Gastroenterologist
Belousov
Evgeniy Leonidovich
19 years of experience
Candidate of Medical Sciences, Member of the Russian Gastroenterological Association.
Make an appointment Many patients experiencing problems with the gastrointestinal tract are interested in what a stomach ulcer is, what are the first signs of a stomach ulcer, and what triggers the onset of the disease. A gastric ulcer should be understood as a pathology of the gastrointestinal tract; ulcers appear on the walls of the stomach due to various reasons.
This pathological process is characterized by complex changes and painful sensations in the patient’s body, which are provoked by a local ulcer. Such processes occur in the stomach and duodenum due to reasons that we will analyze further, consider the development of stomach ulcers and methods of treating the disease.
General information about stomach ulcers
Almost every person has experienced stomach pain due to irregular nutrition.
But with frequent painful sensations in the human stomach, patients are recommended to undergo examinations and tests, because such signals may be the first indicators of the development of a stomach ulcer. You should pay attention to the manifestations of signs of gastrointestinal diseases, because failure to consult a doctor in a timely manner can cause irreversible changes, which will require surgical intervention. If you suspect a stomach ulcer, it is recommended to immediately undergo diagnostics and examination by an experienced doctor, who will identify the causes and manifestations and prescribe appropriate effective treatment depending on the stage and specifics of the stomach ulcer.
In the first stages, the symptoms and manifestations are not too pronounced; it is for this reason that the transition of the disease to an acute advanced form can be missed. The danger of stomach ulcers lies in the fact that the mucous membrane, muscles, and the entire depth of the stomach wall are affected, which is why ulcers require timely detection and treatment. The signs become clear starting from the second stage of the disease.
Risk factors include neglecting hygiene rules before eating, eating from dirty dishes, and eating stale food. It is recommended to take full responsibility for the freshness of products and personal hygiene in order to avoid pathological processes in the gastrointestinal tract.
Main causes
The cause of a defect in the gastric mucosa is considered to be an imbalance between the aggressive secretions of the stomach and the protective qualities of the mucous membrane. To digest food, the stomach secretes pepsin and hydrochloric acid. To prevent them from destroying the stomach, mucus forms on its surface, protecting the organ. If more acid is produced and less mucus is produced, an ulcer may form. The background for such a pathology may be a decrease in gastric motility, a violation of the regenerative - restorative properties of the mucous membrane against the background of certain diseases.
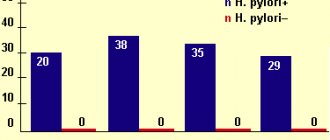
The main etiological cause of ulcer formation is damage to the mucous membrane of the HP. This bacterium successfully survives in an acidic environment and produces an enzyme that causes an inflammatory reaction with subsequent formation of a defect. Helicobacter pylori is detected in 82% of patients suffering from gastric ulcers.
Another reason may be uncontrolled use of anti-inflammatory non-steroidal drugs, such as aspirin.
Provoking factors may be:
- smoking and alcohol abuse;
- constant consumption of spicy food;
- stressful situations;
- hereditary predisposition;
- dry food;
- eating disorder.
Gastric ulcers often develop against the background of certain diseases, such as atrophic gastritis and hormonal pathologies.
Symptoms and causes of the disease
The main causes of the development of stomach ulcers can be:
- pathological inflammatory processes in the gastrointestinal tract;
- Among the common causes of the disease is an increased level of gastric acidity;
- the cause is constant alcoholism and drinking alcoholic beverages of different strengths;
- the reason may be chronic stress and depression;
- decreased immunity;
- Causes of ulcers can also occur under the influence of the pathogenic microorganism Helicobacter. Helicobacter multiplies in the acidic substance of the stomach, possessing some protective factors;
- Negative factors also include heredity, improper and irregular nutrition;
- the disease occurs as a result of consuming low-quality products, smoking, and taking certain medications with significant side effects for the gastrointestinal tract.
To establish the cause of stomach ulcers, it is also necessary to check the patient for concomitant diseases, such as diabetes, syphilis, pancreatitis, gastritis, tuberculosis, Crohn's disease, and cirrhosis of the liver.
Clinical manifestations of diseases of the stomach and duodenum are usually pronounced. The severity of symptoms is determined by the stage - remission or exacerbation. The symptoms manifest themselves most clearly during the period of exacerbation of ulcerative pathology, which is characterized by pronounced manifestations of signs of a stomach ulcer; they can be determined by a doctor during examination and during diagnosis using modern methods.
The main symptoms are:
- painful sensations in the epigastric zone of varying intensity - periodic or worsening. If you experience regular pain, you should check with a qualified doctor;
- a common symptom is hunger pain, which decreases after eating;
- The nature of the pain is different - from aching to sharp cutting. Depending on this symptom, drug treatment is prescribed to reduce pain and spasms;
- heartburn or rotten belching, which depends on the level of stomach acidity. Such symptoms are more often observed with increased acidity;
- Frequent symptoms include stool disorders - constipation with high acidity or diarrhea with low acidity;
- signs of an ulcer also include nausea, bloating;
- rumbling in the stomach, since the underlying parts of the gastrointestinal tract are susceptible to pathology.
Having noticed these signs in a timely manner, you must immediately consult a doctor at the hospital to make a diagnosis and prescribe an appropriate treatment regimen. If there is no response to the signs, the disease occurs with certain complications:
- perforation of the stomach, that is, the occurrence of a through defect connecting the lumen of the stomach with the peritoneal area;
- penetration or defect in the gastric mucosa, which is closed by a nearby organ (omentum or pancreas);
- bleeding in the gastrointestinal tract - special attention must be paid to this sign, it requires immediate hospitalization and, without taking action, leads to death;
- malignant oncological formation in the area of the ulcer.
Are you experiencing symptoms of a stomach ulcer?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
Symptoms of peptic ulcer of the stomach and duodenum
- Aching or cramping pain, low intensity in the epigastric region, often occurs on an empty stomach or immediately after eating
- Constant heartburn, especially at night and in the morning, sour belching
- Nausea
- Belching with air, sour or bitter taste
- Heaviness in the epigastric region after eating, a feeling of rapid filling of the stomach
- Decreased appetite
- When bleeding from ulcers, vomiting appears like “coffee grounds”, dark stools (melena)
- With perforation of ulcers - severe, dagger-like pain in the epigastric region, nausea, vomiting, painful tension in the abdominal muscles
Diagnosis of ulcers: features and procedures
Diagnosis of the disease is carried out by an experienced gastroenterologist, who can determine an accurate diagnosis after examination, history taking and diagnostics using hardware methods.
The gastroenterologist analyzes the patient’s medical history and complaints, family history, and also carries out a number of diagnostic measures. An ulcer is diagnosed using a general blood and urine test, the acidity of gastric juice is examined, and diagnostics is carried out using esophagogastroduodenoscopy. If internal bleeding is suspected and for an accurate diagnosis, a stool test for occult blood is collected. The main goal of the doctor in diagnosis is to confirm the ulcerative defect in the stomach wall and the presence of Helicobacter in the patient. The disease is diagnosed in the following ways:
- X-ray method using barium suspension;
- fibrogastroduodenoscopy visualization of the gastric mucosa using a special magnifying device;
- urease method - based on the detection of urease in exhaled air, which occurs as a result of the proliferation of Helicobacter in the stomach;
- PCR diagnostics – determines the nucleic acid complexes that characterize Helicobacter;
- serological methods for diagnosing the disease, involving the determination of immunoglobulins to Helicobacter;
- specialized tests performed during fibrogastroduodenoscopy.
At the same time, examinations are performed to ensure the possibility of excluding the development of pathological complications. Ultrasound examinations of the peritoneal organs and X-ray contrast examination using barium are performed, which makes it possible to determine the size of the ulcer.
Panel: Risk factors predisposing to ulcer perforation
Nonsteroidal anti-inflammatory drugs (including aspirin)
Inhibitors of prostaglandin synthesis lead to increased gastric acid production and decreased mucus secretion.
Smoking
Smoking suppresses bicarbonate secretion. Nicotine stimulates acid secretion. Significantly associated with ulcer perforation in people under 75 years of age
Helicobacter pylori
It is most common in cohorts of young adults (usually <40 years of age) with perforated duodenum in low- and middle-income countries. Different virulence of strains may have a role in genesis.
Marginal ulcer after bariatric surgery
Probably associated with ischemia of the anastomosis.
Starvation
Perforation of ulcers has been reported during Ramadan. Fasting causes increased acid production when the stomach is empty.
Use of crack, cocaine and methamphetamine
May lead to severe vasoconstriction followed by ischemia. May also cause blood clots and mucosal necrosis.
Zollinger-Ellison syndrome (gastrinoma)
Rarely; risk of formation of recurrent and multiple ulcers. Increased gastrin secretion causes increased secretion and persistence of hydrochloric acid in the stomach and duodenum, with ulceration and potential perforation of the gastrointestinal wall.
Stress ulcers
Occurs in patients in critical condition (burns, injuries, etc.) in the intensive care unit; most often complicated by bleeding, but sometimes perforate. Difficulty in diagnosing patients under the influence of sedatives or on mechanical ventilation.
Steroids
Affects the inflammatory cascade, including the synthesis of prostaglandins. They can dull the signs of peritonitis, blurring the picture and making it difficult to make a diagnosis.
Salt
Increased consumption increases the acidity of the stomach.
Prognostic factors and outcome prediction
No single factor readily identifies patients at high risk for a poor outcome, but older age, the presence of comorbidities, and diagnostic delay before surgery have been consistently associated with an increased risk of death. Clearly, identifying modifiable risk factors to potentially improve outcome is of great interest. In a systematic review covering more than 50 studies with 37 preoperative prognostic factors and including a total of 29,782 patients, several risk factors were consistently associated with mortality (Figure 3). Only two-thirds of studies reported estimates adjusted for risk factors. In addition, definitions and criteria for dividing (eg, age for defining the “elderly” group, creatinine level for diagnosing acute renal failure, and blood pressure for shock) were not consistent across studies. Thus, doctors have tried to combine risk factors to predict disease outcome.
Fig. 3. Preoperative prognostic factors unfavorable for the risk of mortality in perforated peptic ulcer disease
Unfavorable preoperative prognostic factors for mortality. Data taken from Moller et al. ASA - American Society of Anesthesiologists Risk Assessment Score.
Clinical prediction rules
Ideal clinical prediction rules must be easy to use, reliable, highly generalizable, and well validated both within and outside of a given study. However, the outcome prediction rules for ulcer perforation evaluated so far have not yet been classified as ideal.
Difficulties in defining a unified set of factors are likely related to their number and the overall complexity of the disease. Some factors considered are fixed (for example, patient age and gender), while others are adjustable (for example, time to treatment and resuscitation). In addition, given geographic differences in age, sex, and disease onset patterns, a universal, reproducible, and valid risk scoring system may be difficult to develop. The most widely used disease-specific prognostic score in patients with perforated ulcers is the Boey score, which is based on the presence of serious medical conditions, preoperative shock, and ulcer perforation more than 24 hours before surgery. However, its positive predictive value of 94% reported in early studies was not replicated in subsequent studies. Other prediction rules specifically for ulcer perforation have been proposed. However, none of these scoring systems have been validated in external cohorts, making their generalizability difficult. In addition, several different general surgical scoring systems and ICU scales have been used in patients with perforated ulcers. Again, the results were not uniformly confirmed over time and across cohorts, suggesting low external validity of these systems in this setting. It is clear that appropriate devices and studies are needed to analyze and compare data across regions to identify high-risk patients and to facilitate progress in research and experimental development.
Patient Management Strategies
Treatment of patients with perforated peptic ulcers should include early diagnosis and prompt initiation of resuscitation measures. A high short-term mortality rate associated with this disease is reported (10-30%), and morbidity and complications occur in 50-60% of patients. This means that a careful and structured therapeutic approach is required to improve results. There are several strategies and options available (Table 1), but the patient's condition should be taken into account when planning their use.
Preoperative preparation
Sepsis is often present in patients with perforated ulcers, being suspected in only 30-35% of patients presenting with sepsis on arrival to the operating room, and is a leading cause of death, accounting for 40-50% of deaths. Within 30 days after surgery, more than 25% of patients develop septic shock, leading to death in 50-60% of cases. Accordingly, a thorough history and measures to prevent, detect, and treat sepsis in patients with perforated ulcers may lead to a reduction in mortality and morbidity. This goal can be achieved by systematically assessing for signs of sepsis and treating patients according to the principles of the Surviving Sepsis Campaign, including fluid resuscitation, bacterial culture, empiric broad-spectrum antibiotic therapy, and resource management. A multidisciplinary preoperative approach based on these principles has been evaluated in non-randomized clinical trials in patients with complicated perforation peptic ulcer disease, with a statistically significant demonstrated reduction in mortality (number needed to treat per ten patients).
Conservative treatment
In patients with very few or localized symptoms who are in good clinical condition, the choice of surgery may be deliberately deferred in favor of a period of observation. The decision to forego immediate surgery for an initial attempt at a primary conservative strategy is not new and was first advocated more than half a century ago. In a number of consecutive samples, more than half of all patients with perforated ulcers experienced spontaneous obliteration, and such patients underwent successful conservative treatment. The strategy should include intravenous antibiotics, restriction of natural or nasogastric feeding, antisecretory and antacid medications (proton pump inhibitors), and imaging with water-soluble contrast to confirm perforation.
The only RCT ever conducted in this area (before the introduction of proton pump inhibitors) showed success of the conservative strategy in the majority of patients, but a high failure rate in older patients (aged > 70 years). However, when choosing a conservative treatment method, it must be taken into account that mortality from ulcer complications increases with every hour of delay before surgery.
Surgery
Delay of surgery was a factor consistently associated with mortality. Laparotomy with perforation closure using interrupted sutures with or without an omental pedicle to close the defect has been the main approach for several decades.
Laparoscopic repair of perforated ulcers is being used increasingly, recently reaching an incidence of 30-45% of cases. However, the use of laparoscopy varies around the world. A recent US study reported that less than 3% of patients with perforated peptic ulcers were operated on by laparoscopy. Two recent systematic reviews including three clinical RCTs found no difference in mortality or any clinically significant postoperative complications between open and laparoscopic surgery.
A review of the literature describing collected case series showed a small benefit of laparoscopy in reducing postoperative pain and length of hospital stay (and in some cases even reducing mortality), but the results of these reports may be biased towards selection of younger patients, favorable risk estimates (I - II according to the American Society of Anesthesiologists scale), small perforations (<10 mm), as well as short time periods from the onset of the disease to surgery. There is currently no evidence to suggest that laparoscopic surgery is better than open surgery, but there is no evidence that laparoscopy is harmful in patients with sepsis or widespread peritonitis. However, since no difference in mortality has been shown between these techniques, until there is reliable evidence of the superiority of one technique over another, its selection should be guided by the experience of the surgeons performing the operation and the assessment of the patient's condition. Sometimes the perforation may be too large (ie, >2 cm) or the inflamed tissue may be too friable to allow safe healing by primary intention. In addition, if the first attempt to close the defect fails, the second may also fail. In these circumstances, resection may be a safer option. It should be noted that large gastric ulcers or their persistent perforations should raise the suspicion of malignancy, which can be found in almost 30% of patients in this situation. Surgical strategy in such patients may then include resection (distal gastrectomy for gastric ulcer or formal gastrectomy for suspected malignancy), partial gastrectomy with diverting gastrojejunostomy (if the defects are located in the pyloric region) or placement of a T-tube drain, if the defect is in the duodenum. In Japan, some investigators have reported a higher proportion (up to 60%) of patients with perforated ulcers who underwent gastrectomy rather than primary suture, possibly based on tradition and the much higher incidence of gastric neoplasia in Japan. than in North America and Europe.
Table 1: Generalized view of the management of patients with ulcerative disease
| Comments | Base | |
| Prehospital, primary care | ||
| Definition of symptoms, high index of suspicion | Absence of peritonitis in a third of patients. There was no previous history of signs of peptic ulcer in almost half of the patients. Please note that symptoms may vary or be mild in older patients, obese individuals, immunocompromised individuals and children | Observational studies |
| Vital signs monitoring | Detect early signs of systemic inflammatory response syndrome (SIRS) or sepsis by measuring blood pressure, heart rate, respiratory rate and temperature | Surviving Sepsis Campaign (see text) |
| Seek help as soon as possible | Quick connection to the emergency room or hospital. Every hour of delay increases the patient's risk of death | Observational studies |
| Emergency room | ||
| Diagnostics | Exclusively clinical in the presence of generalized peritonitis. Otherwise, CT => X-ray => Ultrasound. Determination of serum lipase to exclude the differential diagnosis of pancreatitis | Observational studies |
| Preparation | Stabilize according to sepsis management guidelines, but keep in mind to minimize surgical delay | Surviving Sepsis Campaign |
| Screening for sepsis | Data allowing a conclusion about the diagnosis of sepsis | Surviving Sepsis Campaign |
| Early intensive care | Prescribing infusion therapy, monitoring vital functions | Surviving Sepsis Campaign |
| Early administration of antibiotics | Blood culture (x2); broad-spectrum antibiotics for intravenous administration | Surviving Sepsis Campaign |
| Making decisions | ||
| Indications for surgery | Patient consent | Common sense |
| Conservative management | Used if: very limited symptoms/defect; the patient's unsuitability for surgery (eg, American Society of Anesthesiologists risk score 5); or the patient's reluctance. Assess the risks and suitability of postoperative intensive care; dialysis; ventilator support | One RCT on conservative treatment; case series; surveillance data with a high risk of discrepancy |
| Surgery | Open or laparoscopic (ready for conversion) (**alternatives to endoscopy) | 3 RCTs showing no difference in outcomes; experimental and sporadic data |
| Palliative care | If the patient is in the terminal stage of the disease | Optimal supportive care; expert opinions, no specific data; observation |
| Preoperative preparation | ||
| Cultures and biopsy | Peritoneal fluid smears, with or without tissue biopsy | Surviving Sepsis Campaign |
| Abbreviated laparotomy | If the patient is in severe shock | Case series |
| Intra-abdominal drainage | No data to support routine use | Observations |
| Postoperative management | ||
| Accelerated Recovery | Quick recovery is possible if the defect is small; providing food at the patient's request, early removal of drainage, early discharge | One small RCT with high risk of discrepancy |
| Helicobacter eradication | Esomeprazole 20 mg twice a day, or omeprazole 20 mg twice a day; amoxicillin 1 g twice a day; clarithromycin 500 mg twice daily | RCTs and meta-analyses |
| Observation (after discharge from the hospital) | Increased delayed mortality, possibly due to common risk factors such as smoking and comorbidities | Some observational studies |
| Control endoscopy | Rules out malignancy of a gastric ulcer if no preoperative biopsy was performed or if the location of the defect is not determined (malignancy of a duodenal ulcer is highly unlikely) | Expert opinions, observational studies |
*This column offers links and is not an exhaustive list. **Cm. Table 2, experimental nature
New treatment strategies for closing perforations
In recent years, new methods have often been used, in particular endoscopic ones. Some approaches represent an alternative between conservative and surgical treatment, such as endoscopic clamping or stenting, but are based on only a small case series (Table 2). Other innovations, such as the use of biodegradable material to cover the ulcer site or mesenchymal stem cells to improve wound healing, have only been evaluated experimentally and have not yet been tested in clinical trials.
Doctors treating the disease
A stomach ulcer requires a qualified, comprehensive approach, so treatment must be carried out in a specialized clinic, where, using modern equipment, research is carried out and a clear diagnosis is established.
For patients who are interested in the question of which doctor treats gastric dysfunction, the answer is clear - this is a gastroenterologist. A specialist conducts examinations and, based on them, prescribes effective treatment methods and surgical intervention for advanced stages of the ulcer. Patients who are disillusioned with general practitioners should contact a gastroenterologist with such a disease, who treats the immediate cause of the disease and helps to overcome the disease without serious consequences for the whole body. A qualified gastroenterologist, based on medical history, causes and symptoms, will determine the nature of the pathology and prescribe appropriate treatment.
Among the many clinics in Moscow where ulcers are diagnosed, one of the leaders is JSC Meditsina. To undergo examination, diagnosis and take appropriate tests, you need to register with a clinic, where you can choose an experienced doctor who will help you effectively and quickly cure the ulcer.
The clinic offers research using modern equipment that allows for color mapping, 3D modeling of tissues and blood vessels, which can be used to examine ulcers and changes in the stomach and gastrointestinal tract in detail, make an accurate diagnosis, and prescribe an effective treatment method. Thanks to high-precision color images, the doctor gets a clear picture of the ulcer.
Doctors at Dr. Roitberg's clinic with many years of experience help overcome the underlying causes, symptoms and manifestations of ulcers, and completely get rid of painful sensations, regardless of how painful the gastrointestinal tract organs are and how the disease progresses.
Possible complications
If the course of ulcer is unfavorable, the following are possible:
Ulcerative bleeding
Occurs in 15-20% of people with peptic ulcer. Accompanied by vomiting that resembles coffee grounds and dark, tarry stools. Other signs of bleeding: weakness, dizziness, tachycardia, decreased blood pressure. May lead to loss of consciousness.
Perforation of the ulcer (perforation)
The phenomenon is observed in 5-15% of people suffering from stomach ulcers. More often in men than in women. It usually manifests itself suddenly, against the background of the absence of symptoms characteristic of peptic ulcer. Characterized by:
- Acute local pain in the epigastric region;
- Painful sensations when palpating the abdomen;
- Tension of the muscles of the anterior abdominal wall.
In the future, it can lead to peritonitis - inflammation of the peritoneum, requiring urgent surgical intervention.
Penetration
That is, the spread of ulcerative damage to neighboring tissues: the pancreas, lesser omentum, gallbladder and common bile duct. In this case, painful sensations lose connection with food intake and become permanent. The temperature rises.
Pyloric stenosis
That is, a narrowing of the opening between the stomach and duodenum. Occurs as a result of unwanted growth of scar tissue. Accompanied by vomiting and belching with the smell of hydrogen sulfide. Sometimes – electrolyte imbalance.
Malignancy
This is the name of the process by which formations become malignant.
Some complications develop in 50-60% of patients.
According to statistics, the likelihood of their occurrence is higher in people with immune disorders. Healing occurs more efficiently and quickly in the absence of immunity problems. That is why treatment of ulcerative gastrointestinal tract is best carried out under the supervision of an immunologist.
Treatment methods
Therapy for the disease should include comprehensive measures.
For the most effective treatment, after diagnosis, the doctor uses antibacterial medications, antispasmodics, prokinetics, medications to stabilize stomach acidity, and the patient is prescribed dietary nutrition if there are problems with the gastrointestinal tract. During the medical treatment of peptic ulcers, antibacterial drugs are used - Metronidazole, Furazolidone; medications that regulate acidity - Kvamatel, Omeprazole. In the absence of complications, treatment of ulcerative pathology is carried out conservatively. Surgical treatment methods and gastroscopy are indicated for certain complications, for example, perforation, bleeding in the gastrointestinal tract and other irreversible pathological or inflammatory processes. Also, medications and treatment methods are prescribed based on the stage of scarring of the walls.
Conservative therapy to combat ulcers takes a leading place and has two main goals:
- cause the death of Helicobacter;
- reduce the acidity of gastric juice to a stable level.
Three-component or four-component regimens can be used, depending on the severity of the inflammatory process.
In parallel, physiotherapy can be carried out (electrophoresis of drugs on the epigastric zone). Therapy mainly includes medication and proper nutrition. Surgery is indicated only for complications. Drug therapy for ulcers involves the prescription of antibacterial agents that help remove bacteria from the body. Treatment is carried out in stages:
- stage one - inhibitors or agents to normalize acidity and reduce the release of hydrochloric acid, are used together with antibacterial drugs based on clarithromycin, from the category of semi-synthetic penicillins. Taking medications lasts an average of a week. The dose and type of medications are prescribed by the doctor solely on the basis of an in-depth examination. If the patient is unresponsive to inhibitors, similar histamine H2 receptor blockers are prescribed. Already at this stage, 90% of patients experience complete elimination of bacteria;
- stage two is required if standard treatment does not bring results. Similar inhibitors are used with antibacterial agents from the group of nitroimidazoles and tetracyclines, and gastroprotectors are introduced. The drugs create a film on the walls of the stomach, which reduces pain, relieves inflammation, increases the resistance of the mucous membrane to negative influences, and restores the protection of the stomach. The duration of the treatment phase is a week or more.
During treatment, the doctor also prescribes concomitant medications aimed at alleviating symptoms: vitamins and medications that protect the mucous membrane from the effects of gastric juice, sedative medications (valerian), antispasmodics to reduce pain, probiotics that help stabilize the normal microflora of the gastrointestinal tract, since it suffers due to taking antibiotics.
An important element of the treatment regimen is the correct diet. You need to eat little and often, 5-6 times a day, without overeating. It is necessary that foods do not require prolonged chewing, since this activates the production of juice in the stomach. For stomach ulcers, it is better to eat purees, soufflés, omelettes, porridges and jelly, cutlets and meatballs, and casseroles.
Based on the stage and characteristics of the disease, the following diets are used:
- Table 1A – for exacerbations of pathology. The diet includes soups in the form of pureed cereals, steam soufflé, soft-boiled eggs, milk porridge, jelly, steamed fish;
- Table 1 – prescribed after exacerbations. Meals include white bread and crackers, vegetable and cereal puree soups, boiled lean meat, steamed fish, cottage cheese casseroles, ground porridge, omelettes, boiled vegetables, and lightly brewed tea. Prohibited are rye bread, meat with fat and streaks, rich broths, spicy and fried foods, marinades, fermented milk products, coffee;
- table 5 – used for remission. Allowed are milk, cottage cheese and low-fat sour cream, steamed cutlets, omelettes and soufflés, boiled and stewed fish, steamed cutlets, crackers and bran bread, and individual vegetables. You should not consume coffee and strong tea, sauces and spices, fatty and fried foods, sour fruits, fresh bread and confectionery, and smoked foods.
Prognosis and prevention
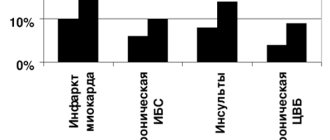
The prognosis for gastric ulcer largely depends on the timeliness of seeking medical help and the effectiveness of anti-Helicobacter therapy. Peptic ulcer is complicated by gastric bleeding in every fifth patient, from 5 to 15% of patients suffer perforation or penetration of the ulcer, and 2% develop cicatricial stenosis of the stomach. In children, the incidence of complications of gastric ulcer is lower - no more than 4%. The likelihood of developing stomach cancer in patients with peptic ulcer is 3-6 times higher than among people who do not suffer from this pathology.
Primary prevention of gastric ulcer includes preventing infection with Helicobacter pylori infection, eliminating risk factors for the development of this pathology (smoking, cramped living conditions, low standard of living). Secondary prevention is aimed at preventing relapses and includes following a diet, avoiding stress, and prescribing an anti-Helicobacter drug regimen when the first symptoms of peptic ulcer appear. Patients with gastric ulcer require lifelong monitoring, endoscopic examination with mandatory testing for H. pylori once every six months. Source: https://www.krasotaimedicina.ru/diseases/zabolevanija_gastroenterologia/stomach-ulcer
Indications for stomach ulcers
Timely treatment ensures effective relief from the disease. Main indications for the treatment of ulcers:
- stop drinking alcohol, eat regularly and properly, exclude fried, fatty, spicy and salty foods;
- prevention of Helicobacter infection - for this it is recommended to follow standard recommendations;
- follow hygiene rules (wash hands before eating);
- wash food before eating;
- use fresh food and throw away spoiled food;
- Wash the dishes well, rinse off any remaining detergent.
Lifestyle in the presence of an ulcer is mainly determined by proper dietary nutrition, which is based on the following provisions:
- frequent and small meals (up to 5-6 times a day), while overeating must be avoided;
- eat enveloping foods, such as oatmeal;
- limit the use of extractive substances;
- give up animal fats;
- eat the portion of foods prescribed by your doctor or nutritionist that contain polyunsaturated fatty acids, which promote rapid healing of ulcers in the stomach and duodenum.
Cost of initial appointment, research, treatment
Prices for medical treatment are shown on the website for patients’ information.
To clarify the current cost of treatment, you need to make an initial consultation with a gastroenterologist, at which the doctor will conduct diagnostic measures and examination, identify the features of the pathology, and prescribe treatment with modern techniques and medications. The price of treatment directly depends on diagnostic measures and therapy, but in each specific case of gastric ulcer the most effective drugs are prescribed depending on the symptoms and stage of the disease. In advanced stages, it is necessary to treat the ulcer with the help of surgical interventions, followed by a hospital stay in the clinic to resolve the worsened manifestations and complications. The clinic offers innovative technologies, detailed analysis and comfortable living conditions.
Classification
Until today, scientists and clinicians around the world have not been able to reach agreement on the classification of gastric ulcers. Domestic experts systematize this pathology according to the following criteria:
- causative factor
– ulcers associated or not associated with H. pylori, symptomatic ulcers; - localization
- ulcer of the cardia, antrum or body of the stomach, pylorus; greater or lesser curvature, anterior, posterior wall of the stomach; - number of defects
- single ulcer or multiple ulcers; - size of the defect
– small ulcer (up to 5 mm), medium (up to 20 mm), large (up to 30 mm), giant (more than 30 mm); - stage of the disease
- exacerbation, remission, scarring (red or white scar), cicatricial deformation of the stomach; - course of the disease
- acute (the diagnosis of gastric ulcer is established for the first time), chronic (periodic exacerbations and remissions are noted); - complications
- gastric bleeding, perforated gastric ulcer, penetration, cicatricial ulcerative gastric stenosis.
Advantages of treatment at the clinic of JSC "Medicine"
JSC "Medicine" (clinic of academician Roitberg) is a multidisciplinary medical center that provides a range of services, including surgery and hospital stays.
Treatment at the clinic of JSC "Medicine" has the following advantages:
- license to carry out medical activities, receive patients, perform operations;
- each doctor has appropriate qualifications and significant experience in domestic and foreign clinics, and their achievements are posted on the medical center’s website;
- high-tech innovative equipment for conducting tests and examinations to establish the true causes of pathological conditions of the gastrointestinal tract;
- cooperation with insurance companies, profitable loyalty programs for corporate clients.
Doctors conduct a thorough and in-depth analysis of the patient’s health status, identify the underlying causes that led to the occurrence of stomach ulcers, and prescribe effective therapy on an outpatient or inpatient basis.