Dear pharmaceutical workers, hello!
Recently we looked at the most popular groups of antibiotics.
Today I would like to dwell on another group of extremely popular antibacterial agents. I'm talking about fluoroquinolones.
They are not antibiotics because they have no natural analogues. But in terms of efficiency they are in no way inferior.
You don't have to read any further if you quickly answer the questions:
- How many generations of fluoroquinolones are currently on the market?
- Name at least one drug from each generation of this group.
- How do generations differ from each other?
- Which fluoroquinolones are used primarily for genitourinary tract infections?
- Name a rare side effect that is caused by drugs in this group.
- At what age can fluoroquinolones be used and why?
So how? Did you manage?
If not, let's continue the conversation.
From the history of fluoroquinolones
The “parents” of fluoroquinolones are quinolones - nalidixic acid (Negram, Nevigramon), pipemidic acid (Palin), etc.
I'm sure you can tell when they are used.
Did you name it?
Right. Mainly for urinary tract infections. Quinolones are essentially uroseptics, i.e. drugs that free the bladder, kidneys, and ureters from bacterial invaders.
Recently, these drugs have been prescribed less and less often, since much more effective drugs have appeared on the market.
Quinolones were synthesized by accident during the study of an antimalarial drug called Chloroquine.
A few years after their discovery, one of the scientists came up with the idea of adding a fluorine atom to the quinolone formula and seeing what would happen. What has emerged is a completely new group of antibacterial agents, which is comparable in effectiveness to cephalosporins.
Group of fluoroquinolones. Features of generations
In some publications, quinolones are considered together with fluoroquinolones and are classified as their first generation.
It turns out to be some kind of rubbish: quinolones are the 1st generation of fluoroquinolones.
But the group turned out to be completely different, with different characteristics and indications!
So I will speak as common sense tells me.
Today there are 3 generations of fluoroquinolones:
Generations of fluoroquinolones differ from each other in their spectrum of antibacterial activity.
Each new generation is superior in some way to the previous one.
The 1st generation is called “Gram-negative” because drugs belonging to this generation act on a wide range of Gram-negative bacteria. And of the gram-positive ones, only a small handful: several varieties of staphylococcus, listeria, corynebacterium, tuberculosis bacillus.
Let me remind you of gram-negative bacteria: Pseudomonas aeruginosa, Gonococcus (the causative agent of gonorrhea), meningococcus (the causative agent of purulent meningitis), Escherichia coli, Salmonella, Shigella, Proteus, Klebsiella, Enterobacter, Haemophilus influenzae, etc.
1st generation drugs can be divided into 2 groups:
Systemic: Ciprofloxacin, Lomefloxacin and Ofloxacin. They penetrate various organs and tissues, therefore they are used for infections of various locations: respiratory tract, ear, eye, paranasal sinuses, genitourinary tract, gastrointestinal tract, skin, bones, etc.
Uroseptics: Norfloxacin and Pefloxacin. These drugs create high concentrations in the urine, so they are most often used for infections of the genitourinary system.
But drugs of this generation have little effect on pneumococcus, chlamydia, mycoplasma, and anaerobes.
Norfloxacin is also included in eye and ear drops called Normax.
The 2nd generation is called “respiratory”, since the drugs related to it act not only on the same pathogens as the 1st generation, but also on most pathogens of respiratory tract infections (pneumococcus, Mycoplasma pneumoniae, etc.).
They deal well with the same enemies of the people as the 1st generation, but also with pneumococci, chlamydia, and mycoplasmas.
I will call the 3rd generation “the storm of anaerobes.”
While I was collecting material for the article, I met several representatives of this generation, but did not see them in the assortment of pharmacies. I don’t see any point in talking about “dead souls”. So I name the most popular: Moxifloxacin (trade name Avelox).
The drugs, or rather the drug, of the third generation of fluoroquinolones act on the same pathogens as the previous two, plus they are able to destroy anaerobic bacteria. Do you remember who they are?
These are unpretentious microbes that, unlike their intelligent brothers, do not need oxygen to live a full life.
They cause severe infections. Their toxins are extremely aggressive, capable of affecting vital organs and causing peritonitis, abscesses of internal organs, sepsis, osteomyelitis and other serious diseases.
Anaerobic bacteria are also the culprits of tetanus, gas gangrene, botulism, and foodborne diseases.
Thus, from generation to generation the spectrum of antibacterial activity of fluoroquinolones expands.
general characteristics
Fluoroquinolones are the name of a class of quinolone medications that exhibit antimicrobial properties. Their main purpose is etiotropic therapy of diseases of bacterial etiology. Medicines in this group have high bactericidal activity, which makes it possible to use them to treat a wide range of pathologies.
Fluorinated quinolones are classified as antibacterial agents of the latest generation.
Fluoroquinolones are chemically synthesized derivatives of quinolone.
This class of compounds is classified as a separate category of antibacterial agents, since it differs from antibiotics in several ways:
- Origin of active ingredients
. A distinctive feature of the group is its completely artificial origin and the absence of natural analogues. - Structural structure
. The chemical structure of the derivatives is represented by a quinolone crystal lattice, which includes fluorine atoms and a piperazine ring.
Depending on the number of additional atoms, mono-, di- and trifluoroquinolones are distinguished. The introduction of several atoms into the structure (in complex with piperazine) made it possible to synthesize substances with high bioavailability.
Mechanism of action
The pharmacology of fluorinated quinolones is aimed at reducing the population of pathogenic bacterial cultures. Active substances penetrate the structure of the cell membrane and inhibit enzymes necessary for the development of bacteria. The mechanism of action depends on the structural structure of the membranes of pathogens and is aimed at suppressing DNA synthesis of microorganisms. Blocking topoisomerase II makes it possible to interrupt the formation and division of gram-negative bacteria, and disruption of RNA transcription when inhibiting topoisomerase IV leads to the destruction of gram-positive microbes.
Advantages of the fluoroquinolones group
You have probably noticed that many doctors love drugs from this group, which is why they are prescribed quite often.
What good did they find in them?
Let's list their advantages.
Fluoroquinolones:
- They have a wide spectrum of action.
- Penetrates deeply into various tissues.
- They have a long half-life, so they can be used 1-2 times a day.
- They are well absorbed from the gastrointestinal tract, so they are available in oral forms, which is more convenient and enjoyable for many patients.
- Highly effective.
- Well tolerated.
Indications for the use of fluoroquinolones
Fluoroquinolones have a wide, I would even say the widest, range of indications:
- Diseases of the upper and lower respiratory tract.
- Urinary tract and prostate infections: cystitis, urethritis, pyelonephritis, prostatitis. Norfloxacin and pefloxacin work especially well against them.
- Gonorrhea, chlamydia, mycoplasmosis.
- Intra-abdominal infections (peritonitis, cholecystitis, etc.).
- Intestinal infections (salmonellosis, dysentery, cholera, etc.).
- Infections of the skin, soft tissues, bones and joints.
- Sepsis.
- Meningitis.
- Tuberculosis.
- Infections of the eyes, outer ear (norfloxacin).
The choice of fluoroquinolone drug depends on the type and severity of the disease, its duration, the type of pathogen and the effectiveness of previously used drugs.
Each drug has its own advantages. For example:
Ciprofloxacin is the most active of the fluoroquinolones against gram-negative bacteria. It is superior to its “colleagues” in its effect on Pseudomonas aeruginosa. Used in combination therapy of drug-resistant forms of tuberculosis.
Ofloxacin is the most active of the 1st generation against pneumococci and chlamydia, but weaker than the 2nd and 3rd generation drugs.
Norfloxacin and pefloxacin are especially good for urinary tract and prostate infections.
Pefloxacin, in addition, penetrates the blood-brain barrier better than other fluoroquinolones, therefore it is used for meningitis (for this there is a concentrate form for intravenous administration).
Sparfloxacin is superior to other drugs in this group in terms of duration of action. Apply once a day.
Levofloxacin is an isomer of ofloxacin, 2 times more active and better tolerated.
Moxifloxacin is the most active of the entire group against pneumococci, chlamydia, mycoplasmas, and anaerobes. It can be used empirically (that is, blindly, without culturing bacteria) for severe infections of various locations.
Urological infections have a number of features that are associated with their clinical picture. Urology hospital patients are characterized by:
- long-term obstructive uropathy;
- long-term drainage of the urinary tract both in the pre- and postoperative period (cystostomy, pyelostomy, nephrostomy, internal stenting, etc.);
- frequent infection with nosocomial strains and their associations;
- significant suppression of the body’s immunoreactivity with its further aggravation after surgical interventions (anesthesia, blood loss, decompensation of basic organ functions, etc.);
- predominantly elderly and senile age, the presence of concomitant severe somatic pathology.
All these circumstances cause significant difficulties in the treatment of bacterial infections in urological patients.
Among the numerous antibacterial drugs used in the treatment of bacterial infections in urology, fluoroquinolones occupy one of the leading places and are the drugs of choice.
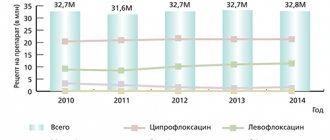
At the beginning of the 21st century, the so-called new fluoroquinolones appeared (Table 1).
The group of early fluoroquinolones has been successfully used for about 20 years and is characterized by very broad indications for use, practically independent of the location of the infection. Basically, drugs in this group are used orally, and in severe forms of the disease - parenterally. Over two decades, more than 30 fluoroquinolones with high antibacterial efficacy have been developed, studied and used in the clinic, but about 10 drugs are used in practical medicine, with the first, early fluoroquinolones being the most widely used. In recent decades, new fluoroquinolones have begun to be used - sparfloxacin, levofloxacin, moxifloxacin (approved for use in Russia).
The spectrum of action of early fluoroquinolones includes gram-negative and gram-positive aerobic bacteria with slightly higher activity against gram-negative microorganisms and a pronounced effect (for some drugs) on pathogens with intracellular localization - chlamydia, mycoplasma, legionella.
The new fluoroquinolones have significantly increased activity against gram-positive aerobic bacteria (while maintaining high activity against gram-negative bacteria), intracellular pathogens and non-spore-forming anaerobes, including strains resistant to the action of earlier fluoroquinolones.
In general, we can summarize some features of new fluoroquinol drugs that justify their use for urogenital infections:
- wide antimicrobial spectrum, covering almost all significant uropathogens;
- predominantly via the renal route of elimination, creating high concentrations in the urine;
- good penetration into organs, tissues and cells of the body; high activity against pathogens with intracellular localization;
- high concentration in the tissues of the kidneys, prostate gland, genital organs in men and women;
- prolonged pharmacokinetics, long half-life (single daily use is sufficient).
Let us consider in more detail the spectrum of antimicrobial activity of 3 drugs that we used in the treatment of urological patients - levofloxacin, sparfloxacin and moxifloxacin (Table 2).
From these tables it follows that the new fluoroquinolones have high activity against all significant uropathogens.
Sparfloxacin was discovered in 1992, registered in Russia and is used for a large number of indications. For urological practice, sparfloxacin is of interest from the point of view of the breadth of its spectrum of action, combining activity against gram-negative microorganisms with increased activity against intracellular pathogens (Table 2). From the point of view of urological pathology, the high activity of sparfloxacin against enterobacteria, the most common causative agents of urinary tract infections, is significant. Thus, the presented data on the antimicrobial effect of sparfloxacin indicate the activity of the drug against gram-positive and gram-negative microorganisms, causative agents of acute, chronic and nosocomial infections of the genitourinary organs.
Sparfloxacin has prolonged pharmacokinetics (T1/2 - 16-20 hours), taken once a day in a low dose - 200 mg orally. Sparfloxacin is a difluoroquinolone (6,8-fluoroquinolone) with an amino group at position 5. These structural features somewhat worsen the toxicological characteristics of the drug, increasing, in particular, its phototoxicity.
The drug is easily absorbed when taken orally, bioavailability is 60%. Sparfloxacin reaches effective concentrations in lung tissue, sputum, pleural exudate, prostate gland, and genital tissues in men and women.
When taking sparfloxacin at a dose of 400 mg, 8.8% or more of this drug is excreted by the kidneys within 50 hours. Extrarenal mechanisms of excretion include biliary excretion of the active drug and its metabolite, sparfloxacin glucuronide; 50–56% of the dose taken is excreted in feces.
We observed 43 patients with complicated forms of urological infections, with a long course of the disease and repeated courses of antibacterial therapy in the anamnesis (Table 4).
Complicating factors in patients with pyelonephritis (31 patients) were urolithiasis, nephroptosis, congenital kidney anomalies, hydronephrotic transformation, diabetes mellitus, etc. Among 12 patients with exacerbation of chronic prostatitis, the disease occurred against the background of benign prostatic hyperplasia (9 patients), with the presence of a cystostomy – at 3.
Upon admission to the hospital, patients were examined by clinical and laboratory methods (including bacteriologically) with the isolation and identification of the pathogen, determination of antibiotic sensitivity (disk diffusion method), the degree of bacteriuria - upon admission, during treatment and after completion of the course of therapy (Table . 5). Sparfloxacin was prescribed according to the following regimen: 400 mg on day 1, 200 mg on subsequent days. The duration of the course of therapy was 7–14 days according to indications.
Studies have shown the high sensitivity of the isolated pathogens to sparfloxacin. In relation to the studied gram-negative cultures, sparfloxacin showed the greatest activity against E. coli, P. mirabilis, P. vulgaris and K. pneumoniae. Resistant strains were found among P. aeruginosa (as part of associations with enterococci) and Enterobacter spp. As a rule, these were multidrug-resistant cultures (isolated from patients with pyelonephritis), and the disease became protracted with the need to replace, in some cases, antibacterial drugs. S. epidermidis and S. aureus were isolated during exacerbation of chronic prostatitis; they were sensitive to sparfloxacin to a greater extent than to ciprofloxacin.
The degree of bacteriuria upon admission of patients ranged from 5 x 104 to 5 x 107 CFU/ml with a decrease in the titer of microorganisms at the end of treatment to 3 x 102 CFU/ml and even with complete elimination of the pathogen in 14 patients with pyelonephritis (including 8 patients with acute pyelonephritis). Partial elimination (up to 5 x 104 CFU/ml) was achieved in 6 cases when Enterobacter spp. and in 2 cases – P. aeruginosa, and therefore the antibacterial therapy regimen was changed.
A good clinical effect was achieved in 35 patients, which was expressed in a decrease in fever, a decrease or disappearance of clinical symptoms of the disease, positive dynamics of laboratory parameters (decrease in leukocytosis, decrease in the shift of the leukocyte formula to the left; a sharp decrease or disappearance of bacteriuria; normalization of urine analysis, etc.).
Unsatisfactory treatment results in 8 patients were due to the need for surgical treatment: in 5 patients with urolithiasis (occlusion of the ureteropelvic segment of the kidney by a stone); in 3 with prostatitis - due to acute urinary retention. In the postoperative period, antibacterial therapy ensured the recovery of these patients.
In general, the clinical effectiveness of sparfloxacin in the treatment of complicated forms of pyelonephritis and prostatitis was achieved in 88.7% of cases, bacteriological - in 78.1%.
Thus, sparfloxacin, a second generation fluoroquinolone, is characterized by a wide spectrum of action, and in terms of activity against gram-positive microorganisms, especially staphylococci and some intracellular pathogens, it is superior to ciprofloxacin. The drug has a prolonged effect and penetrates well into the genitourinary system.
The use of sparfloxacin for chronic pyelonephritis and chronic prostatitis in 43 patients demonstrated high effectiveness in terms of clinical and bacteriological indicators (88.7 and 78.1%, respectively) when used once a day for 7–14 days.
Sparfloxacin was well tolerated by patients. Although cases of phototoxicity and prolongation of the QT interval on the ECG have been described in the literature with the use of this drug, in our observations no such adverse reactions were noted.
Levofloxacin is a levorotatory isomer of ofloxacin. The high effectiveness of ofloxacin, a wide range of indications for its use, the resistance of the molecule to biotransformation in the body, the absence of interaction with most drugs of other pharmacotherapeutic groups and the possibility of developing two dosage forms became the basis for isolating its active isomer into an independent drug. Levofloxacin is 2 times more active than ofloxacin, since in the racemic mixture the activity of the latter is reduced due to the presence of 50% of the weakly active dextrorotatory isomer. In case of insufficiency of renal function, dose adjustment of levofloxacin is required, which is mainly eliminated by renal excretion.
We used levofloxacin in the treatment of 49 patients. All patients had complicated urinary tract infections. They were prescribed monotherapy with levofloxacin under control of microflora sensitivity in vitro. Levofloxacin was used 1 tablet once a day (250 mg in 23 patients, 500 mg in 26 patients). The course of treatment was 10–14 days.
The nosological forms of urological infections in the patients we observed were pyelonephritis, cystitis and chronic prostatitis (all in the acute stage). Complicating factors were urolithiasis, anomalies in the development and location of the kidneys, strictures of the ureters or urethra, benign prostate adenoma, etc.
The clinical effectiveness of treatment with levofloxacin was 100%. This is confirmed by clinical data, laboratory test results, and ultrasound data. Several patients during treatment were successfully operated on with continuation of therapy in the postoperative period, which in all cases proceeded without complications.
From patients treated with levofloxacin, 65 cultures of microorganisms were isolated, the titers of which varied from 105 to 108 CFU/ml. The most frequently detected cultures were E. coli and Enterobacter spp. In addition, several associations were found, such as E. faecalis + Morganella spp., Proteus spp. + Streptococcus spp., Enterobacter spp. + S. epidermidis, etc.
Overall, the bacteriological effectiveness of treatment of complicated urological infections with levofloxacin was 98.5%. The best results were achieved when using the drug in 500 mg tablets. If, when using levofloxacin at a dosage of 250 mg, one culture, Enterobacter spp, was not eliminated, and in 4 observations, along with elimination, superinfection was observed, then when treated with this drug at a dosage of 500 mg, all microorganisms were eliminated and only 2 cases of superinfection were observed.
Levofloxacin was well tolerated by patients; no serious adverse reactions, including phototoxicity, were detected with its use.
Based on the study, it was concluded that levofloxacin is a highly active treatment for patients with urological infections, and it is advisable to treat complicated infections of the genitourinary organs using this drug in 500 mg tablets.
Moxifloxacin is a monofluoroquinolone, the structural feature of which is the presence of an OCH3 group at position 8 and a cyclopropyl radical at position 1 of the quinolone ring. Among the new fluoroquinolones, moxifloxacin is one of the most active drugs against gram-positive bacteria, atypical microorganisms and anaerobes, covering almost all significant uropathogens (Table 2). In terms of the spectrum of antimicrobial action and activity, moxifloxacin is superior to ciprofloxacin.
Moxifloxacin has a bactericidal effect and is characterized by a long-term post-antibiotic effect. The drug is well absorbed from the gastrointestinal tract; food intake slows absorption, but does not affect absorption rates. The volume of distribution of moxifloxacin exceeds 200 liters, which indicates its good penetration into organs, tissues and cells of the body.
The half-life is 11–14 hours, which is the basis for using the drug once a day. The amount of moxifloxacin excreted in the urine is about 20%; a significant part of the unchanged drug is eliminated from the body in feces (about 25%). Renal excretion is primarily due to glomerular filtration.
Our studies involved 46 patients with various uncomplicated (22 people) and complicated urinary tract infections (24 people). The characteristics of the patients are presented in more detail in Table. 6.
Moxifloxacin was presented for research in the form of 400 mg tablets for once daily use. The duration of therapy averaged 7–14 days (7–10 – uncomplicated infections, 10–14 – complicated infections). In the presence of prostatitis, treatment continued for 2–4 weeks.
Already on days 3–5 from the start of treatment with moxifloxacin, positive dynamics were observed in terms of the general well-being of patients and objective data. The symptoms of intoxication stopped, leukocytosis and band neutrophil shift decreased, disappearing by the end of treatment.
Recovery under the influence of treatment occurred in 44 of 46 patients. In two patients the therapeutic effect was not achieved. In one observation, moxifloxacin therapy was ineffective in a patient with complicated pyelonephritis that arose against the background of urolithiasis. As a result of extracorporeal lithotripsy, the calculus located in the pelvis of the left kidney was disintegrated and a large fragment of the latter blocked the ureteropelvic segment of the kidney. A double culture was isolated from the patient: S. marcescens and E. coli in high titer (5 x 105 CFU/ml). It was not possible to eliminate these cultures under occlusion conditions. Surgery was required. After removal of the stone, pyelonephritis was treated with routine antibiotic therapy.
In another observation, a patient with exacerbation of long-term prostatitis who had undergone numerous operations on the prostate gland was treated. When inoculating his sperm, a moxifloxacin-sensitive culture of P. aeruginosa was isolated in a small titer, but significant for prostatitis (5 x 104 CFU/ml). However, long-term therapy with this drug was unsuccessful.
Thus, the clinical effectiveness of treatment with moxifloxacin was 95.7% in our observations.
We carried out etiotropic monotherapy with moxifloxacin under the control of microbial sensitivity to this drug in vitro. 56 cultures of microorganisms were isolated from patients (Table 7).
The treatment allowed us to eliminate 48 out of 56 cultures, i.e., the bacteriological effectiveness of treatment was 85.7%.
It should be noted that during therapy the patients did not develop side effects or unwanted reactions.
Based on the studies, the following conclusion can be drawn: new fluoroquinolones are highly effective in the treatment of uncomplicated and complicated urological infections, such as cystitis, pyelonephritis and prostatitis. Complicating factors for these infections may be urolithiasis, diabetes mellitus, anomalies in the development and location of the kidneys, nephroptosis, hydronephrotic transformation of the kidneys, benign prostatic hyperplasia, the presence of various drainages, neurogenic bladder, cystocele, stress urinary incontinence, various types of strictures of the ureters, urethra, chronic renal failure, etc.
With the therapeutic use of new fluoroquinolones, good results were obtained: clinical effectiveness ranged from 88.7–100%, bacteriological – 78.1–98.5%.
Generalized data on the indications for use and antimicrobial activity of new fluoroquinolones when used in urological practice, confirmed by the results of our studies, are presented in Table. 8.
Contraindications to the use of fluoroquinolones
Common to all:
- Pregnancy.
- Lactation.
- Allergic reactions to fluoroquinolones.
- Childhood and adolescence.
Fluoroquinolones are contraindicated under 18 years of age, since in animal experiments researchers noted a delay in the development of cartilage tissue. Therefore, as a rule, they are not prescribed until the formation of the skeleton is complete. Although, in some cases, doctors prescribe fluoroquinolones to children on their own responsibility. For example, with cystic fibrosis or intolerance to other antibacterial agents.
Interaction
The compatibility of fluoroquinolones with other pharmacological groups is quite high. There are several risks of joint use:
- high neurotoxicity when combined with NSAIDs and methylxanthines;
- the effect of nitrofurans is neutralized;
- preparations with metal ions reduce the absorption of quinolone derivatives;
- The effectiveness of anticoagulants decreases.
A distinctive feature of fluoroquinolones is arthrotoxicity - a negative effect on connective joint tissue. When combining them with glucocorticosteroids, there is a risk of tendon rupture and thinning of cartilage tissue.
With irregular intake of antibacterial agents, resistance to antimicrobial components occurs in the body.
Aminoglycosides, sulfonamides, cephalosporins and tetracyclines introduced into the therapeutic plan do not affect the activity of fluoroquinolones. The simultaneous use of macrolides, penicillins and fluoroquinolone antimicrobial agents is not advisable, since any drug containing fluorinated derivatives has a more significant therapeutic effect.
The most common side effects of fluoroquinolones
- From the gastrointestinal tract: abdominal pain, nausea, vomiting, diarrhea. Therefore, advise taking them after meals.
- Central nervous system disorders: headache, dizziness, convulsions (in people with epilepsy).
- Photodermatoses, i.e. increased skin sensitivity to ultraviolet rays. When exposed to the sun, fluoroquinolones are destroyed, free radicals are formed and cause skin damage.
This means that when selling a drug from this group, you need to offer a sunscreen. Especially in summer and in sunny regions.
Lomefloxacin (Lomflox) and sparfloxacin (Sparflo) differ more than others in their ability to cause photodermatoses.
- Increased liver transaminases. This means that the drugs are hepatotoxic. Therefore, it would be a good idea to take a drug from the fluoroquinolone group in conjunction with a hepatoprotector. Rarely, drug-induced hepatitis does occur.
- Increased QT interval on ECG. For healthy people this is not scary. And if the drug is taken by a person who has serious heart problems, there may be arrhythmia. But this happens when taking large doses of the drug.
- A rare side effect is tendinitis, i.e. inflammation of the tendon and its rupture. Most often, the Achilles tendon is affected. This happens mainly in older people.
Tendonitis occurs because fluoroquinolones inhibit the activity of an enzyme necessary for the synthesis of collagen protein. And it forms the basis of tendons, and connective tissue in general.
Important:
If fluoroquinolones are taken simultaneously with an antacid and a vitamin-mineral complex, insoluble compounds are formed and the drug will not have the desired effect. Therefore, the break between doses should be at least 4 hours.
Now let’s remember all of the above and draw up a list of recommendations for the buyer.