Multiple organ failure syndrome develops as a result of simultaneous or sequential dysfunction of several organs. In most cases, multiple organ failure is the terminal stage of serious diseases, including the last stages of cancer. The term was introduced relatively recently - in 1973 and for more than 45 years it continues to be one of the most common causes of death among patients in intensive care units.
- Features of multiple organ failure
- How does multiple organ failure syndrome manifest?
- Why does multiple organ failure develop?
- Methods for diagnosing the disease
- Treatment of multiple organ failure in Euroonco clinics
- Nutrition for multiple organ failure
- Why is multiple organ failure dangerous?
Features of multiple organ failure
Pathological changes in an organ or organ system do not develop simultaneously. This process occurs in three main stages:
- Compensation. Lasts from three to five days. In response to damage, the body tries to compensate for the lost function. At the initial stages, he manages to do this relatively simply, so a complete failure of the organ does not occur. If treatment is carried out at this stage, it will be possible to avoid serious consequences that are characteristic of other stages.
- Subcompensation. During this period, the body cannot fully replenish the lost function, so the patient needs drug treatment. In order to correct existing disorders, small doses of medications are sufficient.
- Decompensation. This stage is characterized by pronounced changes in organs and complete loss of performance. The patient's condition becomes extremely serious. He needs large dosages of medications and additional measures that are designed to maintain life support (ventilation, hemodialysis).
The severity of multiple organ failure is determined based on the volume of the lesion. Decompensation of two systems corresponds to a severe degree, and of three - to an extremely severe degree.
Classification
Clinicians distinguish two stages of development of multiple organ failure:
- The first is a violation of gas exchange and the blood coagulation system. The amount of bilirubin in the blood increases and the number of platelets decreases. Against this background, there is a deterioration in blood microcirculation. This stage can be considered as the “foundation” of the development of renal, pulmonary, and liver failure;
- the second stage is the stage of decompensation, when irreversible pathological changes occur at the cellular level. In this case, instead of processing carbohydrates to produce energy, the processing of amino acids begins. As a consequence of this, acute heart failure develops and dysfunction of other systems and organs of the patient is observed. The patient falls into a coma.
With complete dysfunction of two organs, death occurs in 30–40%. If there is a disruption or cessation of the functioning of four or more organs, then recovery is almost impossible.
There are also forms of multiple organ failure based on the mechanism of development of the disease:
- single-phase - in the first day after injury, there is a disturbance in gas exchange, which is accompanied by renal, pulmonary and heart failure. In this case, the clinical picture indicates a final complication that leads to death;
- biphasic - after recovery from shock, the patient’s condition can stabilize. Complications result from septic infection, which develops over the next few days. In such cases, there is a small probability that the patient will survive, but subject to correct and timely resuscitation measures.
It would not be entirely correct to consider MODS as an irreversible pathological process. Medicine knows of cases where, with timely resuscitation treatment, it was possible to save a person’s life.
How does multiple organ failure syndrome manifest?
The exact set of symptoms depends on the damage to certain organs. As a rule, the most distinct signs are signs of dysfunction of the respiratory system. This may be evidenced by the following clinical manifestations:
- Dyspnea.
- Activation of accessory muscles during breathing.
- Cyanosis of the skin.
- Severe sweating.
- Impaired consciousness and lethargy in the later stages.
When the cardiovascular system is damaged, chest pain, various hemodynamic disorders, swelling of soft tissues and internal organs are noted. At the initial stage, there is pronounced tachycardia, up to 180 beats per minute. It develops to compensate for disturbances and is eventually replaced by bradycardia, in which the heart rate can drop to 40 beats per minute or even lower. In the later stages, the patient responds poorly to drugs that help normalize the activity of the cardiovascular system. This is one of the reasons why treatment of multiple organ dysfunction becomes difficult.
Disruption of the gastrointestinal tract in multiple organ failure is manifested by symptoms of mechanical compression of the intestine. These symptoms include:
- Violation of the process of defecation.
- Gas retention.
- Bloating and asymmetry of the abdomen.
- Vomit.
- Loss of appetite.
In some cases, gastrointestinal bleeding develops, which aggravates the course of the underlying disease and often causes the death of the patient.
Quite often the clinical picture contains signs that are characteristic of renal failure. First of all, this is a pronounced decrease in urine volume with the subsequent development of anuria, which is an indication for hemodialysis. In addition, patients exhibit a decrease in potassium levels in the blood, renal edema, water and electrolyte imbalance, etc.
Symptoms
The signs and their progress that appear in multiple organ failure are caused by a combination of disorders in the cardiovascular and respiratory systems, as well as dysfunction in the kidneys and liver. They are usually divided into several key conditions:
- functional disorders of the central nervous system;
- respiratory distress syndrome;
- acute liver and kidney failure;
- disseminated intravascular coagulation syndrome (DIC syndrome).
Also, medical specialists have identified four forms of the disease: obvious, hidden (latent), decompensated and terminal. In its obvious form, the toxic syndrome increases. It is accompanied by the progression of blood flow disorders in the liver, kidneys, and skin. The terminal form is characterized by the development of circulatory blockade and ischemia. Metabolites accumulate in human blood, which have a toxic effect on the body and disrupt the excretory function of the liver, kidneys and gastrointestinal tract.
A violation of the biochemical processes of detoxification in the liver is indicated by the presence of ammonia in the blood, and renal failure is indicated by the presence of medium-weight peptides. As for the respiratory system, respiratory distress syndrome develops. The lungs swell, breathing is impaired, and the body does not receive the required amount of oxygen. The patient experiences shortness of breath and an increased heart rate. Symptoms of cyanosis are detected: spots, pallor or blue discoloration of the skin. Extremities become cool.
As for the kidneys, with multiple organ failure syndrome, the risk of oliguria increases, a pathological condition when urine is retained in the body. Parents or caregivers may notice this in a child if he rarely urinates. Since this symptom does not appear only in MODS, it is impossible to make a diagnosis based on this alone. If kidney function is impaired, the content of epithelium, leukocytes and protein in the urine exceeds the norm. Red blood cells may also be detected. As oliguria progresses, anuria occurs, a disease in which urine does not enter the bladder and, as a result, is not excreted from it.
When the liver is damaged against the background of multiple organ failure, cholestatic jaundice develops. Manifestations include: skin itching, which gradually increases, yellowing of the sclera, increased cholesterol and bile acids in the blood, increased bilirubin concentration, decreased number of bilirubin metabolites in feces and urine.
Often, with multiple organ failure, disseminated intravascular coagulation syndrome appears - a disorder of hemostasis caused by deficiency and hyperstimulation of the reserves of the blood coagulation system. It provokes hemorrhagic, microcirculatory and thrombotic disorders. In DIC syndrome, organ dysfunction, bruising in the subcutaneous fat, subcutaneous hematomas, and petechial-hematomal rashes are observed. In acute cases, hypotension, shock, severe bleeding, etc. may develop.
One of the manifestations of MOF in adults and children is increasing acute heart failure. The heart muscle loses its elasticity and ability to contract. As a result, pumping blood becomes much more difficult, leading to stagnation. Progressive AHF may result in pulmonary edema or an asthma attack. Both conditions are extremely life-threatening.
In right ventricular heart failure, the liver becomes enlarged. All tissues and organs are poorly supplied with oxygen, and edema forms. It becomes more difficult for the patient to breathe. From the central nervous system, MOF manifests itself as acute psychosis, lethargy, and sometimes coma.
A common sign of multiple organ failure is duodenal and gastric ulcers. The patient is bothered by pain in the upper abdomen, which gradually intensifies. Heartburn inevitably accompanies a peptic ulcer.
Why does multiple organ failure develop?
Among the reasons that lead to the development of multiple organ failure syndrome are severe diseases and conditions that have a significant impact on the functions of the body. These include severe injuries, sepsis, infectious-toxic shock, etc.
In cancer patients, multiple organ failure syndrome develops after radical tumor removal. A distinctive feature of surgical interventions in oncology is the need to remove part of one or more organs that are affected by the tumor process. Moreover, such operations are often accompanied by massive blood loss, which increases the likelihood of developing the syndrome.
Multiple organ failure develops gradually. There are three main stages in its course:
- Production of various active molecules that lead to the development of a systemic inflammatory response. Such molecules can be interleukins, platelet activation factor, tumor necrosis factor, hormones, enzymes, free radicals, etc. As a result, vascular permeability and tone are disrupted, immune defense mechanisms and the most important biochemical processes are changed. All these changes correspond to the induction phase of multiple organ failure.
- During the cascade phase, the development of systemic damage is noted, which is manifested by characteristic symptoms - thrombocytopenia, leukocytosis, microcirculation disorders, hypoxia, etc.
- The phase of secondary autoaggression is characterized by severe organ dysfunction and disruption of homeostasis.
Multiple organ failure is characterized by several damaging mechanisms, among which the leading ones are ischemia, active thrombus formation and cerebrovascular accident.
Treatment
Complex treatment of multiple organ failure is based on seven main principles. The first is aimed at eliminating the disease or provoking factor that activates and maintains an aggressive effect on the patient’s body. Usually this is a highly invasive infection, purulent destruction, pulmonary hypoxia, severe hypovolemia, etc. If the etiological factor is not eliminated, treatment of MODS is ineffective.
The second principle of the strategy to combat MODS is replacement or artificial maintenance of a vital system (if its operation is not improved, death may occur). These include the circulatory and respiratory systems.
The third principle is antimediator effect. Specialists block endothelial cell receptors with their antagonists using monoclonal antibodies against IL-1, TNFa.
The fourth principle is aimed at normalizing the energy balance. It includes many points, including those presented below.
- Adequate parenteral, mixed, enteral nutrition.
- Metabolic correction is the creation of a normal acid-base balance, without which the performance of enzymes involved in energy production is reduced.
- Drug antioxidant and antihypoxic therapy.
- Introduction of necessary amino acids and vitamins to normalize enzyme activity.
- Normalization of the microcirculatory system and lung function for adequate oxygen supply to tissues.
The fifth principle is effective stimulation of natural detoxification. Extracorporeal methods can also be used - influencing the human body without medicinal or instrumental penetration into the body. These are, first of all, various physiotherapeutic procedures, hemosorption, dialysis, hemofiltration, plasmapheresis, therapeutic massage, etc. These methods should be used until the functions of the internal organs are restored and the body is able to independently maintain homeostasis. In addition, the treatment complex includes methods of functional support of life support organs: artificial ventilation (ALV), pacemaker, vasopressors and cardiotonic drugs.
The sixth principle involves syndromic treatment. Components of multiple organ failure in the form of respiratory distress syndrome, acute hypovolemia, coma, disseminated intravascular coagulation syndrome, acute liver or kidney failure require a set of methods aimed at maintaining or artificially replacing certain functions of the organ and system.
Reducing the invasiveness of actions is the seventh principle of MOF treatment. It takes into account that the invasiveness of modern technologies used in medicine often leads to the development of iatrogenic multiple organ failure.
Methods for diagnosing the disease
Symptoms of multiple organ failure may be similar to other diseases, so to confirm the diagnosis, the doctor prescribes a comprehensive examination, which includes the following diagnostic methods:
- Examination of the patient, analysis of complaints, collection of anamnesis. Already at this stage, a specialist can notice characteristic signs that indicate damage to one or more organs. These may be disturbances in respiratory and cardiac activity, metabolic changes, and deviations in hemodynamics.
- Instrumental examination. Its volume depends on the manifestations of multiple organ failure. The doctor has all non-invasive methods at his disposal, for example, ultrasound, X-ray, CT, MRI, etc. In addition, it is important to regularly monitor the body’s vital signs - blood pressure, heart rate, respiratory rate, etc.
- Laboratory diagnostic methods. Usually, basic tests are prescribed that allow one to evaluate and further monitor the main indicators of hemodynamics, the level of electrolytes and enzymes in the blood, etc.
Taking into account the fact that patients in most cases are in an intensive care unit, multiple organ failure can be detected in the early stages, when complete failure of the organ or system has not occurred.
Multiple organ failure syndrome (MODS) is a natural outcome of critical conditions such as severe concomitant trauma, eclampsia, sepsis, hemorrhagic, toxic-infectious shock, asystole, coma caused by meningoencephalitis, diabetes, and various poisonings. Despite the obvious successes in the development of resuscitation, mortality in patients who have suffered critical conditions complicated by MODS remains very high and, according to different authors, ranges from 35% to 70%, with no tendency to decrease.
In this regard, the following tasks have been set: determining the main mechanisms of development of MODS in various critical conditions and developing an intensive care (IT) strategy.
We believe that the development of multiple organ failure syndrome is based on an acute decrease in metabolism and energy production as a result of metabolic disorders and microcirculation in tissues and organs with subsequent disruption of their function and structure. In the mechanisms of development of MODS, we attach great importance to damage to cellular and vascular membranes by various pathological factors (severe trauma, inflammatory diseases, products of impaired metabolism, products and activators of LPO, toxic agents, etc.), which initiate a complex of pathological changes in cellular structures both at the site of exposure , and at the level of formation of adaptation mechanisms (hypothalamus, pituitary gland, adrenal cortex).
As a result of damage to cellular and vascular membranes, the process of transport and utilization of energy substrates and oxygen is disrupted. Energy deficiency states arise, called hypoergosis,
We first encountered the concept of hypoergosis (energy deficiency of the body) in the work of S.N. Efuni and V.A Shpector (1986). By energy deficiency, the authors understand the discrepancy between the body's (tissue, organ, cell) need for energy and the limited amount of macroergs (ATP) that can currently be used to maintain the structural integrity and functional activity of a tissue or organ.
It is known that energy deficiency is the outcome of almost any pathological process, including those that have reached a critical level, when multiple organ failure occurs associated with the depletion of the cell’s energy resources and the extreme form of tissue hypoxia (Seccha R.V. 1987), S.N. Efuni and V.A. Shpector (1986), considering the problems of energy deficiency, raise the question of the need to revise existing ideas about hypoxic conditions and, in particular, tissue hypoxia. As the authors note, not all hypoergosis is a consequence of oxygen deficiency alone - hypoxia. It can occur when there is a lack of oxidation substrates in the cell (substrate hypoergosis) or inhibition of cell enzymes (enzymatic hypoergosis) with normal or even increased tissue pO2.
Thus, the solution to the problem of MODS should be considered from the standpoint of energy-deficient states.
Diagnosis of MODS was carried out using routine clinical and paraclinical methods. Lung distress syndrome was identified by increasing cyanosis, tachypnea, tachycardia, hard breathing during auscultation and the appearance of moist rales in subsequent stages, and a decrease in pO2. X-ray revealed an increase in the vascular component of the pulmonary pattern with the appearance of focal shadows of the “snow storm” type V against its background. Insufficiency of the cardiovascular system was assessed according to central hemodynamics, electrocardiography, and rheocardiography. Liver failure was assessed by increasing bilirubinemia, hyperenzyme AST, ALT, decrease in prothrombin, fibrinogen, total protein in the blood, increasing toxic encephalopathy. Renal failure was assessed by a decrease in diuresis, specific gravity of urine, increase in urea, and creatinine in the blood. Acute cerebral insufficiency was diagnosed based on neurological status, electroencephalography, and mapping of various functional areas of the brain. It should be noted that quite often - in 40% of cases, MODS was accompanied by DIC syndrome, manifested by an increase in blood clotting time, thrombocytopenia, and the appearance of fibrin degradation products.
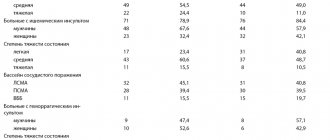
We observed 54 patients who underwent various surgical diseases complicated by MODS. 6 patients with severe combined craniocerebral and polytrauma, 10 patients with hemorrhagic shock, 7 patients with infectious-toxic shock and 31 with purulent-inflammatory diseases of the abdominal and thoracic cavity.
Multiple organ failure syndrome was diagnosed when two or more organs and systems were affected.
The IT strategy was built on the basis of the identified pathogenetic patterns of the occurrence of MODS. The primary task, in our opinion, is to try to restore the energy production of the body's cells and restore the impaired function of cellular and vascular membranes; this task is fully met by our proposed method of combined use of the antihypoxant olyphene, which improves the transport and utilization of glucose and oxygen, as well as lipin, which restores the integrity of cellular and vascular membranes. Olifen was used in a dose of 280 v 420 mg. per day by slow intravenous drip of 5% glucose or 0.9% NaCl solution. Lipin was used intravenously at a dose of 2 v 4 g. per day, and through ultrasonic inhalations and instillations into an endotracheal or tracheostomy tube.
It should be emphasized that 18 patients (33%) with MODS received respiratory support in the form of mechanical ventilation, the indications for which were increasing signs of hypoxia and ineffective spontaneous breathing (a decrease in blood oxygen saturation below 85%). Ventilation was carried out using respirators of the Phase v5 type, or respirators of the RO family in mode of moderate hyperventilation, more often with PEEP. The duration of mechanical ventilation in this group of patients was:
up to a day v 4 patients (7%) from 1 to 3 days v 21 patients (40%) from 3 to 7 days v 24 patients (44%) from 7 to 18 days v 5 patients (9%)
In 8 patients with obvious signs of distress syndrome, a tracheostomy was cannulated to improve the drainage function of the lungs and taking into account the expected duration of mechanical ventilation. In 7 patients with purulent bronchopulmonary complications, HF mechanical ventilation was required using the Spiron 601 device, which made it possible to significantly facilitate the sanitation of the tracheobronchial tree and the transfer of patients to spontaneous breathing.
In the absence of direct contraindications, 43 patients (79%) included HBOT sessions in the complex of measures aimed at reducing hypoxemia and improving microcirculation.
It should be noted that there cannot be standard approaches to IT in patients with MODS. Thus, persistent cardiovascular failure in a number of cases (9 patients) required not only full replenishment of the volume of blood volume (central venous pressure level), but also long-term (up to 7 days), dosed (DASH device - 20) administration of adrenergic agonists (dopamine, mesaton, norepinephrine) and megadoses of glucocorticoids (prednisolone, dexazone, hydrocortisone). Water-electrolyte, protein and carbohydrate metabolism were corrected with standard infusion media: solutions of 5% and 10% glucose, saline solution, lactasol, mafusol, disol, albumin and native plasma.
The rheological properties of blood and microcirculation were improved with the help of rheopolyglucin and disaggregants (trental, chimes, nicotinic acid).
Detoxification involved the introduction of hemodez and forced diuresis with saluretics. With obvious signs of increasing intoxication (clinical picture, intoxication index above 7), extracorporeal detoxification methods were used - plasmapheresis in 27 patients and hemosorption in 4 patients with SKN-type sorbents. In 3 patients, surgical sanitation of foci of infection was required (opening of abdominal abscesses and drainage of the pleural cavity).
Treatment of manifestations of liver failure was carried out using standard methods (glucose solutions, vitamin therapy, Essentiale, Corsil, etc. In severe cases, hormone therapy with glucocorticoids. Liver failure was noted in 18 patients, which amounted to 33% of all patients. Nephropathies of various degrees were identified in 11 patients, and acute renal failure in 5 patients. The ineffectiveness of conservative treatment methods forced ultrafiltration in 4 patients, and hemodialysis in 2 patients (with the SHD v 1 v UB device).
Almost all 54 patients with MODS required antibiotic therapy. The optimal prescription is to prescribe antibiotics taking into account the bacteriogram. However, the urgency of the situation most often forced preventive, as early as possible, prescription of two antibiotics without taking into account sensitivity. Preference was given to semisynthetic penicillins with clavulanic acid (amoxiclav) and aminoglycosides. III generation cephalosporins were also used preventively. Analysis of bacteriograms made it possible to identify the special virulence of staphylococcus, Pseudomonas and Escherichia coli, Proteus, sensitive to fluoroquinolones, carbopinems, aminoglycosides, and dioxidine.
Severe TBI, polytrauma with manifestations of shock in 8 patients required active prevention of fat embolism - adequate anti-shock therapy, effective pain relief, improvement of blood rheology and specific therapy with lipostabil. Correction of immunodeficiency was carried out with gamma V globulin, antistaphylococcal plasma, and immunofan.
In 41 patients (75%), efferent methods of influencing the cellular composition of the blood and its rheology were used. Ultraviolet irradiation of blood was carried out using an Izolda-type apparatus, laser irradiation of blood was carried out using an ALOC-1 apparatus.
We observed positive dynamics in the resolution of MODS with a tendency towards normalization of the listed clinical and paraclinical parameters already by the end of the first day of IT. In the most severe cases it had to be carried out for 1.5 - 2 weeks. It should be noted that only in three cases, when using the IT technique described by us in patients with MODS, secondary septic complications arose.
This approach made it possible to begin prosthetics of impaired vital functions at the earliest possible time and prevented the development of irreversible multiple organ lesions. The implementation of this approach in practice shortened the duration of MODS, prevented the development of fatal complications, and reduced mortality.
Treatment of multiple organ failure in Euroonco clinics
Treatment of multiple organ failure should be comprehensive and carried out in an intensive care unit.
The main goal of patient treatment is to restore lost functions, eliminate the negative consequences of multiple organ failure and prevent complications. For this purpose, medications from the group of antibiotics, NSAIDs, hormones, anticoagulants, etc. are prescribed. If necessary, transfusions of blood or its components are performed, and prevention of disseminated intravascular coagulation syndrome, internal bleeding, and collapse is carried out. Throughout the treatment, the patient must maintain strict bed rest.
Multiple organ failure syndrome often requires replacement of the functions of vital organs that cannot cope with their work. For this purpose, artificial ventilation, renal replacement therapy, and various methods of maintaining cardiac function are used.
The leading cause of multiple organ failure is sepsis, an overreaction of the immune system to infectious agents, resulting in pockets of inflammation throughout the body. This condition often occurs in cancer patients. In this case, an important part of the treatment is antibacterial and infusion therapy. Euroonko clinics successfully use a modern technique - selective sorption on cartridges for extracorporeal hemoperfusion Toramyxin PMX-20R. With its help, the patient's blood is cleared of endotoxin in cases of infections caused by gram-negative and mixed flora.
In severe cases, surgical methods are used. These include extracorporeal detoxification, elimination of intestinal obstruction, and removal of non-viable organs that have begun to become necrotic.
The intensive care unit at the Euroonco clinic has all the necessary equipment for constant monitoring and maintenance of vital functions. We use equipment from leading brands; the rooms are equipped with a centralized oxygen supply system. All the necessary medications of the latest generations are always available. Our capabilities allow us to admit a patient on an emergency basis and immediately begin providing all necessary types of medical care.
Causes
Multiple organ failure can result from tissue hypoperfusion or hypermetabolism, various injuries and infections. As for cellular changes, the influence of mediators plays a major role in them. Their quantity during release depends on the severity of the factor provoking the damaging effect.
In some cases, the cause of multiple organ failure is a transfusion of canned blood that has been stored for a long time (especially in large quantities). Sometimes this condition is preceded by unskilled artificial ventilation. In the field of surgery, infectious complications are a key cause of the body's stress response. They cause disruption of the patient's homeostasis and metabolism system. In 7–22% of cases, multiple organ failure occurs in the postoperative period. In 50% of cases, the diagnosis is made due to purulent complications of acute inflammatory pathologies.
Multiple organ failure can result from impaired immunity and septic processes. In most situations, sepsis begins due to exposure to gram-negative bacteria that enter the organs and bloodstream through the gastrointestinal tract.
Nutrition for multiple organ failure
With multiple organ failure syndrome, the patient's body needs an increased amount of energy. Energy consumption increases 2–3 times compared to the norm. At the same time, the state of the digestive system does not allow the full absorption of nutrients. Therefore, feeding is carried out with special mixtures through a tube or intravenously. Gradually, as you recover, you are allowed to switch to normal food, initially in small portions.
Nutrition should be complete and balanced. The patient's body needs a sufficient amount of protein, vitamins, microelements, and antioxidants. In this case, mixtures with a low glycemic index are used to prevent the development of insulin resistance and diabetes mellitus.
Symptoms
With MODS syndrome, the following clinical picture is observed:
- breathing problems, shortness of breath;
- rapid or rare pulse;
- pallor, yellowing or blue discoloration of the skin;
- feeling of coolness in the lower and upper extremities;
- signs of oligo- or anuria (fluid retention in the body);
- yellow sclera and other visible mucous membranes;
- itching of the skin, which gradually increases;
- formation of subcutaneous hematomas and bruises;
- symptoms of acute heart failure;
- signs of dyspeptic disorders;
- lethargy.
It should be noted that it is not always possible to observe the full manifestation of the clinical picture of MODS. Depending on the etiological factor and the general condition of the patient, at any stage of development of complications, both coma and death can occur.
Why is multiple organ failure dangerous?
The main danger of multiple organ failure is the high risk of death. Depending on the extent of the lesion, mortality can range from 30% to 100%. Even if the main manifestations of the syndrome can be eliminated in a timely manner, the likelihood of developing delayed diseases remains very high. Among the most common complications are:
- Chronic renal failure.
- Cardiac ischemia.
- Various lung diseases.
- Blockade of the cardiac pathways.
- Neurological disorders.
- Encephalopathy, etc.
Despite the development of methods of surgical treatment and systems for monitoring key indicators of the body during surgery, as well as approaches to postoperative patient management, the incidence of multiple organ failure continues to remain high. Due to the relevance of this problem, experts are looking for new ways to solve it, ranging from timely diagnosis to effective treatment.
| More information about treatment at Euroonco: | |
| Palliative care in Moscow | from 44300 per day |
| Emergency oncology care | from 12100 rub. |
Book a consultation 24 hours a day
+7+7+78
Prevention and prognosis
Preventing the body's stress response is a very real task. This requires timely diagnosis to avoid any existing disease from becoming critical. To implement such a preventive scheme, monitoring and functional assessment, normalization of blood circulation, elimination of infections, normalization of breathing and metabolism, provision of energy expenditure (nutrition), as well as early treatment of injuries, inflammation and necrosis are necessary.
The prognosis for the development of multiple organ failure depends on the severity and nature of the accompanying complications. When three or more organs and systems are affected, the patient’s death occurs in 70% of cases. When the function of two organs is impaired for more than a day, death occurs in 55% of patients. When one organ is affected - in 35% of cases.
Diagnostics
Diagnosis, in this case, is purely individual, since everything depends on the current condition of the patient. Urgent resuscitation is often required to stabilize the patient's condition.
Diagnostic methods depend on the current symptoms of organ failure. The following must be carried out:
- general and biochemical blood test;
- general urine analysis;
- coprogram;
- CT, MRI;
- Ultrasound of internal organs;
- HIV test.
Treatment will depend on the identified disorder, the underlying factor, and the patient's current condition. Quite often, if MODS is diagnosed in the second stage of development, only maintenance therapy is carried out.