Questions:
- What is pyoderma?
- Causes of pyoderma
- Symptoms
- Types of pyoderma
- How is pyoderma transmitted?
- Chronic pyoderma
- Pyoderma in children
- Pyoderma in newborns
- Treatment of pyoderma
- Is it possible to treat pyoderma at home?
- At what age can Timogen cream be used in children?
- Treatment with folk remedies
- Prevention
Medical specialists answer frequently asked questions from users
What is pyoderma?
Pyoderma is a disease of purulent skin lesions, most often caused by pyogenic (pyogenic) cocci - streptococci and staphylococci, which are constantly found on the skin and mucous membranes. In addition to these pathogens, there are other microorganisms on human skin, such as pseudodiphtheria bacillus, yeast-like fungi, etc., which can also cause disease under certain conditions. The name of the disease comes from the Greek py'on - pus and de'rma - skin). This is one of the most common skin diseases.
to the begining
Prevention
Preventing infectious and inflammatory skin diseases on your own is not a difficult task.
Basic methods of prevention:
- hygienic skin care;
- timely treatment of cuts and burns;
- treatment of chronic infections;
- regular examinations by a dermatologist for chronic skin diseases;
- control blood sugar levels in diabetes.
Consultation with a dermatologist and immunologist will help the patient learn more about methods of prevention and treatment of pyoderma.
Causes of pyoderma
Frequent causes of pyoderma are hypothermia and overheating of the body under production conditions.
When the body cools, blood circulation is disrupted, swelling of the skin occurs, sebum secretion and sweating decrease, as a result, the skin becomes dry and flaky, making it easily susceptible to injury and infection.
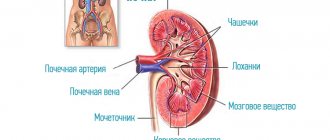
Overheating of the body leads to loss of water and chlorides (mineral salts), the latter affecting the vascular system and the functions of the kidneys and skin.
The possibility of pyogenic infection can be increased by additional irritants like oils and other contaminants.
The skin is able to destroy microorganisms that fall on its surface due to the acidity of the skin (pH), the so-called “acid protective coat of the skin.” Bacterial infection occurs faster in those areas of the skin where the pH is higher - these are the armpits, interdigital folds of the feet, and inguinal folds. Therefore, pathological changes occur more often in these places.
to the begining
Kinds
Superficial staphyloderma
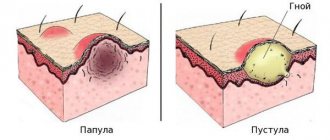
The most common are folliculitis, sycosis vulgaris, ostiofolliculitis, and epidemic pemphigus of newborns. Ostiofolliculitis is an abscess surrounded by a zone of mild hyperemia, penetrated by hair. With folliculitis, the abscess is located against the background of a painful bluish-pink nodule. Vulgar sycosis is called multiple, recurrent ostiofolliculitis and folliculitis against the background of thickened bluish-pink skin, often in the mustache and beard area. Epidemic pemphigus of newborns is a severe, contagious disease of the first days of life. In addition to the palms and soles, the child’s skin becomes covered with large blisters, which later form crusts and extensive erosions.
Deep staphyloderma
The most famous are boils, carbuncles, and hidradenitis. The boil develops from ostiofolliculitis or folliculitis. First, a painful node appears in the thickness of the skin, which enlarges; a large pustule is formed in its center, which opens with the subsequent separation of the purulent-necrotic core. After which, the resulting ulcer gradually scars.
A carbuncle is several boils located in one place, closely adjacent to each other, against the background of a general dense, edematous infiltrate of a bluish-purple color. The deep ulcer formed after opening the carbuncle heals with a rough scar. Hidradenitis is a purulent inflammation of the apocrine sweat glands, often recurrent. In the armpits, anogenital area, and around the nipples of the mammary glands, deep, painful nodes appear, over which the skin is colored bluish-pink. The nodes are opened with the release of liquid pus.
Superficial streptoderma
The most common is streptococcal impetigo . This disease occurs more often on the face in children and young women. Against the background of slightly hyperemic skin, phlyctens (bubbles with opalescent contents) appear, shrinking into yellowish crusts or eroding. When staphylococci are attached, the crusts become greenish-yellow or sometimes hemorrhagic ( impetigo vulgaris ). Without treatment, the disease can affect large areas of the skin. Lichen simplex , more often in children, is an abortive form of streptococcal impetigo. It is expressed by the appearance of whitish or light pink, slightly flaky spots.
Deep streptoderma
Vulgar ecthyma . With this disease, deep pustules appear, shrinking into purulent-bloody crusts, under which ulcers are found. After 2-3 weeks, the ulcers heal.
to the begining
Diagnostics
To diagnose pyoderma, the doctor first examines the rash and determines its nature. Then the discharge from the purulent areas is examined under a microscope. If the tissue damage is very severe, a biopsy is often prescribed.
Additionally, the doctor may recommend a blood test to exclude diabetes, control leukocytes and ESR.
When making a diagnosis, cutaneous forms of tuberculosis and syphilis, as well as various fungal, parasitic and other skin lesions that are not related to pyoderma, are excluded.
Pyoderma in children
Pyoderma in children most often develops due to parents' failure to comply with the hygiene regime. That is, parents do not wash their hands before touching the child, wash the child poorly or rarely, the child’s clothes are poorly washed and not ironed, and their clothes are rarely changed. In rare cases, also if hygiene rules are not followed, it is possible for a child to become infected from relatives who have foci of chronic infection - carriers of staphylococci, streptococci, people with reduced immunity (patients with diabetes, alcoholism, old people, cancer patients).
to the begining
Risk factors
The etiology of pyoderma is not limited to the mechanisms of formation of the purulent-inflammatory process. Dermatologists know the forms of predisposition to this disease associated with lifestyle, heredity and the patient’s individual history.
Known risk factors:
- Failure to comply with personal hygiene rules. Constant skin contamination increases the risk of infection.
- Overheating or hypothermia of integumentary tissues. Temperature changes disrupt the functions of local immunity. Often, after hypothermia, the skin becomes a gateway to infection.
- Age. In newborns and the elderly, pyoderma most often occurs due to insufficient effectiveness of local immunity.
- The presence of a large number of allergic reactions and autoimmune diseases (especially in children.)
- Pathologies of the endocrine system. The condition of the skin largely depends on hormonal influences.
- Metabolic diseases: diabetes and obesity.
- Congenital and acquired immunodeficiency conditions.
- Poor nutrition leading to a deficiency of certain vitamins and microelements in the body.
- Unfavorable family heredity. Skin diseases may be associated with the transmission of genetic mutations.
The causative agents of pyoderma dermatitis are found in the environment and on the surface of the integumentary tissue. These are staphylococci, streptococci and some pathogenic fungi. People often become infected with pyogenic bacteria in a hospital setting.
Pyoderma in newborns
Pyoderma in newborns most often occurs due to nosocomial infection, violation of the rules of child care and in weakened, premature children. Common pyoderma in newborns is called bullous impetigo, it is life-threatening and progresses very quickly; treatment is carried out only in a hospital. Red rashes appear on the skin, which quickly turn into hyperemia of the entire skin; detachment of the epidermis occurs with the formation of large blisters and crusts. When an infection gets into the umbilical wound, inflammation develops - omphalitis, which can quickly develop into umbilical sepsis. Symptoms of omphalitis: pus from the umbilical wound and an unpleasant odor, swelling and redness of the edges of the wound and the skin around it, increased body temperature, refusal to eat, anxiety.
to the begining
General information
Pyoderma - what kind of disease is it? Pyoderma is a skin disease represented by a large group of acute and chronic purulent skin diseases caused by pyogenic microorganisms. Sycosis , boil , impetigo , acne vulgaris , diaper rash, erysipelas - this is just a short list of forms of pyoderma, which are often the cause of temporary disability.
In the vast majority of patients, pyoderma often recurs or takes a chronic course, requiring long-term and persistent treatment. Pyoderma code according to ICD-10: L08.0 – Pyoderma. Dermatitis: purulent, septic, pyogenic. Objective signs of pyoderma are various morphological elements on the skin, and the clinical course describes the developing pathological processes in it.
Bacterial skin infections (staph/streptococcal) are extremely common and can range from mild to life-threatening infections. The proportion of pyoderma among dermatological pathologies in adults varies between 17-45%. In countries with high economic development, they are detected in almost 32% of patients with infectious diseases. Pyodermatitis is more common among workers employed in the mining, metal/woodworking industries, transport workers and agricultural machine operators. In countries with a hot, humid climate, pustular skin diseases are second only to mycoses in terms of incidence. It occurs in all age groups, but in children the incidence of pyoderma is much higher than in adults, and the proportion of incidence is 25-50% of all dermatoses .
Pyoderma in adults occurs more often in the age group of 45-60 years, and by gender, men predominate, in whom pyoderma is diagnosed in 65–72% of all cases. However, it is extremely difficult to accurately estimate their prevalence, both in general and among specific population groups, due to the wide variety of clinical manifestations and the rapid resolution of the rashes in most cases (within 7-10 days). Skin infections vary in many ways: causative agent (microbial associations), clinical manifestation, therapy and prognosis.
Many people are interested in the question: is pyoderma contagious or not? Yes, this is a highly contagious disease, easily transmitted from a sick person to a healthy person, and in crowded rooms (children's groups) some types of pyoderma can take on the character of limited epidemics. The transmission mechanism is direct contact (direct contact of damaged skin with the skin of a sick person) and indirect contact (household contact through personal hygiene items, toys, household items). Asymptomatic carriers of group A streptococci also pose a significant danger. The main factor in the spread of some types of pyoderma from a carrier/infected person is the proximity of a healthy person to the person who secretes microorganisms.
Treatment
- Treatment in children
Treatment of omphalitis is carried out only by a doctor. In the initial stage, local use of medications is possible: washing the wound with a solution of hydrogen peroxide, treatment with brilliant green, iodine solution, methylene blue solution and various local antimicrobial drugs. Treatment of pyoderma in children involves the use of broad-spectrum antibiotics, infusion therapy, and immunomodulators. In the initial stages of pyoderma, it is possible to treat pyoderma with local means - solutions of boric and salicylic acids, sanguiritin, eucalymin, tomicide, cyminal and others in the form of solutions, lotions, under a bandage. See also our specialist’s answer to the user’s question: Pyoderma in children, how to cure it? - Treatment in adults
In adults, pyoderma is also treated by a doctor. For mild pyoderma, local medications are used (see above); for moderate severity, broad-spectrum antibiotics and sulfonamides are added to local treatment.To increase the body's resistance in the treatment of pyoderma, the immunomodulatory drug Thymogen is used. These are Thymogen cream, which is applied to the affected areas, and Thymogen solution for injection.
to the begining
Consequences and complications
In cases of uncomplicated pyoderma with shallow skin lesions, the skin is completely restored after recovery; in cases of protracted/chronic pyoderma, when deep layers of the skin are involved in the pathological process, pigment spots and scars remain after recovery. In the absence of timely and adequate therapy, there is a high risk of progression of the disease and an increase in the severity of its course with the possibility of developing lymphangitis , lymphadenitis , meningitis . In young children, complications such as tonsillitis , scarlet fever and glomerulonephritis .
Can it be treated at home?
- First of all, it is necessary to establish the nature of pyoderma. In other words, identify the causative agent of the disease and determine its sensitivity to antibiotics. After a course of antibacterial therapy (local use of antibacterial drugs in most cases is ineffective) against the background of normal multivitamin-mineral support (taking vitamins), such diseases usually go away. But pyoderma, as a rule, develops against the background of reduced immunological resistance or is provoked by diseases of the internal organs: stomach, intestines, liver, pancreas. Therefore, an in-depth examination is necessary.
to the begining
List of sources
- Masyukova S.A., Gladko V.V., Ustinov M.V. and others. Bacterial skin infections and their significance in the clinical practice of a dermatologist. Consilium Medicum. 2004; 6 (3): 180–5 p.
- Dermatovenerology. National leadership. (Edited by Yu.K. Skripkin, Yu.S. Butov, O.L. Ivanov) M: GEOTAR-Media, 2011. – 1024 p.
- Belkova, Yu. A. Pyoderma in outpatient practice / Yu. A. Belkova // Clinical microbiology and antimicrobial chemotherapy. 2005. T. 7. No. 3. P. 255 – 270.
- Kirichenko I.M. Modern approaches to the treatment of infectious skin diseases. Cons. Med. 2006; 8 (1): 8–10.
- New possibilities for local therapy of pustular skin diseases/Nurullin R.M., Abdrakhmanov R.M., Khaliullin R.R.// Kazan Medical Journal – 2012 – T.93, No. 2.