Pharmacodynamics and pharmacokinetics
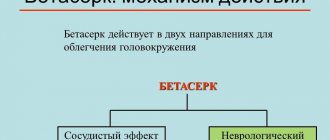
The mechanism of action of the drug has been partially studied; there are several hypotheses in this regard. Betahistine is a synthetic analogue of histamine , acts on H1 receptors , is an antagonist of H3 receptors , and exhibits insignificant activity towards histamine H2 receptors . The active substance improves blood circulation in the vessels of the inner ear by relaxing the sphincters in the microcirculation system of the inner ear . The drug can also increase blood flow in the basilar arteries .
Vestinorm tablets promote vestibular compensation, accelerate the process of restoration of vestibular function, by regulating metabolic processes in the release of histamine . The effectiveness of the drug has been proven in studies on patients with vestibular disorders and Meniere's disease. This group experienced a decrease in the frequency and severity of attacks.
After taking the tablets, the active substance is quickly absorbed into the gastrointestinal tract . Betahistine then metabolized to form the metabolite 2-pyridylacetonic acid . When taking the medicine with food, the plasma concentration of the metabolite is slightly lower than when taken on an empty stomach, and the absorption process from the gastrointestinal system slows down. The metabolite reaches its maximum concentration an hour after taking the drug. The half-life is 3 and a half hours. 2-pyridyl acetone acid is excreted mainly in the urine, a small amount is excreted in the feces and through the kidneys.
blood plasma proteins is very small - about 5%.
Pharmacological properties of the drug Vestinorm
betahistine (N-methyl-2-(pyridin-2-yl)ethanamide dihydrochloride) is a drug used for vestibular disorders (dizziness). A synthetic analogue of histamine, has a histamine-like effect. The drug is a partial agonist of histamine H1- and antagonist of H3-histamine receptors of the inner ear and vestibular nuclei of the central nervous system. Improves microcirculation and permeability of the capillaries of the inner ear, increases blood flow in the basilar arteries, normalizes endolymph pressure in the labyrinth and cochlea, transmitter transmission in the neurons of the medial nuclei of the vestibular nerve at the level of the pons of the brain stem. As a result, disorders of the vestibular apparatus and cochlear disorders are normalized, the frequency and intensity of dizziness is reduced, noise and ringing in the ears are reduced, and hearing improves. Improvement in the condition of acute vestibular disorders is noted already in the first days of treatment with the drug. A stable therapeutic effect is achieved within 2 weeks of taking the drug and can increase when taking the drug for several months. Being a blocker of H3 receptors in the nuclei of the vestibular nerve, it exhibits a pronounced central vasodilator effect. After oral administration, it is quickly and almost completely absorbed from the gastrointestinal tract. The maximum concentration in blood plasma is achieved 3 hours after administration. Protein binding is low. Passes through histohematic barriers. The half-life is 3–4 hours. Metabolized in the liver to 2-peridylacetic acid, which is almost completely excreted from the body in the urine within 24 hours.
Indications for use
Vestinorm is prescribed for illness and Meniere's syndrome , which are accompanied by dizziness, nausea, tinnitus, vomiting and hearing loss . Tablets are also used to eliminate the symptoms of vestibular dizziness in various diseases ( post-traumatic encephalopathy , dizziness after operations in ophthalmology and neurosurgery , vertebrobasilar insufficiency , vestibular neuritis , labyrinth , cerebral atherosclerosis
Pharmalogical Action.
A histamine-like agent that improves microcirculation. The active ingredient of Vestinorm is betahistine dihydrochloride. Vestinorm is a synthetic analogue of histamine, an antagonist of H3 histamine receptors and a partial agonist of H1 histamine receptors of the vestibular nuclei and inner ear. The drug has the ability to block the process of breakdown of endogenous histamine and restore normal neuronal transmission in the neurons of the medial nuclei of the vestibular nerve at the level of the brain stem. Vestinorm is able to inhibit the enzyme diamine oxidase and have an effect on precapillary sphincters. The drug in the basilar arteries increases blood flow and normalizes endolymph pressure in the cochlea and labyrinth. As a result, cochlear disorders and disorders of the vestibular apparatus are normalized, ringing and noise in the ears are reduced, the intensity and frequency of dizziness attacks are reduced, and hearing improves. In case of acute vestibular disorders, improvement is noted already within the first day of therapy with Vestinorm. Within two weeks of using the drug, a stable therapeutic effect is achieved, which can increase with continued therapy with the drug for several weeks. Due to the ability to block H3 receptors of the vestibular nerve nuclei, Vestinorm has a central vasodilator effect. After oral administration, Vestinorm is quickly absorbed from the digestive tract and reaches its maximum concentration in the blood after 3 hours. The drug is characterized by a low ability to bind to blood proteins. Vestinorm penetrates all histohematic barriers. The half-life of the drug is 4 hours. In the liver, Vestinorm is metabolized to 2-peridyl-acetic acid, which is excreted by the kidneys during the day.
Indications for use
Vestinorm is prescribed for the treatment of Meniere's disease (and syndrome), relief of syndromes and conditions characterized by dizziness, including vestibular dizziness of various origins (vertebrobasilar insufficiency, post-traumatic encephalopathy, vestibular neuritis, cerebral vascular atherosclerosis, labyrinthitis, benign positional dizziness after ophthalmological and neurosurgical surgeries and etc.).
Mode of application
Vestinorm is recommended to be taken after meals or during meals, without chewing.
The drug is prescribed to adults three times a day, 8-16 mg. The daily dose of Vestinorm is 24-48 mg. Depending on the effect of treatment, the duration of therapy with Vestinorm and the dose of the drug should be determined by the doctor individually. Side effects Vestinorm is well tolerated in most cases. Minor disturbances in the digestive tract (feeling of heaviness in the epigastric region, nausea), headaches may occur. These disorders usually go away when the dosage of the drug is reduced or when used with food. In extremely rare cases, when using Vestinorm, allergic reactions (urticaria, itching, skin rashes) may occur.
Contraindications
Vestinorm is contraindicated for peptic ulcers (in active form), bronchial asthma (during exacerbation), pheochromocytoma, hypersensitivity to the components of the drug.
Pregnancy
There is insufficient data on the safety of using Vestinorm during pregnancy.
Drug interactions
Simultaneous use with antihistamines (tavegil, suprastin, fenkarol, zyrtek, kestin, xyzal, etc.) leads to a decrease in the effectiveness of Vestinorm.
Overdose
In case of an overdose of Vestinorm, disturbances from the gastrointestinal tract (vomiting, nausea), and headache may occur. There is evidence of the appearance of convulsive paroxysms when taking the drug at a dose exceeding 728 mg. Treatment of overdose: gastric lavage, symptomatic therapy.
Release form
Vestinorm tablets 8 mg, 30 tablets. packaged. Vestinorm tablets 16 mg, 30 tab. packaged.
Storage conditions
Vestinorm should be stored at a temperature not exceeding 25 degrees Celsius. Protect from light and moisture. Keep away from children.
Compound
1 tablet of Vestinorm contains: 8 mg (16 mg) of betahistine dihydrochloride. Excipients: microcrystalline cellulose 101, aerosil, sodium starch glycolate, magnesium stearate, medical low molecular weight polyvinylpyrrolidone 12600±2700. Attention! The description of the drug on this page is simplified. Before purchasing and using the drug, consult your doctor or pharmacist, and also read the instructions approved by the manufacturer. Information about the drug is provided for informational purposes only and should not be used as a guide to self-medication. ATTENTION! This section is provided for informational purposes only and is not a catalog or price list of our company. To obtain information about the availability of drugs, call + 99871 202 0999 Pharmacy Network Helpline 999.
Side effects
As a rule, the drug is well tolerated. The most common symptoms are discomfort in the stomach, nausea, and headache.
There are also known cases of flatulence , bloating , allergic reactions , anaphylaxis , angioedema , rashes and itching
5, hives.
By taking the medication with food and reducing the daily dosage, some of the side effects go away.
Research results and their analysis
Before the start of therapy with Vestinorm and Betaserc, as well as during treatment on the 3rd, 7th and 14th day of taking the drugs, the neurological status of the patients was assessed. In particular, special attention was paid to the presence of symptoms such as: 1) nystagmus; 2) hearing impairment; 3) somatosensory disorders (feelings of unsteady soil underfoot, falling through, rocking on the waves, walking over bumps); 4) autonomic disorders (pallor, sweating); 5) oculomotor disorders; 6) disturbance of balance and coordination of movements during the Romberg test. Data on the dynamics of the distribution of patients according to the presence of the above symptoms during 2-week therapy with the study drugs are given in Table. 2 (ordinal numbers of pathological neurological symptoms correspond to those listed above).
As can be seen from table. 2, before the start of treatment, the clinical picture of the disease in the main and control groups was similar: pathological neurological symptoms such as nystagmus (66.67% of patients in both groups), hearing impairment (30.95% in the main group and 33.33% in both groups) were observed. - in the control group), somatosensory pathological symptoms (feelings of unsteady soil underfoot, falling through, swaying on waves, walking over bumps) (76.19% of patients in the main and 71.42% in the control groups), autonomic disorders (pallor, sweating) - 59.52% of patients in both clinical groups. Oculomotor disorders were observed in 23.81% of patients in the study group and 19.04% in the control group; impaired balance and coordination of movements during the Romberg test were observed in 85.71% and 83.33% of patients in the study and control groups, respectively. Thus, before the start of therapy with both drugs, the clinical picture of the disease in patients was dominated by disorders of balance and coordination of movements, pronounced somatosensory and autonomic disorders, and horizontal nystagmus (Table 2).
During 2-week therapy with Vestinorm and Betaserc, there was a gradual and approximately equal decrease in both groups in the main clinical and neurological manifestations of dizziness in vertebrobasilar insufficiency. Thus, on the 3rd day of taking the drugs Vestinorm and betaserc, there was a tendency to reduce the number and severity of pathological somatosensory and autonomic disorders, and horizontal positional nystagmus was detected somewhat less frequently (Table 2). By the middle of the course of treatment with both drugs (7th day of taking Vestinorm and Betaserc), there was a more significant decrease in these pathological symptoms and a slight decrease in the number of patients with hearing impairment and statodynamic disorders using the Romberg test (Table 2).
At the end of therapy with Vestinorm and Betaserc, a significant decrease in the frequency and severity of pathological somatosensory disorders was observed: they were observed only in 16.67% of patients in the main group and 19.04% in the control group. The same pronounced dynamics were observed in relation to the relief of autonomic disorders (decrease to 14.28% in both groups by the end of treatment) and static-dynamic disorders according to the Romberg test (35.71% of patients in the main group and 33.33% in the control group). By the end of treatment, horizontal positional nystagmus was also relieved quite well, which on the 14th day of therapy persisted only in 14.28% of patients in the main group and 16.67% in the control group. To a somewhat lesser extent, the studied drugs affected hearing impairment: by the 14th day of therapy, they were noted in 16.67% of patients receiving Vestinorm and 14.28% of patients receiving Betaserc. The study drugs had the least effect on pathological oculomotor disorders, which by the end of therapy continued to be observed in 19.04% of patients in the main group and 16.67% in the control group (Table 2).
Thus, both drugs compared had an equally pronounced positive effect on the main clinical and neurological manifestations in patients with dizziness due to vertebrobasilar vascular insufficiency. Vestinorm and betaserc had the greatest effect on pathological somatosensory and autonomic disorders, horizontal nystagmus, static and dynamic ataxia in the Romberg test. Other pathological clinical and neurological manifestations of dizziness against the background of chronic vertebrobasilar vascular insufficiency also tended to decrease, but this dynamics was less pronounced.
During the clinical study, the daily frequency of dizziness attacks in patients of both groups ranged from 8 (maximum value) to their complete absence (Table 3). The dynamics of the distribution of patients according to the frequency of dizziness attacks per day during 2-week therapy with Vestinorm and Betaserc are presented in Table. 3, the average number of attacks per day at different stages of treatment in the main and control groups - in table. 4 and in Fig. 1.
As can be seen from table. 3, 4, before the start of treatment with the compared drugs, the frequency of dizziness attacks was: in the main group - from 2 to 8 per day (median - 7 attacks per day), or on average for the group 6.78 ± 1.55; in the control group - from 3 to 8 per day (median - 7 attacks per day), or on average for the group 6.69 ± 1.40.
Before starting therapy, the majority of patients in both groups reported having very frequent attacks of dizziness: 7 attacks per day - in 30.95% of patients in the main and 26.19% in the control groups, 8 attacks per day - in 42.95 and 38. 09% of patients in both groups, respectively (Table 3).
From the first days of taking Vestinorm and Betaserc, there was a gradual decrease in the daily frequency of dizziness attacks. Thus, on the 3rd day of treatment, the average frequency of dizziness attacks in the main group was 5.92 ± 1.31 attacks, in the control group - 5.90 ± 1.44 (Table 4, Fig. 1). By the 7th day of treatment with both drugs, a decrease in the average number of attacks was recorded to 3.76 ± 1.14 in the main group and 3.55 ± 1.36 in the control group (Table 4, Fig. 1). Also, by the middle of treatment with the study drugs, the spectrum of distribution of patients in terms of the number of dizziness changed - with a maximum of 4-5 attacks per day in both groups (Table 3). After the 7th day of taking the drugs, 11.9% of patients in the main group and 14.28% of patients in the control group noted days without dizziness.
At the end of the 2-week course of treatment, a significant and equally pronounced reduction in the daily frequency of dizziness attacks was noted in both groups (Fig. 1): all patients reported having no more than 4 attacks, while the absence of attacks was noted in 2.38% of patients in the main and in 4.76% - in the control group, 1 attack per day - in 1 patient (2.38%) receiving betaserc, 2 attacks per day - in 9.52% of patients in the main group and 14.28% in the control group (Table 3). By the end of the course of treatment, most patients experienced no more than 3 (73.81% of patients in the main and 76.19% of patients in the control groups) or 4 (26.19 and 23.81% of patients in both groups, respectively) attacks of dizziness (Table 3 ). Thus, the maximum value of the frequency of attacks at the end of treatment is 4, the minimum is 0 (no attacks), the median is 3 attacks per day in both groups.
By the end of the course of treatment, the average frequency of dizziness attacks in patients taking Vestinorm decreased to 3.09 ± 0.76 attacks per day. Quantitatively similar dynamics were observed in the group of patients taking betaserc, in which the frequency of dizziness decreased to an average of 2.90 ± 0.96 attacks per day (Table 4, Fig. 1). On average, the frequency of dizziness attacks by the end of treatment in the main group decreased by 3.69, in the control group - by 3.79 per day (Table 4), which reflects the high effectiveness of the drugs in relieving dizziness attacks due to chronic vertebrobasilar insufficiency.
To check the statistical significance of the differences between the frequency of dizziness attacks before and after treatment with the study drugs, we used the paired Student's test. A prerequisite for the application of this criterion was to check compliance with the normal distribution law of individual differences using the Shapiro-Wilk test with a significance level of 0.01. Individual differences were subject to the normal distribution law, so the application of the Student's test in this case turned out to be correct. The value of the paired Student's test in the main group was 2.13, in the control group - 2.22, which exceeds its critical values for these degrees of freedom (2.02) at a significance level of 0.05 and allows us to conclude that the differences between the frequency of dizziness before and after treatment with study drugs. Thus, with 14-day therapy with the study drug Vestinorm, as well as with treatment with the reference drug betaserc, there is a significant decrease in the frequency of dizziness attacks in patients with vertebrobasilar vascular insufficiency.
In 27 (64.29%) patients of the main group, a significant effect of the study drug Vestinorm on the frequency of dizziness attacks was noted at the end of the 14-day course of treatment: relief of attacks in 1 patient (2.38%) with an initial 2 attacks per day and a decrease in the number of attacks by 50% or more - in 26 (61.90%) patients. In 18 (42.86%) patients with an initial 8 attacks and in 6 (14.28%) with an initial 7 attacks, their frequency decreased to 3 by the end of the study. In another 2 patients (4.76%) with an initial 7 attacks their the frequency decreased by the end of treatment to 2 per day. Thus, in these 27 patients (64.29%), the effectiveness of Vestinorm can be assessed as high in this indicator.
In 11 patients (26.19%), the frequency of dizziness by the end of therapy with Vestinorm decreased by 25–49% from the initial values: in 2 patients (4.76%) with 5 initial attacks per day, their frequency decreased to 3, in 2 (4 .76%) with 3 attacks - up to 2, in 2 (4.76%) with 6 initial attacks - up to 4 and in 5 patients (11.90%) with 7 attacks - up to 4. That is, the effectiveness of Westinorm in these 11 (26.19%) of patients was assessed as moderate.
In 4 (9.52%) patients with an initial 5 attacks of dizziness per day, their frequency by the end of Westinorm therapy decreased to only 4 (less than 25%), which made it possible to assess the effectiveness of therapy in them as low.
In the control group, 28 (66.67%) patients experienced complete relief of dizziness attacks by the end of the course of treatment: in two patients (4.76%) with the initial 6 attacks per day, and in 26 (61.90%) patients the frequency of attacks dizziness decreased by more than 50%. Among them, in 20 (47.62%) patients with a high (6–8) frequency of attacks, their number decreased to 3 per day, of which initially one patient (2.38%) had 6 attacks per day, 16 (38 .09%) - 8 and 3 (7.14%) - 7 attacks per day. In 5 (11.90%) patients with an initial 7 attacks, their frequency decreased to 2, and in another patient (2.38%) with 6 attacks, their frequency decreased to one per day. Thus, the effectiveness of betaserc in these 28 patients (66.67%) can be assessed as high in this indicator.
In 9 (21.43%) patients taking betaserc, the frequency of attacks decreased by 25–49% from the initial values by the 14th day of taking the drug: in 2 (4.76%) patients with an initial 6 attacks of dizziness per day, their frequency decreased to 4, in 3 (7.14%) patients with 7 attacks before treatment with betaserc, their number decreased to 4, in 3 (7.14%) patients with an initial 4 paroxysms of dizziness per day - to 3 and in one patient with 3 attacks before treatment with betaserc, the frequency of paroxysms of dizziness decreased to 2. Thus, the effectiveness of the reference drug betaserc in these 9 (21.43%) patients can be assessed as moderate.
In 5 patients in the control group (11.90%) with an initial 5 attacks of dizziness per day, their frequency by the end of betaserc therapy decreased only to 4 (less than 25%), which made it possible to assess the effectiveness of therapy in them as low.
Thus, the study drug Vestinorm and the reference drug betaserc had an equally effective effect on reducing the frequency of dizziness attacks in patients with chronic vertebrobasilar vascular insufficiency.
The severity (intensity) of dizziness attacks was assessed by patients using the Dizziness Handicap Inventory (DHI) scale (1996). Data on the distribution of patients during the 2-week course of treatment (before treatment, on the 3rd, 7th day of treatment and after completion of therapy with Vestinorm and Betaserc) according to the intensity of dizziness according to the scoring of this scale are given in Table. 5 and in Fig. 2.
Before starting therapy with Vestinorm and betaserc, the majority of patients assessed the intensity of dizziness as mild or moderate (III and IV points on the DHI scale): mild intensity of attacks was observed in 23.81% of patients in the main group and 21.43% in the control group, moderate - in 50 .00 and 54.76% of patients in both groups, respectively. Attacks of dizziness of weaker intensity (minimum - II DHI points) before the start of therapy with both drugs were not observed in any patient, while severe (V points on the DHI scale) attacks were noted by 11.90% of patients in both groups, and significantly pronounced (VI points on the DHI scale) - 14.28 and 11.90% of patients in both groups, respectively (Table 5, Fig. 2).
On the 3rd and especially on the 7th day of taking Vestinorm and Betaserc, a tendency towards a decrease in the intensity of dizziness attacks was revealed. Already on the 3rd day of taking the drugs, the number of patients with severe and significantly severe attacks of dizziness (V-VI points on the DHI scale) decreased significantly - 2 (4.76%) patients in each group. On the 7th day of taking Vestinorm, the number of patients with attacks of mild intensity (III point) increased to 30.95%; in both groups, 19.05% of patients for the first time noted a significant decrease in the intensity of dizziness to a minimum (II point); the number of patients with severe and significantly severe attacks of dizziness (V–VI points on the DHI scale) also continued to decrease (Table 5).
By the 14th day of the study at the end of the course of treatment, 1 patient (2.38%) in the Westinorm group and 2 (4.76%) in the Betaserc group had completely stopped their attacks (I point on the DHI scale), not a single patient had severe or significantly severe attacks of dizziness were observed (V–VI points on the DHI scale). The majority of patients (47.62 and 52.38% in the main and control groups, respectively) had minimal signs of dizziness, corresponding to II points on the DHI scale. Mild intensity of dizziness (III point on the DHI scale) was observed in 30.95 and 26.19% of patients taking Vestinorm and betaserc, respectively, and moderate intensity (IV point on the DHI scale) - in 19.05 and 16.67% of patients, respectively (Table 5, Fig. 2).
Thus, the study drug Vestinorm and the reference drug betaserc had a significant and quantitatively comparable positive effect on the severity of dizziness, manifested in a significant reduction in the intensity of dizziness attacks on the DHI scale in patients with chronic vertebrobasilar vascular insufficiency.
An analysis of the dynamics of the intensity of dizziness attacks under the influence of 2-week therapy with Vestinorm and Betaserc revealed a decrease by more than one point on the DHI scale in 38 (90.47%) patients in each of the study groups, which corresponded to the high and moderate effectiveness of the compared drugs in terms of this indicator. In 4 patients (9.52%) in each group, by the end of the 2-week course of treatment, the initial moderate degree of dizziness intensity remained (III point on the DHI scale), which was regarded as low effectiveness.
An examination and survey of all patients in the main and control groups during this clinical study did not reveal any complaints, unexpected adverse reactions, complications or intolerance to the compared drugs Vestinorm and betaserc when prescribed daily, 1 tablet 3 times a day for 14 days.
The patients did not complain of nausea, vomiting, headache and did not experience any unpleasant sensations (such as a feeling of heaviness in the epigastrium or abdominal pain) that could be associated with the effect of the studied drugs. Allergic reactions in the form of skin rash, itching, and urticaria were also not observed when taking the study drugs. The absence of side and toxic effects under the influence of 2-week therapy with Vestinorm and Betaserc is also confirmed by data from objective clinical and laboratory studies (Tables 6, 7).
The compared drugs did not have a negative effect on the main indicators of cardiac activity and hemodynamics: at the end of the study, patients in both groups showed no significant changes in heart rate and blood pressure (Table 6).
Long-term 2-week administration of the compared drugs also did not have any negative impact on the indicators of the morphological composition of peripheral blood, on the levels of its main biochemical constants characterizing the functional state of the liver and kidneys, and did not affect the indicators of clinical urine analysis (Table 7).
In general, based on the subjective complaints of patients and the results of objective clinical and laboratory studies, the tolerability of Vestinorm and Betaserc can be assessed as good in all patients of the main and control groups.
Analysis of the results of assessing the effect of a 2-week course of therapy with Vestinorm and Betaserc on the dynamics of the frequency and intensity of dizziness attacks allowed us to make a final assessment of the effectiveness of treatment in the compared groups, which is presented in Table. 8.
Thus, at the end of the study, 27 (64.29%) patients in the main group and 28 (66.67%) patients in the control group experienced relief or reduction in the frequency of dizziness attacks by more than 50% and a weakening of the intensity of attacks by 1 or more points on the scale DHI, which corresponded to high efficiency.
In 11 (26.19%) patients in the main group and 9 (21.43%) patients in the control group, the frequency of dizziness attacks decreased by 25–49% and the intensity of dizziness attacks decreased by 1 or more points on the DHI scale, which corresponded to moderate effectiveness.
In 4 (9.52%) patients in the main and 5 (11.90%) in the control group, there was a decrease in the frequency of attacks by less than 25% with almost unchanged severity of dizziness on the DHI scale, which made it possible to evaluate the effectiveness of the compared drugs as low ( Table 8).
Thus, in terms of the spectrum and quantitative expression of clinical effectiveness, as well as in terms of the studied tolerability indicators, the study drug Vestinorm was completely therapeutically equivalent to the reference drug betaserc.
Vestinorm, instructions for use (method and dosage)
Tablets are prescribed orally for adults. It is best to take the medicine after meals without chewing the tablet.
The dosage and duration of therapy is determined by the attending physician, depending on the effectiveness of treatment and the individual characteristics of the patient.
It is best to prescribe the drug in the early stages of the disease to avoid its progression or decrease in the patient’s hearing acuity.
Instructions for use of Vestinorm
The daily dosage ranges from 24 to 48 mg.
Depending on the dose, the frequency of administration varies. For example, Vestinorm 24 mg is prescribed 1 tablet 2 times a day. Tablets with a dosage of 16 mg are taken 0.5-1 tablets 3 times a day. A medicine containing 8 mg of active substance is taken 1-2 tablets 3 times a day.
On average, the duration of treatment is several months. Sometimes improvements in the condition occur only after 14-21 days of daily pill taking.
No dosage adjustment is required for elderly people, people with liver and kidney diseases.
Special instructions for the use of the drug Vestinorm
In patients with peptic ulcers of the stomach or duodenum (including a history) the drug is prescribed with caution. During the period of use of Vestinorm, patients with pheochromocytoma and asthma should be under medical supervision. There is no experience with the use of the drug during pregnancy and lactation, as well as in children. Vestinorm does not have a sedative effect and does not affect the patient’s ability to engage in potentially hazardous activities that require increased attention and speed of psychomotor reactions (driving vehicles, working on machines and machines).
Analogs
Level 4 ATX code matches:
Betagis
Stugeron
Betaserk
Betaver
Westicap
Betagistine
Tagista
Vestibo
Cinnarizine
Aviomarin, Cinarizin, Vesticap, Cinnaridone, Stugeron, Tablets for motion sickness and nausea, Betaserc, Avetide, Akuver.
Reviews about Vestinorm
Reviews about the drug are good. It is often taken by patients with VSD to relieve unpleasant symptoms, dizziness and speech problems after traumatic brain injuries .
Reviews about Vestinorm:
“I have been familiar with such drugs for dizziness for a long time. I was prescribed Vestinorm at a dosage of 24 mg, once a day, for ten days, and then we’ll see about the condition, as the doctor told me. Around the fourth day, my condition improved noticeably. I don’t know, maybe I should have continued taking the drug, but I stopped taking it because it went away”;
“I have VSD + PA. Dizziness occurs very often, I read about Westinorm on the forum. I tried it and the dizziness became less frequent”;
"I am 50 years old. A diagnosis of vertebrobasilar insufficiency was made. I took Vestinorm for a month. I haven't drunk for 2 days. The dizziness does not go away completely, but has decreased. There are more head positions in which I don’t feel dizzy.”
VESTINORM 24MG TAB No. 30
Instructions
Trade name of the drug: Vestinorm®
Active ingredients: Betahistine
Pharmacotherapeutic group: Medicine against motion sickness syndrome, Medicine against motion sickness syndrome
Release form:
10 tablets in a blister. 8 mg tablets. 3 blisters per pack. Tablets of 16 mg and 24 mg. 3 or 6 blisters per pack.
Dosage form:
Tablets 8 mg N30 (3×10), 16 mg, 24 mg N30 (3×10), N60 (6×10) (blisters)
Compound:
1 tablet contains: Active substance: betahistine dihydrochloride 8 mg or 16 mg, or 24 mg based on 100% dry matter; Excipients: microcrystalline cellulose, sodium starch glycolate (type A), colloidal anhydrous silicon dioxide, povidone, magnesium stearate.
Pharmacokinetics:
Absorption When administered orally, betahistine is rapidly and almost completely absorbed from the digestive tract. After absorption, the drug is quickly and almost completely metabolized to form the metabolite 2-pyridylacetic acid. The plasma concentration of betahistine is very low. Therefore, all pharmacokinetic analyzes are carried out by measuring the concentration of the metabolite 2-pyridylacetic acid in blood plasma and urine. When taking the drug with food, its maximum concentration (Cmax) is lower than when taken on an empty stomach. However, the complete absorption of betahistine is identical in both cases, indicating that food intake only slows down the absorption of the drug. Distribution The percentage of betahistine that is bound to plasma proteins is less than 5%. Biotransformation After absorption, betahistine is quickly and almost completely metabolized into 2-pyridylacetic acid (which does not exhibit pharmacological activity). After taking betahistine orally, the concentration of 2-pyridylacetic acid in the blood plasma (and in the urine) reaches its maximum 1 hour after taking the drug and decreases with a half-life of about 3.5 hours. Excretion 2-pyridylacetic acid is rapidly excreted in the urine. When taking the drug at a dosage of 8-48 mg, about 85% of the initial dose is found in the urine. Excretion of betahistine by the kidneys or feces is negligible. Linearity The rate of recovery remains constant with oral dosing of 8-48 mg of the drug, indicating linearity in the pharmacokinetics of betahistine and suggesting that the metabolic pathway involved remains mild. The mechanism of action of betahistine has only been partially studied. There are several credible hypotheses that support data from animal and human studies. The effect of betahistine on the histaminergic system: it has been established that betahistine partially exhibits antagonistic activity towards H1 receptors, as well as antagonistic activity towards histamine H3 receptors in nervous tissue and exhibits insignificant activity towards histamine H2 receptors. Betahistine increases the metabolism and release of histamine by blocking presynaptic H3 receptors and inducing a decrease in the number of corresponding H3 receptors. Betahistine may increase blood flow in the cochlear region, as well as throughout the brain: pharmacological studies in animals have demonstrated improved blood flow in the stria vascularis of the inner ear, possibly due to relaxation of the precapillary sphincters in the microcirculation of the inner ear. Betahistine has also been shown to increase cerebral blood flow in humans. Betahistine Promotes Vestibular Compensation: Betahistine accelerates recovery of vestibular function after unilateral neurectomy in animals by accelerating and promoting central vestibular compensation. This effect is characterized by increased regulation of histamine metabolism and release and is realized as a result of H3 receptor antagonism. In humans, treatment with betahistine also reduced the time to recovery of vestibular function after neurectomy. Betahistine alters the activity of neurons in the vestibular nuclei: Betahistine has also been found to have a dose-dependent inhibitory effect on the generation of peak potentials in neurons of the lateral and medial vestibular nuclei. The pharmacodynamic properties of betahistine, as shown in animals, may provide a positive therapeutic effect of the drug in the vestibular system. The effectiveness of betahistine was shown in studies involving patients with vestibular vertigo and Meniere's disease, during which a decrease in the severity and frequency of dizziness attacks was observed.
Indications for use:
Meniere's disease and syndrome, characterized by such main symptoms as dizziness, sometimes accompanied by nausea and vomiting, hearing loss (hearing loss), and tinnitus. Symptomatic treatment of vestibular vertigo.
Mode of application:
Prescribed orally for adults. The daily dose is 24-48 mg, evenly distributed throughout the day. Tablets of 8 mg Tablets of 16 mg Tablets of 24 mg 1-2 tablets 3 times a day ½-1 tablet 3 times a day 1 tablet 2 times a day Tablets are taken after meals, without chewing. The dose and duration of therapy are determined by the doctor individually depending on the effectiveness of the therapy. A reduction in symptoms is sometimes observed only after 2-3 weeks of treatment. The best results are observed when taking the drug for several months. If treatment is prescribed at the onset of the disease, progression and/or hearing loss in later stages can be prevented. Elderly patients No dose adjustment is required for patients in this group. Renal failure No dose adjustment required. Liver failure No dose adjustment required.
Side effects:
From the digestive tract: often – nausea, dyspepsia; frequency unknown - complaints of minor stomach upsets (vomiting, abdominal pain, bloating and flatulence). These side effects usually go away when the drug is taken with food or when the dose is reduced. From the nervous system: often – headache. From the immune system: frequency unknown - hypersensitivity reactions, such as anaphylaxis. From the skin and subcutaneous tissue: frequency unknown - hypersensitivity reactions of the skin and subcutaneous fat, in particular angioedema, rash, itching and urticaria, have been observed.
Contraindications:
Hypersensitivity to the active substance and other components of the drug. Pheochromocytoma. Children's age, pregnancy and lactation (due to the lack of sufficient experience in using the drug in these categories of patients). Drug interactions: Based on in vitro data, inhibition of cytochrome P450 enzyme activity in vivo is not expected. Data obtained in vitro indicate inhibition of betahistine metabolism by drugs that inhibit monoamine oxidase (MAO) activity, including MAO subtype B (for example, selegiline). Caution is recommended when using betahistine and MAO inhibitors (including selective MAO subtype B) simultaneously. Because betahistine is a histamine analog, interaction between betahistine and antihistamines could theoretically affect the effectiveness of one of these drugs.
Special instructions:
Patients with a history of bronchial asthma, gastric and duodenal ulcers require careful medical supervision during treatment with Vestinorm. Use during pregnancy or breastfeeding. There are no data regarding the use of betahistine in pregnant women. The drug should only be taken if absolutely necessary and under the direct supervision of a physician. The penetration of betahistine into breast milk has not been studied. The benefit of using the drug is determined by the ratio of the benefits of breastfeeding to the potential risk for the child. Children. There is no experience in using the drug to treat children, so it should not be prescribed to this age category. The ability to influence the reaction rate when driving a vehicle or working with other mechanisms. Betahistine, according to clinical studies, does not have a significant effect or effects that potentially affect the ability to drive a car or operate other machines. The drug should not be used after the expiration date and should be stored out of the reach of children.
Overdose:
In case of overdose, nausea, abdominal pain, and drowsiness may occur. There have been reports of seizures and cardiopulmonary complications when intentionally taking high doses of betahistine, especially in combination with overdose of other drugs. Treatment: symptomatic therapy.
Storage conditions:
Store in a place protected from light at a temperature not exceeding 25ºС.
Shelf life: 3 years.
Dispensing conditions: By prescription.
Manufacturer: Farmak, PJSC, Ukraine
Westinorm price
The cost of the drug is approximately 150 hryvnia for 60 tablets with a dosage of 24 mg.
- Online pharmacies in RussiaRussia
- Online pharmacies in UkraineUkraine
LuxPharma* special offer
- Westinorm tab.
24 mg No. 30 1800 rub. order - Westinorm tab. 16mg N30
1600 rub. order
show more
Pharmacy24
- Vestinorm 24 mg N30 tablets PAT "Farmak", Ukraine
110 UAH. order - Vestinorm 24 mg N60 tablets PAT "Farmak", Ukraine
204 UAH order
- Vestinorm 16 mg N30 tablets PAT "Farmak", Ukraine
91 UAH order
- Vestinorm 16 mg N60 PAT "Farmak", Ukraine
165 UAH order
- Vestinorm 8 mg No. 30 tablets PAT "Farmak", Ukraine
68 UAH order
Materials and research methods
This clinical trial was conducted as an open, comparative, randomized and parallel study. The study included 84 patients of both sexes from 18 to 65 years old with at least 10 attacks of dizziness per week resulting from chronic vertebrobasilar insufficiency, who were undergoing inpatient and outpatient treatment at the Institute of Neurology, Psychiatry and Narcology of the Academy of Medical Sciences of Ukraine. The patients were divided into the main and control groups of 42 patients each. Patients of the main group received the study drug Vestinorm, the control group received the reference drug betaserc, 1 tablet (8 mg) 3 times a day for 14 days.
The diagnosis of dizziness due to chronic vertebrobasilar vascular insufficiency was established on the basis of complaints of attacks of systemic dizziness, which was described by the patient as a feeling of movement of one’s own body (rotation, spinning, falling or swaying) and/or surrounding objects around one of the axes of three-dimensional space, often in combination with the sensation sinking, unsteadiness of the soil underfoot. The diagnosis was confirmed by the presence of typical vertebrogenic complaints: dull, aching pain in the cervical spine, limitation of head movements, increased pain and the appearance of dizziness with sharp flexion or extension of the neck, as well as with prolonged constant load on the cervical spine, pain radiating to the occipital region, upper limbs. Patients were diagnosed with limited range of motion in the cervical spine (especially turning and tilting the head), pain in the spinous processes and paravertebral points at the level of the vertebral motor segments C3–C7, naderbov points, points of the vertebral artery, and stellate ganglion. To identify vestibular disorders, a de Klein test was performed (the test was considered positive when spontaneous nystagmus appeared when throwing the head back or turning to the sides with subsequent fixation).
The duration of the disease was: up to 6 months - 9.52% of patients in the main group and 11.90% of patients in the control group, from 6 months to 1 year - 30.95% of patients in the main group and 26.19% of patients in the control group, more than 1 year (1 –5 years) - 59.52 and 61.90% of patients in the main and control groups, respectively.
The average frequency of dizziness attacks per week in patients of the main group was 28.5 ± 9.3, in patients of the control group - 27.6 ± 9.9.
From the table 1 shows that the patients of the main and control groups included in the study were comparable in age, gender and body weight.
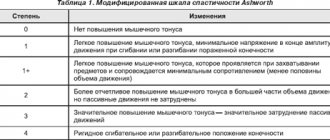
Methods for assessing the clinical and neurological status included a general clinical examination with recording of blood pressure (BP), heart rate (HR) and other physical examinations, a survey and clinical examination to collect anamnesis, register the patient’s subjective complaints and identify possible adverse reactions, and assess the neurological the status of patients, taking into account the presence or absence of: nystagmus, hearing impairment, balance and coordination of movements during the Romberg test, somatosensory, autonomic and oculomotor disorders. The assessment of indicators characterizing an attack of dizziness, in particular the frequency of attacks per day and their intensity, was carried out using the Dizziness Handicap Inventory scale (1996):
I - attacks of dizziness do not bother you;
II - minimal symptoms of dizziness;
III - mild symptoms of dizziness when turning the head or standing up, which do not interfere with normal life activities and are not accompanied by autonomic disorders;
IV - moderate symptoms of dizziness: attacks of dizziness lasting up to 10 seconds, minimal restrictions on motor activity, possible autonomic disorders (nausea, vomiting, imbalance, headache);
V - severe symptoms of dizziness: attacks of dizziness lasting up to 30 seconds, moderate restrictions on motor activity, autonomic disorders in most cases of dizziness (nausea, vomiting, imbalance, headache, blurred vision, weakness, falling, numbness in the limbs), restlessness, anxiety regarding possible loss of balance and falling;
VI - significantly pronounced symptoms of dizziness: attacks lasting more than 30 seconds, always accompanied by autonomic disorders (nausea, vomiting, imbalance, headache, blurred vision, weakness, falling, numbness in the limbs), severe limitation of motor activity, fear of possible loss balance and fall.
Laboratory methods included general clinical blood and urine tests and biochemical blood tests (ALT, AST, creatinine, cholesterol, glucose).
Patients participating in the study received concomitant therapy according to indications, including: antiplatelet agents (aspirin), analgesics, antihypertensives, cardiovascular drugs, and physiotherapeutic procedures. A number of patients took medications used to treat concomitant diseases (vitamins, vasoactive agents, chondroprotectors, calcium supplements) in a prescribed dose. During the study, patients in both groups were not prescribed other drugs used to relieve attacks of dizziness: betahistine, cinnarizine, flunarizine, chlorpromazine, diazepam, and antihistamines.
Statistical processing was carried out using variation statistics methods. The average values of the indicators (M) and their standard error (m) were calculated. The reliability of differences between the average values of the studied indicators was determined using the Student's test, assessing the probability at a significance level of at least 95% (p ≤ 0.05).