- Analyzes
- Prices
- About Us
- Contacts
Patau syndrome is a chromosomal disorder caused by the presence of an extra chromosome 13 pair.
This pathology was discovered in 1657 by the scientist Erasmus Bartholin, but the chromosomal cause was proven only in 1960 by Dr. Klaus Patau.
Patau syndrome is a rare pathology (1:7000-1:10000 cases), occurring with equal frequency in both sexes. The hereditary etiology of the disease has not been proven; the incidence increases with the age of the parents.
You can find out with 99% accuracy about the risk of Patau syndrome and other chromosomal abnormalities, as well as the sex of the fetus, from 9 weeks of pregnancy, just by donating blood from a vein. Learn more about the NIPT test.
Patau syndrome statistics
Proper development of the human body requires the presence of 2 (and only 2) copies of human autosomal chromosomes. Having a third copy of the chromosome is usually lethal to the developing embryo. Trisomy 13 refers to a narrow group of trisomies that includes only three diseases.
Patau syndrome occurs with a frequency of 1 in 8,000 to 12,000 births. Although the direct cause of the disease has not yet been established, the risk of its occurrence increases with maternal age.
Patau syndrome is well expressed even in the fetus, but the full symptoms of the pathology become visible immediately after the birth of the child. In most cases, a fetus with trisomy 13 dies in the uterus. The percentage of deaths in the neonatal period is also very high.
Children who survive more than 1 month have progressive developmental impairment. The average life expectancy of babies affected by this genetic defect is just over 3 years. Only a few children reach adolescence. Case reports of Patau syndrome in adults are extremely rare.
Girls with Patau syndrome are slightly more common. This is probably due to the more frequent freezing of male fetuses in the uterus.
History[edit]
Trisomy 13 was first discovered by Thomas Bartholin in 1657,[11] but the chromosomal nature of the disease was established by Dr. Klaus Patau in 1960.[12] The disease is named after him.
In England and Wales, there were 172 diagnoses of Patau syndrome (trisomy 13) in 2008–09, with 91% of diagnoses made prenatally. There were 111 elective abortions, 14 stillbirths/miscarriages/fetal deaths, 30 unknown outcomes, and 17 live births. Approximately 4% of Patau syndrome with unknown outcomes may result in a live birth, so the total number of live births is estimated at 18.[13]
Reasons for the development of Patau syndrome in the fetus
Patau syndrome can develop as a result of spontaneous duplication of chromosome 13 or, less commonly, due to the so-called Robertsonian translocation with the presence of an additional chromosome 13 attached to another chromosome or when only part of chromosome 13 is duplicated.
Robertsonian translocation
If a Robertsonian translocation has occurred, one of the parents is likely to be its carrier, despite the fact that he himself is healthy. Therefore, the presence of a translocation can be determined by the parental karyotype (blood test).
Sometimes the phenomenon of mosaicism occurs. This suggests the presence of an extra chromosome 13 in only some cells of the body. In this case, the severity of the disease depends on the ratio of “healthy” and abnormal cells.
Prevention
Patau syndrome is a disease that occurs unpredictably. At this point in time, doctors have not developed specific recommendations that, if followed, could prevent this disease in newborns.
All that can be said for certain is that in case of hereditary or genetic diseases in the family, as well as the mature age of the parents, one should consult with a specialist, undergo all the necessary examinations and be tested for laboratory genetic studies.
Symptoms of Patau syndrome
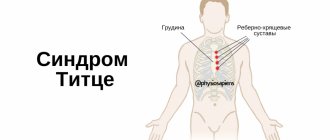
Patau syndrome is usually diagnosed after birth based on the presence of birth defects and a neurological examination. The most sensitive to the presence of abnormalities in genetic material are the central nervous system and the circulatory system.
Children with Patau syndrome have a low Apgar score soon after birth. Birth defects observed immediately after birth:
- cleft lip and/or palate;
- complete absence or deformation of the nose;
- microcephaly, microophthalmia (small eyes), anophthalmos (no eyeballs);
- hypotelorism (reduced distance between the eyeballs);
- foot deformity (absence or reversal of the longitudinal arches of the foot, positioning of the foot in plantar flexion, with the front part raised), polydactyly (extra fingers and toes);
- umbilical hernia and neural tube defects;
- In 80% of cases, heart defects are observed, that is, patent ductus arteriosus, ventricular and/or atrial septal defect and dextrocardia (position of the heart on the right side of the chest);
- Holoprosencephaly, which is a situation where the brain was not completely divided into the left and right hemispheres, is common. It is the cause of serious neurological disorders.
No nose
Polydactyly
Umbilical hernia
Because of the high risk of death immediately after birth, any possible decisions regarding surgery (eg, palate reconstruction) are postponed until later in the child's life.
The most common causes of death in children with Patau syndrome include cardiovascular failure, congenital heart defects, and pneumonia. People with this congenital disorder have severe mental retardation and developmental delays. These children are at increased risk of cancer.
Links[edit]
- ^ ab "Trisomy 13: a brief description". GOV.UK.
_ - "Prevalence and incidence of Patau syndrome". Disease Center - Patau Syndrome
. Adviware Pty Ltd. 2008-02-04. Retrieved February 17, 2008. the average maternal age for this anomaly is about 31 years - About.com> Patau Syndrome (trisomy 13) by Chrissy Danielsson. Updated June 10, 2009
- H. Bruce Ostler (2004). Diseases of the eyes and skin: color atlas. Lippincott Williams and Wilkins. paragraph 72. ISBN 978-0-7817-4999-2. Retrieved April 13, 2010.
- "Trisomy 13: MedlinePlus Medical Encyclopedia". Retrieved April 12, 2010.
- Callahan, Tamara L., and Aaron B. Caughey. Obstetrics and gynecology drawings. Baltimore, MD: Lippincott Williams & Wilkins, 2013.
- Janvier, Annie; Farlow, Wilfond (1 August 2012). "The experiences of families with children with trisomy 13 and 18 on social media". Pediatrics
.
130
(2):293–298. DOI: 10.1542/peds.2012-0151. PMID 22826570. - "Patau Syndrome". StatPearls
. StatPearls. 2021. - "Patau Syndrome (Trisomy 13)". Retrieved July 3, 2014.
- Nelson, Catherine E.; Rosella, Laura C.; Mahant, Sanjay; Guttmann, Astrid (2016). "Survival and surgical interventions for children with trisomy 13 and 18". JAMA
.
316
(4):420–8. DOI: 10.1001/jama.2016.9819. PMID 27458947. Retrieved December 3, 2021. - sind / 1024
in Who Named It? - Patau K, Smith DW, Terman E, Inhorn SL, Wagner HP (1960). "Multiple congenital anomaly caused by an additional autosome." Lancet
.
1
(7128): 790–3. DOI: 10.1016/S0140-6736(60)90676-0. PMID 14430807. - "National Cytogenetic Down Syndrome Registry Annual Reports 2008/09". Archived from the original on 2010-04-15.
When can the disease be detected?
In some cases, abnormalities suggestive of Patau syndrome can be detected by tests performed in the first trimester of pregnancy. For this purpose, an ultrasound scan with neck transillumination assessment and the PAPPA test are prescribed.
Ultrasound
If a pathology is detected, the doctor will recommend an abortion. The method of abortion depends on the stage of pregnancy at which the pathology was diagnosed.
If Patau syndrome is suspected only after the birth of the child, it will be necessary to carry out cytogenetic tests to make a definitive diagnosis. Due to the frequent occurrence of heart defects, the child also needs to have a heart ultrasound. Often expensive imaging tests are required: computed tomography (CT) and magnetic resonance imaging (MRI) to detect abnormalities in the brain and kidneys.
Throughout the entire diagnostic process, the assistance of a genetic counseling center is extremely important, where parents have the opportunity to receive:
- information on the mechanism of occurrence of the defect (spontaneous trisomy or carrying an additional fragment of chromosomes in one of the parents);
- prognosis for the child's condition;
- information on the risk of the defect occurring in subsequent children, etc.
Treatment
Typically, treatment for Patau syndrome is prescribed to each child individually, if possible. Surgery is often performed to correct birth defects. General strengthening therapy is prescribed to restore the level of immunity and other important functions of the body.
Each treatment is for specific physical problems that are present in the baby at birth. But it is definitely impossible to do without surgical intervention. At the same time, a cleft lip or cleft palate can be corrected with surgery, and in the future such children need repeated help from a speech therapist, professional and physical therapy. Therefore, the child must be provided with appropriate care and adequate nutrition.
But it is still impossible to fully cure this disease, since it occurs at the genetic level, which cannot be corrected due to many difficulties.
Will the next child get sick?
The risk of Patau syndrome in subsequent children is closely related to the underlying cause of the disease in the first child, as well as to the age of the mother.
In the case of spontaneous trisomy, the risk of developing trisomy 13 (and trisomy 21 and 18, i.e. Down syndrome and Edwards syndrome, respectively) increases by 0.5% compared with the existing risk associated with maternal age.
In the case of Robertson's translocation, the probability of recurrence of the situation can vary from a few percent to 100%. Risks are determined individually based on the results of genetic tests.
MAKE AN APPOINTMENT
[contact-form-7 id=”296″ title=”Untitled”]
Abortion and contraception clinic in St. Petersburg - department of the medical gynecological association "Diana"
Make an appointment, tests or ultrasound via the contact form or by calling +8 (812) 62-962-77. We work seven days a week from 09:00 to 21:00.
We are located in the Krasnogvardeisky district, next to the Novocherkasskaya, Ploshchad Alexander Nevsky and Ladozhskaya metro stations.
The cost of a medical abortion in our clinic is 3,300 rubles. The price includes all pills, an examination by a gynecologist and an ultrasound to determine the timing of pregnancy.
Diagnostic measures
Diagnosis of this pathology, like any other genetic disease, is carried out prenatally and postnatally. Prenatal detection of such anomalies allows us to compare the possible risks of giving birth to a sick child. Prenatal diagnostic methods are divided into invasive and non-invasive.
Non-invasive methods are considered safe. Fetal material is not required to detect a genetic abnormality. Ultrasound examination of the fetus and Dopplerography of the uteroplacental blood flow are recommended for all pregnant women. Diagnosis using ultrasound is 100% reliable.
Standard prenatal screening includes a blood test for biochemical markers. The results obtained are correlated with the age of the pregnant woman and gestational age. If the data obtained is outside the normal range, doctors recommend terminating the pregnancy. The analysis requires venous blood from a pregnant woman, which contains fragments of the genetic structure of the fetus.
Invasive methods include:
- Chorionic villus biopsy, which allows diagnosing the disease from 8 to 12 weeks of pregnancy. One of the membranes is taken for analysis using a puncture needle. A small amount of material is sufficient for research.
- Amniocentesis is the collection of amniotic fluid with a special needle through the peritoneum for cellular analysis. The method is relevant from 14 to 18 weeks of pregnancy. The study is carried out under ultrasound control. Cells containing fetal DNA are tested for genetic diseases.
- Cordocentesis is a study of fetal cord blood that allows one to determine genetic abnormalities with high accuracy. It is carried out after the 20th week of gestation.
Despite the high accuracy and reliability of invasive methods, they are used only in extreme cases. Introduction into the body of a pregnant woman and penetration into the membranes of the fetus carries a certain risk. Any incorrect movement by the specialist performing the procedure can lead to intrauterine death of the fetus.
The diagnosis is made after determining the baby's karyotype by qf-PCR. Only DNA analysis can confirm or refute the alleged diagnosis. Using chromosomal studies, it is possible to determine whether a child has trisomy 13, whether the anomaly has a hereditary etiology or is caused by a spontaneous intrauterine mutation. To assess the risks and be able to prevent such mutations, parents must undergo a detailed genetic study, which gives a 100% result. Genetic testing is carried out even if intrauterine death of the fetus has occurred, in order to prevent the syndrome during a second pregnancy.
Postnatal diagnosis consists of examining the newborn by a neonatologist and identifying clear and specific symptoms. Sick children are advised to undergo a thorough comprehensive examination, including the following instrumental techniques:
- Cardiography – electrocardiography, phonocardiography, coronary angiography, magnetocardiography;
- Ultrasound of internal organs located in the abdominal cavity and pelvis: pancreas, kidneys, ureters, organs of the reproductive system;
- Neurosonography - ultrasound of the brain;
- Tomographic examination of brain structures - CT or MRI.
Sick children usually require consultation with doctors - specialists in the field of ophthalmology, otolaryngology, neurology, pediatric surgery, genetics, endocrinology, and psychiatry.