In principle, two forms of urinary incontinence can be distinguished: stress urinary incontinence or stress urinary incontinence and urge urinary incontinence. The most common type of incontinence is stress incontinence, when urine loss occurs during physical activity (coughing, sneezing, running, jumping, lifting heavy objects, etc.).
Unfortunately, this disease affects women of all age groups. Moreover, up to 50% of women suffer from urinary incontinence during pregnancy, and a third of them continue to experience symptoms of the disease after childbirth. Urgent incontinence is a type of incontinence in which loss of urine occurs against the background of a strong urge to go to the toilet or when thinking about the toilet, or against the background of provoking factors (the sound of running water, the proximity of a toilet or home, stress).
Urgent urinary incontinence
Urge urinary incontinence is a sudden, difficult urge to urinate when a person does not have time to “run” to the toilet.
A mixed version is also possible and often occurs, in which both types are combined in different proportions.
The basis of stress urinary incontinence is a weakening of the closing function of the urinary sphincter (the muscle that holds urine). This is often combined with weakening of other pelvic muscles (so-called pelvic floor muscle weakness) and prolapse or dislocation of organs (prolapse).
The cause of urge urinary incontinence is increased sensitivity (overactivity) of the muscle (detrusor) of the bladder.
It is clear that the approaches to treating these two forms of urinary incontinence will differ fundamentally.
Next, we will consider what Russian and European clinical guidelines offer for the treatment of urinary incontinence in women.
Let's start with the most common form - stress urinary incontinence.
As already mentioned, this form of incontinence is more common in women over 50 years of age and is associated with weakening of the pelvic floor muscles and, in particular, the urinary sphincter.
At the first stage, all women with stress incontinence are given simple but effective recommendations on how to cure urinary incontinence without drugs and without surgery. These recommendations include:
- weight loss and control;
- control of bowel regularity (avoid constipation);
- do not lift weights, avoid heavy physical activity;
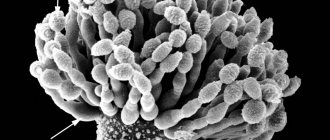
- physical therapy aimed at strengthening the pelvic muscles (Kegel exercises, training with vaginal balls or cones);
Of the listed activities, I will tell you in more detail about training the muscles of the perineum and pelvic floor. The fact is that this is actually a fairly effective way to cure urinary incontinence without surgery. American gynecologist Arnold Kegel in the middle of the last century proposed an exercise consisting of rhythmic contraction of the muscles surrounding the urethra, which later received his name.
Kegel exercise
How to do a Kegel exercise correctly? First you need to feel the muscles involved in holding urine. To do this, try holding your urine for a few seconds while urinating. When you feel which muscles need to be contracted for this, try to do it without urinating, first in a lying position, and then in any position of the body. Three seconds of tension, three seconds of relaxation. To enhance the effect, use special devices - vaginal balls or weights, as well as exercise equipment. These devices are widely available on the Internet. Repeat Kegel exercises at least three times a day for 15-30 repetitions. The effect can be expected after 2-3 months, but do not stop training to achieve maximum results. In addition to eliminating (or preventing) stress urinary incontinence, Kegel exercises eliminate uterine and vaginal prolapse, improve blood circulation in the pelvic organs, and improve sexual sensations.
Surgeries for urinary incontinence. Installation of the mesh (sling).
If the above measures have insufficient effect, more radical treatment is required. It is pertinent to note here that there are no effective medications for the treatment of stress urinary incontinence. Both domestic and foreign clinical guidelines unanimously recognize sling operations as the method of choice in the treatment of this form of urinary incontinence in women. The essence of these interventions is the implantation of a synthetic loop (mesh) under the lower wall of the urethra, which provides support and compensates for the weakening of the musculofascial apparatus of the perineum.
How is a urethral sling (TVT-O, TOT) installed? This operation is a modern high-tech minimally invasive intervention. Urethropexy (another name for this manipulation) is performed under general or spinal anesthesia. The loop is installed through a minimal (about 1 cm) incision in the anterior vaginal wall, which is immediately sutured with a cosmetic self-absorbing suture. The duration of the procedure is no more than 30 minutes. The very next day, after a follow-up examination, the woman is discharged home. The effect of the operation occurs immediately, incontinence stops. Some models of mesh implants allow minor adjustments in the first day after implantation to more accurately adjust the degree of tension of the loop. Thus, the postoperative period is easy and painless. The main limitation is the need for sexual abstinence for a month. The effect of installing a loop lasts for many years.
At the same time, incorrect implantation of a urethral sling is fraught with unpleasant complications. These include: damage to the vaginal wall, damage to the urethra and bladder, bleeding, urinary retention. Complications are extremely rare and are mainly associated with violation of the surgical technique. Therefore, the surgeon’s experience is a decisive factor in the success and safety of sling operations. When you contact me, you can be sure of the result.
Is it possible to install a midurethral sling if I am planning a pregnancy?
After implantation of the prosthesis, you can safely plan a pregnancy and give birth through the birth canal. At the same time, the risk of relapse of the disease does not exceed 20% (regardless of whether a Caesarean section was performed or the birth was vaginal).
Bibliography
- Centers for Disease Control and Prevention. (2014). Prevalence of Incontinence Among Older Americans (PDF, 1.3 MB). National Center for Health Statistics. Vital Health Statistics; 3(36).
- Reddy, J., & Paraiso, M. F. R. (2010). Primary Stress Urinary Incontinence: What to Do and Why. Reviews in Obstetrics & Gynecology; 3(4): 150–155.
- Stewart, W. F., et al. (2003). Prevalence and Burden of Overactive Bladder in the United States. World Journal of Urology; 20(6): 327–336.
- American College of Obstetricians and Gynecologists. (2016). Urinary Incontinence (PDF, 84 KB). (link is external)
- Altman, D., Granath, F., Cnattingius, S., & Falconer, C. (2007). Hysterectomy and Risk of Stress-Urinary-Incontinence Surgery: Nationwide Cohort Study. (link is external) Lancet; 370(9597): 1494–1499.
- Gleason, J. L., Richter, H. E., Redden, D. T., Goode, P. S., Burgio, K. L., & Markland, A. D. (2013). Caffeine and Urinary Incontinence in Women. International Urogynecology Journal; 24(2): 295–302.
- Sangsawang, B., & Sangsawang, N. (2013). Stress Urinary Incontinence in Pregnant Women: A Review of Prevalence, Pathophysiology, and Treatment. International Urogynecology Journal; 24(6): 901–912.
- Kim, D. K., & Chancellor, M. B. (2006). Is Estrogen for Urinary Incontinence Good or Bad? Reviews in Urology; 8(2): 91–92.
- Health Resources and Services Administration, Agency for Healthcare Research and Quality. (2012). Nonsurgical Treatments for Urinary Incontinence in Adult Women: Diagnosis and Comparative Effectiveness (PDF, 12.9 MB). Comparative Effectiveness Review; 36.
- US National Library of Medicine. (2017). Kegel exercises – self-care.
- Institute of Medicine. (2004). Dietary References Intakes: Water, Potassium, Sodium, Chloride, and Sulfate (link is external).
- Rosinger, A. and Herrick, K. (2016). Daily water intake among US men and women, 2009–2012. National Center for Health Statistics Data Brief; 242.
- American College of Obstetricians and Gynecologists. (2017). Surgery for Stress Urinary Incontinence (PDF, 85 KB). (link is external)
- Food and Drug Administration. (2018). Considerations about surgical mesh for SUI.
Hyaluronic acid for urinary incontinence
Another modern atraumatic method of treating stress urinary incontinence is the introduction of bulk-forming agents into the tissue around the urethra . The most commonly used preparation is hyaluronic acid gel. This technique is even less invasive, and therefore has a lower risk of undesirable consequences, and does not require anesthesia or hospitalization. But at the same time, it has an efficiency quite comparable to sling operations. The disadvantage of periurethral injection of hyaluronic acid for urinary incontinence is the temporary effect (6-12 months) and, accordingly, the need to repeat these procedures annually.
Now let's look at another common form of urinary incontinence - urgency. As already mentioned, the cause of urge urinary incontinence is a sudden increase in pressure in the bladder due to uncontrolled contraction of its wall. Accordingly, the therapeutic effect is aimed at reducing the contractility and excitability of the bladder muscle (detrusor). This is achieved, most often, with the help of medications. Accordingly, surgical treatment for this type of urinary incontinence is not used.
Diagnosis of the disease
In order to accurately diagnose urinary incontinence, you need to seek help from a gynecologist. The doctor will conduct an examination and prescribe the necessary tests.
Agnostics includes the following activities:
- Examination by a specialized specialist. Collection of medical history and complaints. The doctor prescribes keeping a special urination diary, which displays the volume and number of urinations per day.
- Gynecological examination (examination of the anatomical structures of the female reproductive system).
- Cough test. The study is carried out on a full bladder. The woman needs to cough or strain. If urination occurs after coughing, the test is considered positive.
- Uroflowmetry (a method for diagnosing urodynamics that involves measuring urinary flow). It is carried out strictly on a full bladder, using a special uroflowmeter device.
- Cystoscopy (examination of the surface of the bladder).
- Ultrasound (necessary for a more accurate visualization examination).
- A combined urodynamic study (CUDI) is necessary to determine the cause of urination.
Laboratory research
- Creatinine, urea - to assess the state of kidney function;
- General urine analysis;
- Blood test for the level of glycated hemoglobin;
- Flora smear;
- Cytological examination of the cervix.
At the Federal Scientific and Clinical Center of the Federal Medical and Biological Agency, you can undergo all the necessary diagnostics and laboratory tests in one day, which will significantly save your time. However, the list of studies can be changed depending on the indications and health status of the patient. The doctor will prescribe all the necessary procedures during a face-to-face consultation and, based on the results, will select the most optimal treatment method.
Drugs for the treatment of urinary incontinence
Two groups of medications are used to treat this form of urinary incontinence. The first, traditionally used group, currently includes four main drugs: Tolterodine (Detrusitol), Solifenacin (Vesicare), Oxybutynin (Driptan) and Trospium chloride (Spazmex). All of these drugs are highly effective and safe, and are the first line of treatment for urge urinary incontinence. Undesirable effects of their use include dry mouth and a tendency to constipation. Other side effects are less common. There are also contraindications, which the doctor must warn you about.
The second group is relatively new and so far consists of a single drug - Mirabegron (Betmiga). It is prescribed as a second-line drug when the first group of drugs is insufficiently effective.
A combination of drugs from both groups is also possible. The duration of drug therapy for urinary incontinence is usually no less than three months, and is often carried out for months and years.
As an alternative to continuous use of drugs, and also if their effectiveness is insufficient, intravesical botulinum therapy can be used. For urge urinary incontinence, Botulinum toxin is injected directly into the wall of the bladder (detrusor). This manipulation is performed under anesthesia (“during sleep”), using a cystoscope. The effect of botulinum therapy for urgent urinary incontinence lasts up to 6 months, after which repeated administration is necessary.
If you have urinary incontinence, where to start?
If you or your loved ones are faced with this problem for the first time, then the algorithm of actions given below will help you quickly come to the correct solution to the problem.
- Note the factors that provoke incontinence (under what circumstances does it occur). This may include coughing, laughing, changing body position (for example, standing up), lifting heavy objects, eating spicy foods, alcohol, or caffeinated drinks.
- Keep a diary of urination, that is, write down the time and volume of urine. Note all episodes of incontinence, as well as times when you have difficulty holding in urine. For reliability, keep the recording for 2-3 days (including night hours).
- With this information, make an appointment with a urinary incontinence specialist. For example, contact me by calling 8-903-964-03-01 or filling out the electronic form via the link
The sooner you start acting, the sooner you will return to your usual comfortable “dry” life.
Risk factors for the development of urinary incontinence in women
Here I will list several factors that increase the likelihood of urinary incontinence (we are talking mainly about the stress form):
- Multiple and/or traumatic births;
- Work involving heavy lifting;
- Excess body weight;
- Constipation;
- Bronchial asthma;
- Sedentary lifestyle;
- Prevention of urinary incontinence will include regular physical activity, body weight control, and daily bowel movements.
Author: candidate of medical sciences, doctor of the highest category, Rotov Anton Evgenievich
What restrictions exist after surgery?
As a rule, within 5-7 days after discharge from the hospital, women can return to everyday activities - going to work, doing housework. For 1-1.5 months after surgery, patients are advised to lead a gentle lifestyle: avoid lifting heavy objects, active sports, sexual activity, and also refrain from visiting saunas, swimming pools, and taking baths.
It is recommended to pay attention to behavioral habits: avoid smoking, adhere to a balanced diet, normalize body weight.
Questions about the article
Tatiana
September 20, 2021 at 05:20 pm
Tell me, what to do if you are planning a pregnancy due to incontinence due to OAB? I’m currently taking an m-anticholinergic drug (Spazmex), which actually helps me, but this drug, as I read, is not allowed during pregnancy. In addition, as far as I understand, it can worsen the condition. What can be done to prevent the condition from worsening during pregnancy while discontinuing the drug?
Anton Evgenievich Rotov
September 21, 2021 at 09:45
During pregnancy, it is indeed undesirable to use any drugs. In this regard, some aggravation of the manifestations of OAB is possible. I don’t know of any absolutely reliable and safe methods to prevent this. Calming herbal preparations (valerian, motherwort), which are often prescribed during pregnancy, may be of some benefit. At the same time, spontaneous improvement is also possible. Need to try.
Elena
August 9, 2021 at 06:57 pm
Hello! The son is a 15-year-old teenager with urinary incontinence when laughing. What to do, please tell me. Thank you in advance!
Anton Evgenievich Rotov
August 9, 2021 at 07:01 pm
This is not typical. It is necessary to be examined by a urologist, and possibly also by a neurologist (but start, of course, by contacting a urologist)
Why you need to treat nocturnal enuresis
There is not a single person who would like to sleep in diapers or wake up in a puddle of urine. A constant smell, wet underwear and judgmental glances from even the closest people are the eternal companions of people with NE.
Patients with nocturnal enuresis cannot live a normal life: travel is excluded for them, and they have to sleep alone. This is oppressive, an inferiority complex develops, and the psyche is destroyed.
As for health, enuresis is often only a symptom of a disease that requires mandatory treatment, especially when it comes to the kidneys or hormonal imbalance.