drugs directly to the right place using electric current. This ensures a pronounced therapeutic effect and rapid improvement in the patient’s condition. Using electrophoresis, anti-inflammatory, antispasmodic agents, as well as muscle relaxants can be injected into the area of compression of the sciatic nerve.
Exercise therapy
Physical therapy for sciatica plays an important role. A properly selected set of exercises allows you to relieve muscle spasms, activate metabolic processes and thereby speed up the process of nerve fiber restoration and eliminate soft tissue swelling.
The exercise therapy program is selected for each patient individually, taking into account the nature of the existing spinal pathologies. Therefore, only a specialist can cope with this task.
For sciatica, most exercises are recommended to be performed lying on a hard surface. Initially, the doctor selects light exercises and requires a small number of repetitions. The first classes are conducted under his supervision so that the patient can fully master the correct technique of the proposed exercises and continue to practice independently.
Gradually, the complexity of the exercises is increased and the load is increased in order to achieve optimal results. But this can also only be done under the strict supervision of a specialist.
It is necessary to do exercise therapy every day. Exercises are performed slowly, without sudden movements. And if pain occurs, you should immediately stop exercising and consult a doctor.
Manual therapy
Properly conducted manual therapy sessions increase the effectiveness of the treatment and contribute to a rapid improvement in the condition. The use of special techniques of manipulation, mobilization, post-isometric relaxation and others can not only improve blood circulation in the affected area and relieve muscle spasms, but also normalize the position of the vertebrae, increase the distance between them to normal levels and release pinched nerve fibers. This quickly leads to relief and normalization of the patient’s condition.
But manual therapy sessions can only be trusted by qualified specialists, since incorrect movements or lack of understanding of the effects on the spine in certain diseases can cause significant harm and provoke the development of unwanted complications.
Sciatica is not uncommon during pregnancy. But due to the fact that during this period the use of most medications is unacceptable, manual therapy is one of the main ways to relieve pain and improve the condition of women before childbirth.
Features of relieving inflammation of the sciatic nerve
It is important to begin the treatment process by identifying the stage of the disease and the main causes of the problem. If, based on the results of diagnostic studies, the doctor discovers an acute stage of sciatica, the patient is hospitalized or prescribed bed rest.
To treat the problem, certain pharmaceuticals, hydrotherapy, special gymnastics, and massage are prescribed. Additionally, you can use folk remedies: alcohol tinctures, ointments, creams.
For constant, non-reducing pain, in some cases even surgery is used.
Surgery
The operation is indicated if conservative therapy is ineffective and severe pain that cannot be eliminated by conservative methods persists for more than 6 weeks, as well as in the presence of:
- large intervertebral hernias;
- spondylolisthesis;
- spinal deformities;
- hemangiomas, chondromas and other spinal tumors;
- severe dysfunction of the pelvic organs, leading to urinary or fecal incontinence.
In such situations, conservative therapy will, at best, slow down the development of these pathologies, but not eliminate them completely. But if in the isolated existence of, for example, an intervertebral hernia, this is enough to improve the patient’s condition, then in cases where the presence of spinal pathology provokes the addition of sciatica, such measures will not be enough.
After all, the cause of the pinched sciatic nerve remains, it continues to suffer and cause the corresponding clinical picture. Therefore, in such cases, surgery is the only way to achieve a lasting improvement in the condition, restore a normal quality of life and eliminate the risk of loss of ability to work.
But even if there are indications, surgical intervention cannot always be performed. It is contraindicated for:
- pregnancy;
- infectious and inflammatory diseases;
- decompensated diabetes mellitus;
- serious respiratory or heart failure.
A timely operation can completely eliminate the causes of sciatica.
Surgical treatment of sciatica for intervertebral hernias
Herniated discs are a common cause of sciatica. Moreover, the severity of symptoms of nerve entrapment does not always depend on the size of the protrusion. Sometimes even small hernias can cause serious pain, limited mobility and neurological disorders.
Today, the problem of intervertebral hernia can be completely solved only by surgery, but the type of operation directly depends on the size, location and other features of the hernia. For small protrusions, preference is given to percutaneous surgical methods: nucleoplasty and hydroplasty.
In both cases, the essence of the operation is to destroy part of the nucleus pulposus of the disc, which leads to a reduction in the size of the hernia or even its retraction due to the creation of reduced pressure inside the disc. Percutaneous surgery techniques involve the use of thin cannulas, the diameter of which does not exceed several millimeters.
Operations of this type can be performed under general or local anesthesia. The instruments are inserted into the disc under the control of the image intensifier, which allows the neurosurgeon to precisely control the direction and depth of needle insertion, and also practically reduces the likelihood of injury to nerves or large blood vessels to 0.
Using cold plasma, radio waves, thermal laser energy or liquid pressure (during hydroplasty), part of the nucleus pulposus is destroyed. The volume of intervention is clearly controlled by the surgeon. Once the desired effect is achieved, the cannula is removed, and the remaining postoperative wound does not even require sutures. It is covered with a sterile bandage, and within a few hours the patient can leave the clinic and return to daily activities.
But nucleoplasty and hydroplasty are effective only for hernia sizes up to 0.7 cm. In other cases, other methods are used:
- Microdiscectomy – involves removing the hernia through an incision of about 3 cm in the projection of the affected disc. Special miniature instruments are used to perform the operation. Microdiscectomy allows you to remove a hernia of almost any size and location, while the small size of the incision ensures ease of rehabilitation and speed of recovery.
- Endoscopic surgery is a gentle method of surgical treatment of intervertebral hernia, which involves removing it with special instruments that are inserted into the patient’s body through punctures up to 1 cm in diameter. Through endoscopic surgery it is also possible to remove almost any hernia, but if its location is complex, the technique is powerless.
Surgery for sciatica caused by spondylolisthesis
Surgical treatment is indicated for spondylolisthesis, accompanied by a displacement of the vertebra by more than 50% relative to the normal axis. It can be carried out in two ways, and the choice of a particular one is based on the results of the MRI. But with sciatica, stabilization of a displaced vertebra in a normal position is permissible only after removal of the anatomical formation that provokes compression of the nerve and the development of neurological symptoms of sciatica.
In almost all cases, stabilization of a displaced vertebra is carried out using a special plate, which is fixed to a healthy and slipping vertebra using screws. This eliminates the possibility of it being re-displaced from its anatomically correct position. But first it is necessary to carry out:
- Discectomy – removal of the intervertebral disc is indicated if, against the background of spondylolisthesis, an intervertebral hernia forms and impinges on the spinal root. If complete removal of the disc is required, it is replaced with an endoprosthesis or a graft of the patient's own bone. The first option is preferable, since modern endoprostheses are in no way inferior in functionality to natural intervertebral discs.
- Foraminotomy - is performed when a nerve is pinched in the foraminal openings of the spine as a result of a decrease in their size due to the proliferation of bone tissue or other reasons.
- Laminectomy is a radical operation used only in extreme cases when spondylolisthesis has led to stenosis of the spinal canal. During a laminectomy, both individual anatomical structures and entire vertebrae can be removed. In the latter case, the removed vertebra is replaced with appropriate implants.
Surgery for sciatica caused by scoliosis
Scoliotic deformity of the spine often provokes pinching of various nerves and the development of sciatica in particular. Therefore, if the deformity cannot be corrected conservatively, surgical intervention is resorted to.
There are several types of operations performed for scoliosis. The specific tactics for restoring the correct axis of the spine are determined individually, but in all cases special metal structures are used that fix the vertebrae in the correct position. Sometimes they involve correcting the position of the vertebrae after surgery with gradual tightening of the screws to form a more correct axis of the spine.
But if previously all operations to correct scoliosis involved long incisions along almost the entire length of the spine, today this is possible even in a minimally invasive way. As a result of eliminating spinal deformity, the nerves are freed, which helps eliminate the causes of sciatica and progressively improve the patient’s condition.
Treatment of sciatic nerve pain
To successfully treat sciatic nerve pain, the CELT Pain Clinic uses modern techniques:
- Physiotherapy - aimed at reducing pain, improving blood circulation and relieving swelling and may include: UHF therapy, electrophoresis, laser and magnetic therapy, paraffin applications;
- Systemic therapy involves the use of non-steroidal anti-inflammatory drugs. Their use should be regulated by a doctor, since they have a number of side effects. In addition, anticonvulsants can be prescribed, which are extremely effective in treating neuralgia. In addition, drugs are used that relieve pain symptoms quickly. They can be prescribed either as tablets or as injections. Our Pain Clinic uses only modern, effective means.
- Blockades aimed at the affected area. Depending on the problem causing the pain, different medications may be used to block the pain. To control the accuracy of delivery of the medicine to the problem area, we use an X-ray unit or ultrasound machine.
Do you want to be healthy and eliminate pain attacks from your life? Contact the CELT Pain Clinic!
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Prevention of sciatica
In fact, avoiding the development of sciatica is much easier than then suffering from unbearable pain and undergoing treatment. To do this, as well as to avoid relapse of the disease after successful treatment, it is enough to lead a healthy lifestyle and follow simple rules:
- maintain the level of physical activity at an optimal level (daily walking, morning exercises and visits to the pool 2-3 times a week are enough to maintain normal muscle tone and improve the condition of the whole body);
- take breaks every hour when working sedentarily and use an orthopedic corset if you need to sit for a long time;
- purchase an orthopedic mattress that will not sag under body weight;
- observe the correct technique for lifting heavy objects: with your knees bent and your back straight;
- refuse strong physical activity;
- normalize your diet and avoid overeating.
Thus, it is possible to cope with sciatica, improve the quality of life and avoid the risk of losing the ability to self-care at almost any stage of development. But it is much easier to do this when the first symptoms appear. Otherwise, the likelihood of needing surgery is very high.
Disease prevention
To prevent the development of lumboischialgia, it is recommended:
- eat rationally;
- move more often;
- exercise;
- perform exercises that strengthen the back muscles and stretch the muscles;
- when doing physical work, use the principles of biomechanics;
- balance the load with the body’s capabilities;
- fight excess weight;
- promptly treat diseases of the spine, blood vessels and digestive system;
- don't get too cold.