Rosuvastatin tablets are designed to reduce the production of your own cholesterol in the body. When the levels of this organic compound in the blood increase, the risk of developing atherosclerotic changes in capillaries, cardiac ischemia, heart attack and stroke increases significantly. Therefore, proper therapy is important in the initial stages, as soon as test results show elevated total cholesterol levels.
In the initial stages, when the excess of the permissible norm is small, the patient is prescribed a special diet with limited fatty foods. Thus, the use of lipid-lowering drugs, such as Rosuvastatin, gives the maximum effect. This material covers selected instructions for using the drug.
Composition and effect of the drug, indications for use
The tablet prescription in Latin is written as Rosuvastatin. The drug belongs to the group of lipid-lowering drugs (statins) and is an inhibitor of HMG-CoA reductase. Designed to reduce the production of own cholesterol by liver tissue and reduce the volume of harmful lipoproteins (having a low density) in the blood plasma.
One tablet, coated with a soluble film coating, contains the active component of rosuvastatin calcium (in a dosage of 5 to 40 mg) and excipients in the form of cellulose, calcium dihydrate, magnesium stearate, povidone, corn starch and others. Manufacturers of the original drug Rosuvastatin are Russian pharmaceutical companies, JSC Vertex, LLC Izvarino Pharma.
Foreign manufacturers of drugs based on the substance rosuvastatin AstraZeneca, Gedeon Richter, KRKA, TEVA and others. The tablets can be stored for 3 years from the date indicated on the carton at a temperature below 25 °C. Rosuvastatin is dispensed from pharmacies with a doctor's prescription.
Indications for use:
- new-onset hypercholesterolemia;
- familial hypercholesterolemia of the heterozygous or homozygous type;
- high concentration of triglycerides in blood plasma;
- pathological state of capillaries in connection with manifestations of atherosclerosis, including progression of the disease (as a measure of complex treatment);
- prevention of cardiovascular diseases, including in elderly patients.
Medicines of the statin group are prescribed to patients who have not been helped by a diet combined with increased physical activity, frequent exposure to air, and quitting smoking and drinking alcohol.
Rosuvastatin price
On average, the price of this drug ranges from 200 to 600 rubles.
- Online pharmacies in RussiaRussia
- Online pharmacies in UkraineUkraine
ZdravCity
- Rosuvastatin-Canon tablets p.p.o.
10 mg 28 pcs. Canonpharma Production JSC 323 rub. order - Rosuvastatin-SZ tab. p/o captivity. 5mg 30pcsNAO Northern Star
RUB 219 order
- Rosuvastatin-SZ tab. p/o captivity. 0.01g 30pcsNAO Northern Star
RUB 279 order
- Rosuvastatin tablets p.p.o 20 mg 30 pcs Izvarino Pharma LLC
RUB 1,038 order
- Rosuvastatin tablets p.p.o. 10 mg 30 pcs. Ozone LLC
RUB 362 order
Pharmacy Dialogue
- Rosuvastatin-Teva tablets 20 mg No. 30Teva LLC
RUR 753 order
- Rosuvastatin-Teva tablets 10 mg No. 90 Teva LLC
RUB 1,277 order
- Rosuvastatin Canon tablets 10 mg No. 90Canonpharma Production
RUR 688 order
- Rosuvastatin-Teva tablets 5 mg No. 30Teva LLC
409 rub. order
- Rosuvastatin-Teva tablets 10 mg No. 30Teva LLC
RUR 573 order
show more
Pharmacy24
- Rosuvastatin Sandoz 5 mg No. 28 tablets Lek pharmaceutical company d.d., Slovenia
96 UAH. order - Rosuvastatin Sandoz 10 mg No. 28 tablets Lek pharmaceutical company d.d., Slovenia
130 UAH order
- Rosuvastatin Teva 10 mg No. 30 tablets TEVA Pharmaceutical Industries Ltd., Israel
101 UAH order
- Rosuvastatin Teva 5 mg No. 30 tablets TEVA Pharmaceutical Industries Ltd., Israel
73 UAH order
- Rosuvastatin IC 5 mg No. 30 tablets INTERCHEM Partnership with additional coverage, Ukraine
67 UAH order
Instructions for use and dosage
Taking the drug is not associated with eating food; there is no need to think about taking pills before or after meals. It is advisable to take Rosuvastatin at night, since at night the body's own cholesterol production increases. But such a measure is not necessary; it is enough to simply take the drug once every 24 hours without skipping, at approximately the same time.
Do not chew the tablet, swallow it whole with the required amount of water.
According to the official instructions for use, before starting to use the tablets, the patient is prescribed a low-fat diet so that the therapy brings maximum effect. The patient should limit the amount of salty, hot and spicy foods, refuse food containing large amounts of animal fats, carbonated drinks, baked goods, sausages, canned food and ready-made sauces.
You need to introduce as much fiber, vegetables and fruits into your diet as possible. Such a balanced diet should be maintained not only during the course of statin treatment, but also after its completion. The initial dosage recommended by doctors for patients for initial use or transferred to Rosuvastatin from other lipid-lowering drugs is 5–10 mg for 24 hours.
But the selection of the initial dose is made finally, based on the results of biochemical blood tests. The specialist also takes into account the patient’s risk of developing consequences from the heart and capillaries - heart attack, ischemia, heart failure.
If there are no side effects from using Rosuvastatin, the dosage can be increased if necessary after four weeks. If the result of taking tablets at a dosage of 20 mg does not provide a therapeutic effect or the cholesterol level as a result of the analysis is several times higher (for example, with familial hypercholesterolemia), the doctor prescribes Rosuvastatin at a dose of 40 mg per day and takes the patient under control.
No ads 1
The same dose is prescribed for people at high risk of heart complications. If the patient has not previously contacted specialists, has undergone examination and has not taken statin drugs, he should not be prescribed 40 mg tablets per day at once. Every two weeks during the course of therapy, the patient is advised to donate blood for biochemistry in order to monitor cholesterol levels over time.
Patients suffering from moderate or mild renal failure can take Rosuvastatin at an initial dosage of 5-10 mg. If these disorders are moderate or severe, statins are not prescribed. For liver diseases occurring in acute or chronic form, then during the acute stage, the use of Rosuvastatin is contraindicated.
Is it possible to divide the tablet in half, many patients ask, who are prescribed, for example, a dose of 10 mg per day, but the pharmacy only has a 20 mg release form. Firstly, when dividing the pills, the dosing accuracy may not be observed; this point is especially important for patients whose body reacts violently to even a slight excess of the specified dose.
Secondly, most tablets from the statin group, including Rosuvastatin, are coated with a soluble film coating. It protects the active components from the action of gastric juice. If the integrity of the tablet is violated, the components of the medicine enter into an undesirable reaction with the acidic environment of the stomach.
Too active release of the active substance and its absorption into the blood occurs due to the breaking of the pill into pieces
And the third problem is the impact of environmental factors on the divided tablet itself (light, humidity and heat). If half of such a pill has been left for several days, it may lose its medicinal qualities. The instructions for use of Rosuvastatin indicate that the tablet should not be chewed. Accordingly, it is undesirable to divide it into parts. It is better to buy a drug with a good shelf life in the required dosage and take it as recommended by the treating doctor.
No ads 2
Currently, in developed countries, up to 80–95% of patients with coronary heart disease (CHD) take statins. These figures indicate that cardiologists have no doubt about the advisability of such treatment. Indeed, in recent years, data from several very large studies have been published, which clearly indicate a decrease in mortality (both cardiovascular and general) during therapy with these drugs. In addition, many additional effects of statins have been described and can be used alone. This is, for example, a significant anti-ischemic effect observed with long-term use of these drugs. The anti-inflammatory effects of statins are so great that attempts are being made to treat rheumatoid arthritis with their help. There have been reports of the clinical effectiveness of statins in demyelinating diseases.
However, despite the widespread use of statins, target levels of lipids (primarily atherogenic fractions) are not always achieved. At the same time, a decrease in the incidence of complications of coronary atherosclerosis is associated with the correction of this particular risk factor. Attempts to combine statins with other lipid-lowering drugs are not always successful, as they can lead to the development of severe side effects (as was the case with cerivastatin, which in combination with fibrates led to the development of a large number of cases of rhabdomyolysis). There is evidence of the combined use of statins and nicotinic acid. However, nicotinic acid itself has a very wide range of side effects.
Currently, the use of maximum dosages of statins is actively recommended. However, this makes treatment so expensive that even in developed countries this approach is not widely used. Thus, monthly treatment with atorvastatin (the most popular statin in the United States) at a dose of 80 mg (excluding the cost of monitoring safety parameters) will cost almost $400. In our country, where such a dosage is not registered, taking 8 tablets (10 mg) of atorvastatin per day will cost the patient $400–500 monthly. But even such doses do not always lead to achieving the target level of low-density lipoproteins (LDL).
Comparison of moderate and aggressive lipid-lowering statins
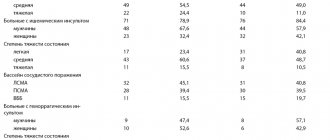
During 2004, the results of 2 interesting studies were published comparing statins - pravastatin, which has a very moderate effect on LDL levels, and atorvastatin, which reduces LDL levels to a much greater extent. The data obtained indicate that the administration of statins, which intensively lower lipid levels, leads to a more pronounced clinical effect.
REVERSAL Study
This study (Reversal of Atherosclerosis with Aggressive Lipid Lowering) compared the effect of 40 mg of pravastatin and 80 mg of atorvastatin per day on the dynamics of atherosclerotic lesions of the coronary bed by changes in the volume of coronary atheroma [1]. Of the 2163 patients screened, 654 patients were randomized and received study drugs. Of these, 502 patients were able to perform intravascular ultrasound of satisfactory quality at baseline and after 18 months of therapy, with 249 patients included in the pravastatin group, 253 in the atorvastatin group. The baseline LDL level in both groups was 150.2 mg/dL (3.89 mmol/L). During treatment with pravastatin, the content of this fraction decreased to 110 mg/dl (2.85 mmol/l), and when using atorvastatin - to 79 mg/dl (2.09 mmol/l). According to this indicator, the differences turned out to be highly significant (p
The studied statins had different effects on atheroma volume. If atherosclerotic lesions progressed during treatment with pravastatin (increase by 2.7%, p = 0.001), then in the atorvastatin group its volume did not change.
PROVE-IT Study – TIMI-22
The Pravastatin or Atorvastatin Evaluation and Infection Therapy – Thrombolysis in Myocardial Infarction 22 (PROVE-IT – TIMI-22) study also compared the effects of atorvastatin (80 mg/day) and pravastatin (40 mg/day) [2].
4162 patients were randomized - men and women over 18 years of age who were hospitalized for acute coronary syndrome (with or without ST-segment elevation) or who had an episode of high-risk unstable angina within 10 days before inclusion in the study. Total cholesterol levels should not exceed 240 mg/dL (6.21 mmol/L) or 200 mg/dL (5.18 mmol/L) if patients had previously received statins. The study did not include patients who had previously received statins at a dose of 80 mg/day, or patients using drugs metabolized by the 3A4 isoenzyme of the cytochrome P450 system.
The pravastatin group included 2063 patients and the atorvastatin group - 2099. The groups were completely comparable in all main clinical characteristics, with the exception of the incidence of peripheral atherosclerosis, which was more often observed among patients receiving pravastatin (p = 0.03). The follow-up period ranged from 18 to 36 months (average 24 months). After 925 endpoints were recorded, the study was stopped.
Endpoints included death from any cause, myocardial infarction, documented unstable angina requiring hospitalization, revascularization (angioplasty or coronary artery bypass grafting) performed more than 30 days after randomization, and stroke.
A significant difference between the groups in LDL levels was noted already from the 30th day of treatment. When using pravastatin, its average concentration was 95 mg/dl (2.46 mmol/l), and in the atorvastatin group it was 62 mg/dl (1.60 mmol/l). In patients previously treated with statins, additional pravastatin did not reduce LDL levels, while atorvastatin reduced their concentration by another 32%. In patients who had not previously taken statins, LDL cholesterol levels decreased by 22% when treated with pravastatin, and by 51% when using atorvastatin. At the same time, the level of high-density lipoproteins (HDL) increased to a greater extent in the pravastatin group (8.1 vs. 6.5%, p
Differences in the degree of reduction in CRP levels also turned out to be highly significant. Although its content significantly decreased in both groups, with pravastatin its level decreased to 2.1 mg/l, and with atorvastatin - to 1.3 mg/l (initial level - 12.3 mg/l in both groups ).
The main result of the study was a 16% (p = 0.005) lower incidence of endpoints in the atorvastatin group. During 2 years of observation, the incidence of adverse outcomes with pravastatin was 26.3%, and only 22.4% with atorvastatin. The difference between the groups began to be noted on day 30 of treatment and persisted throughout the study.
During treatment with atorvastatin, the incidence of unstable angina requiring hospitalization (by 29%, p = 0.02) and the need for revascularization (by 14%, p = 0.04) were significantly lower. Reductions, although not significant, were also observed in the risk of death from any cause (by 28%, p = 0.07) and the combined endpoint of death + myocardial infarction (by 18%, p = 0.06). Stroke was rare in both groups, and there was no significant difference in this endpoint between the groups.
The benefit of atorvastatin was greatest in patients with baseline LDL levels greater than 125 mg/dL (34% risk reduction for the composite endpoint, p = 0.02) and in patients who had not previously received statins.
The importance of the results demonstrating a clear advantage of atorvastatin also lies in the fact that they were obtained in a study conducted by the company that produces pravastatin, whose specialists had reason to assume completely different results. The main hypothesis underlying the protocol was that there would be no difference in the clinical effects of the two statins, despite differences in lipid-lowering effects.
The concept is the lower the better”
In July 2004, amendments to message 3 of the US National Cholesterol Education Program were published in the journal Circulation [3]. Based on the results of recently published studies, it was decided to significantly tighten the requirements for blood LDL levels (Table 1).
It is proposed to identify 4 risk groups for the development of coronary death over the next 10 years. The high-risk group includes conditions that correspond to the risk of a heart attack or coronary death in more than 20% of cases over the next 10 years. This is a history of coronary artery disease (myocardial infarction, unstable angina, stable angina, revascularization procedures), signs of significant myocardial ischemia. In addition, this risk is caused by the presence of so-called CHD risk equivalents in the patient. This is clinically significant non-coronary atherosclerosis, diabetes mellitus, or a combination of conditions in which the risk exceeds 20%.
In this group of patients, LDL levels should be below 100 mg/dL (2.6 mmol/L). However, there is evidence that this goal may be to reduce LDL concentrations below 70 mg/dL (1.8 mmol/L), especially in patients at very high risk (acute coronary syndrome). If the LDL level in such patients is greater than or equal to 2.6 mmol/l, lipid-lowering therapy is required along with lifestyle changes. However, there is evidence that statin therapy is indicated for such patients even in cases where the initial LDL level is below 2.6 mmol/l. High triglyceride levels or low HDL levels are an indication for additional fibrates or niacin. Moreover, if the concentration of triglycerides is above 2.3 mmol/l, then one of the goals of therapy is to achieve the level of atherogenic fractions of cholesterol (cholesterol of all fractions except HDL) below 3.4 mmol/l (0.8 mmol/l above the target LDL level ).
The next gradation – high intermediate risk – involves a combination of 2 or more risk factors, in which the incidence of myocardial infarction or coronary death over the next 10 years is 10–20%. This risk is caused by a combination of smoking and an increase in blood pressure over 140/90 mm Hg. Art., low HDL level (
The risk based on these factors is calculated using special calculator programs (on the Internet, such a calculator is located at www.nhlbi.gov/guidelines/cholesterol).
Intermediate risk is a combination of 2 or more risk factors for which the 10-year risk calculated using a calculator does not exceed 10%.
When lipid-lowering drugs are used in high- and intermediate-risk groups, LDL levels should be reduced by at least 30–40%.
It is also important that all patients actively adjust their lifestyle (increase in physical activity); carried out therapy aimed at reducing excess body weight and treating metabolic syndrome, eliminating hypertriglyceridemia and increasing HDL levels if they decreased.
In the low-risk group (0–1 risk factor), the risk of CAD should not be calculated.
European recommendations for the prevention of cardiovascular diseases are based not on calculating the risk of complications of coronary atherosclerosis, but on taking into account the total risk of cardiovascular diseases, including stroke.
The place of the anti-inflammatory effect in the antiatherogenic action of statins
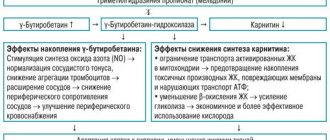
The large number of effects of statins that are not associated with a decrease in the level of atherogenic lipoproteins allows us to seriously discuss the question of what is more important - their effect on cholesterol synthesis or other consequences of blockade of mevalonic acid metabolism.
The anti-inflammatory effect of statins has received the most attention. The participation of inflammatory reactions in atherogenesis is now considered proven. It has been established that the prognosis for atherosclerotic lesions of various locations can be significantly clarified by measuring the level of inflammatory markers in the systemic circulation. Most often, this is done by determining the level of CRP using a highly sensitive technique. Based on data from large epidemiological studies, it is proposed to divide the CRP level into 3 ranges: low - less than 1.0 mg/l, medium - 1.0-3.0 mg/l and high - more than 3.0 mg/l. A CRP level above 10 mg/L indicates the presence of causes for a systemic inflammatory response, such as infection, trauma, etc. To assess the risk of atherosclerosis, this test should be repeated 2 weeks after the relief of these conditions.
CRP is a non-glycosylated protein, the main regulator of whose synthesis is interleukin 6. The stimulus that provokes the synthesis of CRP can be oxidized lipoproteins. Until recently, it was believed that CRP is synthesized by hepatocytes, but recently it has been discovered that it can also be produced in atherosclerotic plaques, kidneys, nervous tissue and alveolar macrophages. Recently, information has emerged that CRP is not only a marker of the inflammatory process in atherosclerosis, but is itself an active factor in atherothrombosis.
The effect of CRP on endothelial cells leads to a decrease in the activity of endothelial NO synthetase, a decrease in the synthesis of prostacyclin, an increase in the production of type 1 plasminogen activator inhibitor, endothelin-1, interleukins 6 and 8, and some cell adhesion molecules that provoke the migration of macrophages into the subendothelial layer. The proatherogenic effect of CRP on smooth muscle cells is manifested by the acceleration of their proliferation, increased expression of angiotensin type 1 receptors and an increase in the level of inducible NO synthetase. The latter synthesizes nitric oxide, which is spent mainly on the formation of a very aggressive radical - peroxynitrite. Macrophages under the influence of CRP more actively produce free radicals, cytokines (interleukins 1 and 6, tumor necrosis factor), tissue factor, etc. [4]. All this confirms the direct participation of CRP in the processes of atherogenesis. Therefore, reducing its level can be considered as one of the main goals of pathogenetic treatment of atherothrombosis.
To date, several studies have been published comparing the effects of different statin regimens on CRP levels. A randomized, placebo-controlled trial of 110 patients compared the effects of treatment with atorvastatin (10–80 mg, target LDL level less than 2.1 mmol/L) and lovastatin (5–10 mg, target LDL level less than 3.4 mmol/L). l). A significant decrease in CRP levels (from 2.6 to 1.7 mg/l, p = 0.002) was achieved only with intensive lipid-lowering therapy with atorvastatin. In other words, there is a parallel between the effects of statins on lipids and inflammatory markers.
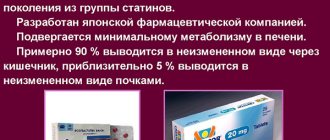
Rosuvastatin is the most effective statin
Rosuvastatin (Crestor) is a completely synthetic drug of the statin group, approved for clinical use in 2003. Due to its obvious advantages, the demand for rosuvastatin turned out to be very high. This is evidenced by the fact that since registration it has already been prescribed to more than 2.5 million patients, despite the presence of 5 other statins on the pharmaceutical market.
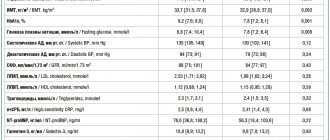
The pharmacokinetic characteristics of rosuvastatin and other currently used statins are presented in table. 2. After a single dose of rosuvastatin, its maximum concentration in the blood is reached after approximately 5 hours. The drug has the longest half-life - 19 hours. This may be due to the phenomenon of enterohepatic recirculation demonstrated experimentally. Approximately 88% of rosuvastatin is reversibly bound to plasma proteins, mainly albumin.
The pharmacokinetic characteristics of rosuvastatin are not affected by age, gender, time of drug administration or concomitant food intake, as well as the presence of moderate liver failure.
The rosuvastatin molecule is hydrophilic, which makes it more selective towards hepatocytes than other tissues. Another consequence of the hydrophilicity of this drug is its significantly less effect on cholesterol synthesis in skeletal muscle myocytes. In studies conducted on cultured skeletal muscle cells, rosuvastatin and another hydrophilic statin, pravastatin, reduced the activity of cholesterol synthesis to a much lesser extent (50-1000 times) than the lipophilic atorvastatin, simvastatin and cerivastatin. This fact allows us to consider rosuvastatin potentially safer compared to other drugs from the statin group.
It has been shown that 90% of the drug is excreted in feces, and 10% in urine. Only 10% of rosuvastatin is metabolized; its main metabolite, N-desmethyl rosuvastatin, is approximately 2 times less active than the main substance. Unlike most statins (in particular, atorvastatin and simvastatin), rosuvastatin interacts minimally with enzymes of the cytochrome P450 system, and therefore the likelihood of its interaction with many widely prescribed drugs (antihistamines, antifungals, antiulcers, a number of antibiotics, antidepressants, cardiac glycosides, etc.) is minimal. In particular, the drug does not have an inhibitory effect on isoenzymes 1A2, 2C19, 2D6, 2E1 and 3A4. Only for the 2C9 isoenzyme, a decrease in its activity by 10% was noted. When rosuvastatin was co-administered with fluconazole (a potent inhibitor of the 2C9 isoenzyme), only a slight increase in statin concentrations was observed.
The clinical effectiveness of rosuvastatin is being actively studied in a series of studies, the program of which is called GALAXY (45 thousand participants). This program examines the effects of rosuvastatin on lipids, inflammatory markers, the dynamics of the atherosclerotic process and so-called fixed (or “hard”) endpoints. The program covers most of the conditions for which statins are currently used.
However, the greatest interest is in the AURORA study, which examined the effect of the drug in patients on hemodialysis; the CORONA trial, which included patients with heart failure, and the JUPITER trial, which focused on primary prevention in patients with normal LDL levels and elevated CRP levels. All these studies are ongoing and their results will resolve a number of unexplored issues.
Among those completed, the MERCURY I (Measuring Effective Reductions in Cholesterol Using Rosuvastatin therapy) study was of great importance for assessing the effectiveness of rosuvastatin. This open-label, randomized trial included 3161 patients with hyperlipidemia [5]. Its purpose was to compare the effectiveness of rosuvastatin, atorvastatin and other statins in terms of reducing LDL concentrations. The main criterion for assessing effectiveness was achieving the target LDL level. The study lasted 16 weeks.
The result of the study was the demonstration of a significant advantage of rosuvastatin over other statins in terms of their effect on lipids. The target LDL level while taking rosuvastatin at a dose of 10 mg/day was achieved in 86% of patients compared to 80% when using a similar dose of atorvastatin (p
Currently, rosuvastatin is recommended for use in dosages of 10–40 mg per day. At the same time, LDL levels are reduced by 52–63%, i.e. to a much greater extent than when using other statins in similar doses. In addition, treatment with rosuvastatin significantly increased the concentration of HDL by 14% and decreased the level of triglycerides by 28%.
Reducing the level of atherogenic fractions of cholesterol (primarily LDL cholesterol) is not the only goal of lipid-lowering therapy. It should also be aimed at correcting the content of HDL, a potentially antiatherogenic fraction of lipoproteins, the level of which is reduced in many patients.
At the last European Congress of Cardiology (2004), the results of the largest population-based study INTER-HEART were presented. It showed that 9 potentially modifiable factors determine the risk of myocardial infarction by 90%, with the most significant of them being the ApoB/ApoA1 ratio. In second place in importance is smoking, followed by diabetes mellitus, arterial hypertension, abdominal obesity, psychosocial factors, the amount of fruits and vegetables consumed, physical inactivity and alcohol consumption [6].
The fact that the most significant was the ratio of ApoB, the only protein included in LDL, to ApoA1, the HDL protein, once again confirms the special importance of maintaining this fraction of lipoproteins at an optimal level. The main competitor of rosuvastatin, atorvastatin, has a very slight effect on HDL concentrations. Moreover, as the dose of atorvastatin increases, the extent of its effect on HDL decreases.
Rosuvastatin behaves in the opposite way. The STELLAR study [7] showed that differences between it and atorvastatin in the effect on HDL appeared already when using these drugs at a dose of 10 mg, and when taking statins at a dose of 20 mg, the difference became highly significant. When using rosuvastatin at a dose of 10 mg, the level of ApoB decreased by 38%, and the concentration of ApoA1 increased by 5%. As a result, the ApoB/ApoA1 ratio decreased by 40%.
The pronounced hypotriglyceridemic effect of rosuvastatin can be considered proven in patients with initial triglyceride levels in the range from 3.4 to 9 mmol/l [8]. A randomized, placebo-controlled study that included 156 such patients showed that a 6-week course of rosuvastatin therapy leads to a decrease in triglyceride levels by 37–40%, and cholesterol of all atherogenic fractions by 42–51%. In parallel, HDL levels increase by 6–18%. This feature of the action of rosuvastatin allows us to expect that its widespread introduction into clinical practice will significantly reduce the need for the combined prescription of statins and fibrates.
Safety of rosuvastatin
The problem of treatment safety is the most important aspect of the use of any medicine. It becomes especially important when introducing into clinical practice a drug intended for a very large number of patients. Attention to the safe use of statins has increased sharply after the withdrawal of cerivastatin from the market, the uncontrolled use of which led to a large number of fatal complications.
The emergence of a new drug in this class, rosuvastatin, opened a discussion about the advisability of registering a new drug in conditions where a significant number of statins already exist and are actively used. That is why rosuvastatin has undergone very careful study from a safety point of view. Information for this drug was analyzed on twice the number of patients required for registration of other statins. One of the consequences of this test was some delay in the release of the drug to the market. On the other hand, its results allow us to confidently assert that, subject to dosages and rules for prescribing rosuvastatin, its use is at least as safe as other statins.
However, some precautions common to all statins must be taken when using rosuvastatin. Thus, in some patients, while using high doses of rosuvastatin, proteinuria may be observed, associated with the development of a kind of tubulopathy, which is also observed in 0.2–0.6% of cases when using other statins. Therefore, the drug should not be prescribed in a dose of 40 mg to patients with creatinine clearance less than 60 ml/min and in any dosage with creatinine clearance below 30 ml/min. In any case, when prescribing 40 mg of rosuvastatin, it is necessary to monitor the level of proteinuria.
Like other statins, rosuvastatin should be used cautiously in patients who abuse alcohol and have liver disease. All patients need to determine the level of liver transaminases initially and after 3 months of therapy. An increase in their level by more than 3 times is a reason to reduce the dose or discontinue the drug.
Pharmacokinetic studies have shown that patients belonging to the Mongoloid race are more sensitive to the effects of statins. Therefore, when prescribing rosuvastatin to such patients, slightly lower dosages should be used and the drug should not be used at a dose of 40 mg.
The most serious, although extremely rare, side effect of any statin is the development of rhabdomyolysis. Before starting the use of rosuvastatin, it is necessary to measure the initial level of creatine phosphokinase. If it increases more than 5 times after 5-7 days, the analysis must be repeated - if the increase persists, rosuvastatin therapy is not started. It was found that myopathy and rhabdomyolysis are more common in patients with kidney damage and hypothyroidism; in the presence of congenital muscle diseases in relatives; in patients who had signs of muscle tissue damage while taking other statins and fibrates; in persons who abuse alcohol; in cases where the drug is used in combination with fibrates. Such patients should not be prescribed rosuvastatin at a dose of 40 mg. The presence of myopathy is a contraindication to the use of the drug in all dosages.
Rosuvastatin is also contraindicated in women during pregnancy and lactation. It should not be prescribed to patients with preserved reproductive function if they do not use contraception.
In general, the safety profile of rosuvastatin does not differ from that of other statins. To date, its safety has been studied in more than 15 thousand patients, 1500 patients have taken the drug for more than 2 years. More than 45 thousand people are currently participating in controlled studies of rosuvastatin.
Thus, the feasibility of the widest use of statins in clinical practice does not raise any doubts today. In our country, as well as throughout the world, there are practically no doctors left who are unfamiliar with the therapeutic possibilities provided by drugs of this class. Unfortunately, statins are not always used correctly, in adequate dosages, which, of course, significantly reduces the effectiveness of their use as a means of preventing severe complications of atherosclerosis. A new representative of this class, rosuvastatin (Crestor), now available in Russia, surpasses all other statins in its ability to reduce the level of proatherogenic lipoproteins. Its most important advantages are also its beneficial effect on antiatherogenic fractions of lipoproteins (primarily HDL) and a powerful hypotriglyceridemic effect. This reduces the need for combined administration of statins and fibrates, which significantly increases the safety of lipid-lowering therapy. In addition, the effectiveness of the drug in most patients at an initial dose of 10 mg reduces the need for titration compared to other statins, increases adherence to treatment, and reduces the cost of therapy. Some features of the pharmacokinetics and pharmacodynamics of rosuvastatin allow us to expect better tolerability of this drug compared to other statins.
Contraindications
The abstract for the drug Rosuvastatin lists the following factors under which doctors do not risk prescribing Rosuvastatin to patients even in a small dosage of 10 mg-20 mg:
- acute reaction of the body to substances from the statin group, including rosuvastatin;
- high activity of liver transaminases;
- diseases of the liver and kidneys in acute form or in chronic form, but in the acute stage;
- lactase deficiency;
- glucose-galactose malabsorption;
- severe renal failure;
- disturbances in the functioning of the endocrine system, in particular the thyroid gland;
- pathologies of joints and muscles that increase susceptibility to myalgia and rhabdomyolysis;
- simultaneous use of medications of the fibrate group and Cyclosporine;
- alcohol addiction.
If cholesterol levels are elevated in patients with alcohol dependence, the doctor evaluates the condition of the internal organs during the examination. In the absence of violations on the part of these systems, the specialist may prescribe Rosuvastatin in a minimum dosage, provided that the patient is ready to stop drinking alcohol during and after treatment.
If liver pathologies already have a pronounced course against the background of alcoholism, such patients should not use statins. Pregnancy and breastfeeding are also contraindications to the use of Rosuvastatin. Some components of the drug penetrate into milk, causing allergic reactions, digestive problems and other negative consequences in the newborn.
During pregnancy, active substances pass through the placental barrier, causing intrauterine malformations. Therefore, a woman who is undergoing treatment with Rosuvastatin should be aware of the consequences of an unexpected pregnancy during this period. She will have to have an abortion, due to the high risk of defects in the unborn child, or use effective methods of contraception in advance.
What do drugs have in common?
To understand what the difference is and which drug is better - Rosuvastatin or Atorvastatin, it is necessary to conduct a comparative analysis. Both drugs under consideration are representatives of the new generation of statins. It is necessary to select one that, along with a noticeable therapeutic effect, has minimal side effects.
Their mechanism of action is approximately the same, but there are slight differences. If you understand the difference between them, you can adjust the treatment of a particular patient, which will significantly improve the prognosis for his recovery. The commonality between Rosuvastatin and Atorvastatin is that both drugs have a dual effect - they reduce the level of bad cholesterol and increase the content of good cholesterol.
Also common to these two drugs is that they:
- improve the condition of the inner lining of blood vessels during its dysfunction;
- improve blood flow through vessels;
- have a beneficial effect on the vascular wall.
Both drugs have common indications for use. Since they belong to the latest generation of statins, they can be prescribed not only for the treatment of diseases, but also for their prevention, which was difficult with the first and second generation statins due to the many side effects from them.
Therefore, the drugs in question are recommended for use in patients who have an increased risk of developing coronary heart disease. Factors that increase this risk include:
- age over 55 years;
- a history of diabetes mellitus;
- addiction to smoking;
- high blood pressure;
- hereditary predisposition to high cholesterol;
- reduced levels of high-density lipoproteins in the blood.
Atorvastatin and Rosuvastatin are not prescribed for the treatment of children and adolescents, during breastfeeding and pregnancy, or in the acute stage of liver disease. They are used with caution if the patient suffers from alcoholism, is predisposed to myopathy, or has a history of renal failure.
The maximum therapeutic effect from taking new generation statins is achieved after 4 weeks from the start of treatment. If the medicine is taken by a woman who has retained reproductive capabilities, then she is recommended to take care of reliable contraception along with statins.
Both drugs have minimal side effects and are therefore well tolerated by patients. They can be taken regardless of food intake and without reference to a specific time of day.
High levels of “bad” cholesterol lead to blockage of blood vessels
Side effects
The main side effects of the drug Rosuvastatin occur in the nervous system. This happens more often when the dosage is incorrectly selected or when patients do not comply with medical recommendations for taking the pills, since they are well tolerated in an appropriate dose.
Such negative effects include headaches and dizziness, an unreasonable feeling of anxiety, irritability or, conversely, apathy. Sleep disturbances with nightmares that were not there before may appear. When the stomach and intestines are weak, diarrhea, bloating, and attacks of nausea and vomiting occur in response to taking statins.
The drug is a representative of the statin group
Constipation alternating with diarrhea is accompanied by pain in the epigastric region, transient jaundice, and pancreatitis may worsen. Chronic gastritis is a relative contraindication to the use of Rosuvastatin, since it can worsen during the course of treatment.
Other negative effects that may occur after taking Rosuvastatin:
Lowering cholesterol without statins
- from the respiratory system - the development of infections of the larynx and nasal sinuses (laryngitis, pharyngitis, sinusitis), primary manifestations of bronchial asthma, accompanied by shortness of breath, dry paroxysmal cough. In rare cases, interstitial lesions of the pulmonary system develop with chest pain, laryngeal cough and respiratory distress;
- from the urinary system - infections of the kidneys, bladder and excretory canals, nagging pain in the lower abdomen, swelling of the lower extremities;
- allergic manifestations - skin rashes like urticaria, in isolated cases angioedema;
- other body systems - the development of non-insulin-dependent diabetes mellitus, a sharp decrease in hemoglobin, thrombocytopenia, influenza-like syndrome, damage to the roots of teeth with the formation of purulent abscesses.
With long-term use of Rosuvastatin, some men experienced signs of erectile dysfunction, and women experienced gynecomastia. A few patients complained of persistent insomnia, as a result of which they developed depressive states.
Side effects
This drug has a wide range of side effects:
Musculoskeletal system:
- arthritis;
- myopathy;
- backache.
Nervous system:
- dizziness;
- headache;
- neuralgia;
- state of anxiety, depression;
- insomnia.
Respiratory system:
- cough;
- asthma;
- pneumonia;
- bronchitis;
- pharyngitis;
- rhinitis.
Urinary system:
- infections;
- pain in the lower abdomen.
Gastrointestinal tract:
- diarrhea;
- vomit;
- nausea;
- constipation;
- gastritis.
Heart rate:
- cardiopalmus;
- angina pectoris.
Important points and cross-talk
Rosuvastatin should not be prescribed to patients after major surgical interventions, suffering from severe forms of arterial hypertension, severe metabolic disorders and uncontrolled epilepsy. Serious injuries, disturbances in the water-electrolyte balance in the body and the consequences of blood poisoning are also indications for which it is necessary to assess the possible risks of prescribing the drug.
What medications are currently recommended for the patient is a very important point when prescribing Rosuvastatin. Lipid-lowering drugs cannot be combined with the following medications:
- proteinase inhibitors;
- Fenofibrate, Gemfibrozil and other fibrates;
- Ezetimibe;
- Erythromycin;
- antacids;
- fusidic acid;
- Cyclosporine.
Women taking oral contraceptives containing norgestrel and ethinyl estradiol should closely monitor for possible side effects of the drug combination and report to the doctor if they occur.
No ads 3
Features of Atorvastatin
The drug Atorvastatin belongs to the category of third generation statins. The drug is available in various dosages - 10, 20, 40 and 80 mg. The pharmacy chain offers 2 types of this drug - Russian (Atorvastatin) and Israeli (Atorvastatin-Teva). The active ingredient in Atorvastatin is atorvastatin calcium trihydrate.
The drug reduces the concentration of low-density lipoproteins and simultaneously increases the content of high-density lipoproteins. Also effective for familial and homozygous hypercholesterolemia. The effectiveness of the medicine appears after 2 weeks of regular use. After just 30 days, the maximum effect of the anticholesterol drug is achieved, which persists throughout the entire duration of treatment.
Atorvastatin, like Rosuvastatin, belongs to a new generation of statins
Taking Atorvastatin must be combined with diet. According to the diet, the patient must exclude from the diet foods rich in animal fats, as well as dishes prepared by frying. You can take the tablets regardless of meal time. The dosage is selected individually by the attending physician based on the results of the lipid profile.
The initial dosage is 10 mg; subsequently, if necessary, it can be increased to 80 mg per day. Patients suffering from renal or liver failure take Atorvastatin at this initial dosage all the time. Indications for the use of Atorvastatin are the complex treatment of high levels of total cholesterol and LDL and increased levels of triglycerides.
The following side effects may occur while taking Atorvastatin:
- sleep disturbance;
- headache and dizziness;
- anemia or thrombocytopenia;
- dyspeptic disorders;
- arthritis and myalgia;
- allergy;
- swelling;
- baldness;
- increased sweating;
- sensitivity to light.
Atorvastatin is not prescribed for use in cases of increased activity of liver enzymes, renal failure, during pregnancy and lactation, in case of individual intolerance to the components of the drug, severe liver pathologies. The drug is also contraindicated in patients under 18 years of age.
The cost of the drug in pharmacies depends on the dosage and manufacturer and varies from 130 to 400 rubles. Its analogues are the drugs Atoris, Liprimar, Tulip.
Substitute drugs
In medical practice, it is customary to replace one drug with another with similar properties if for some reason there is no therapeutic effect or the patient simply has increased sensitivity to the drug. If it is necessary to select an analogue of Rosuvastin, a specialist may prescribe Roxera tablets.
There are practically no differences from Rosuvastatin, since both drugs are based on the same active substance. But we cannot miss the point that medicines from foreign manufacturers are of higher quality due to their repeated testing, proven effectiveness and safety. Many patients do not save money, but purchase foreign drugs on the advice of their attending physicians.
Which is better, Roxera or Atorvastatin? The second drug also belongs to the group of third-generation statins and is intended for the treatment of hypercholesterolemia, produced in dosages from 10 to 80 mg. Roxera belongs to the IV generation class, contains the optimal dosage of the active substance and is suitable for patients who were prescribed a statin drug for the first time.
The difference is that Atorvastatin cannot be mixed with food, but Roxera is taken regardless of meals. The second difference is the chemical effect on the body. Atorvastatin has a large dosage, which is why it is broken down by liver enzymes; the activity of the tablets depends on the condition of this organ.
Roxera rarely reacts with other drugs taken by the patient, thanks to its flexible dosage form. This leads to the conclusion that it is better not to replace them with Atorvastatin for a patient who has been prescribed rosuvastatin-based tablets.
Substitutes for Rosuvastatin
Rosuvastatin SZ is the same analogue of Rosuvastatin, the only difference is that the generic version of the original drug Crestor Rosuvastatin SZ is produced by a pharmaceutical company in Russia.
In the absence of drugs such as Rosuvastatin and Roxera in pharmacies, the doctor can successfully replace them with Crestor at a dosage of 5 mg or higher. The same can be said about Rosuvastatin VIAL tablets, a similar drug produced by VIAL. The difference between many synonyms of Rosuvastatin lies only in the manufacturer and price.
Rosuvastatin analogues
Level 4 ATX code matches:
Akorta
Atomax
Lipitor
Pravastatin
Simvastol
Owencore
Simgal
Tulip
Lovastatin
Liptonorm
Rozulip
Zokor
Rosart
Tevastor
Atorvastatin
Liprimar
Simvastatin
Atoris
Basilip
Rosecard
Analogues of this drug are the following drugs:
- Crestor
- Kleval
- Rosart
- Rosicore
- Roseystar
- Roxera
- Tevastor
However, you should choose one or another analogue only in consultation with a doctor.
Reviews
There are a lot of reviews from doctors about the drug Rosuvastatin, mostly they are all positive. Many experts prefer to prescribe the original drug based on the same active ingredient Crestor, although it is more expensive, but has proven quality and effect. Among the substitutes for regular Rosuvastatin, Roxera is also popular.
But according to general medical practice, the drug Rosuvastatin is in one of the first places among the group of statins, since it belongs to the IV generation of drugs, has a flexible dosing system and is well tolerated by most patients. Reviews from patients who took Rosuvastatin are also positive:
Angelina, 47 years old: My attending cardiologist prescribed Rosuvastatin and at the same time recommended me to keep a low-fat diet and exercise (my weight at that time exceeded 95 kg). Two months have passed, I take 10 mg tablets per day, the weight has dropped, and the latest blood results pleased my doctor and me. Cholesterol dropped to normal levels.
Nina, 54 years old: In general, I am satisfied with Rosuvastatin tablets, but sometimes I notice that my head starts to hurt after taking it. Especially when I take the medicine on an empty stomach. I have a hereditary form of hypercholesterolemia, so I have to take pills constantly. I regularly donate blood for testing, after prescribing Rosuvastatin (before that I took Atorvastatin), my cholesterol levels have decreased significantly.
Ivan, 41 years old: Due to my obesity (125 kg), my blood pressure began to fluctuate, I felt dizzy, and after a long walk I began to feel short of breath. It turned out that it was not just a matter of high body weight; the test result showed that I had high cholesterol. At the insistence of the doctor, I had to go on a diet and take Rosuvastatin tablets along with Dibikor, as he prescribed. I was afraid of side effects after reading the long instructions, but so far I have not noticed any ill health after taking Rosuvastatin. I will continue to take medicine and go on a diet, I want to reduce not only cholesterol, but also weight.
What is the difference
A comparison of the drugs Atorvastatin and Rosuvastatin revealed that, despite some similarities, they belong to statins of different generations. Rosuvastatin is the latest development, and Atorvastatin precedes it. The advantage of the latest generation is that the dosage of the drug can be reduced, since it is highly effective.
Lovastatin and its analogues
Unlike Atorvastatin, 90% of Rosuvastatin is excreted from the body through the digestive system, and 5% through urine. In addition, if we compare drugs with each other in terms of lowering low-density cholesterol, Atorvastatin is slightly inferior to Rosuvastatin.
The first reduces by a maximum of 54%, and the second by 63%. They also differ in their half-life. If for Atorvastatin this period of time takes from 15 to 30 hours, then for Rosuvastatin it takes 19 hours.
The newest generation drug has a higher bioavailability. This means that it is better absorbed by the body. But the difference between them is not so significant: Atorvastatin – 12% and Rosuvastatin – 20%.
What also makes these drugs different is the nature of their solubility. Thus, Rosuvastatin is a hydrophilic drug, and Atorvastatin is lipophilic. This means that Atorvastatin is fat soluble and Rosuvastatin is water soluble. If you have to make a choice between Atoris and Rosuvastatin, then you must keep in mind that Atoris is a type of Atorvastatin, so the similarities and differences will be approximately the same.
In terms of safety, both drugs under consideration are approximately the same. But, for example, in type 2 diabetes, preference should be given to Rosuvastatin, since it has less effect on carbohydrate metabolism.
If we compare these drugs by cost, then in general the price of Atorvastatin is significantly lower than the cost of Rosuvastatin. In this sense, the dosage of the drug and the number of tablets in the package are important. For example, 90 tablets of 20 mg of Atorvastatin will cost about 800 rubles, while for the same package of Rosuvastatin you will have to pay more than 1000 rubles.
Judging by the effectiveness of these drugs, practice shows that Rosuvastatin has a more pronounced effect compared to Atorvastatin. Their effectiveness is higher, and the potential for side effects is lower than that of first-generation statins, for example, Simvastatin.
Features of Rosuvastatin
Rosuvastatin is a lipid-lowering agent and is prescribed to normalize the level of triglycerides and phospholipids and lipoproteins in the blood. The main active ingredient is rosuvastatin. It is prescribed for the treatment and prevention of hypercholesterolemia, atherosclerosis and its complications, and vein thrombosis.
Rosuvastatin reduces high concentrations of low-density cholesterol, total cholesterol, triglycerides, and apoliprotein. At the same time, it helps to increase the level of high-density lipoproteins. While taking this drug, the atherogenicity index decreases. This effect indicates normalization of the lipid profile.
Indications for prescribing this drug are as follows:
- hereditary tendency to increase cholesterol;
- initial detection of high cholesterol levels in the blood;
- increased levels of triglycerides in the blood;
- prevention of complications of atherosclerosis, namely angina pectoris, hypertension, myocardial infarction and stroke in patients over 50 years of age.
Since Rosuvastatin is not metabolized in the liver, its effect on this organ is minimal. After 90% of the drug is excreted through the intestines with feces, the rest through the kidneys with urine. The drug is not prescribed to persons under 18 years of age, patients with lactose intolerance, women during pregnancy and breastfeeding.
It is contraindicated in patients at the acute stage of liver disease, patients with myopathy, and those with individual intolerance to the components of the drug. The combination of Rosuvastatin with Cyclosporine is unacceptable. During treatment with this statin, doctors recommend following an anti-cholesterol diet. When prescribing a drug in a dosage of more than 40 mg, the attending physician takes into account the absolute and relative indications for this.
Rosuvastatin lowers cholesterol levels better than all other similar drugs
Both drugs - Atorvastatin and Rosuvastatin - have good patient reviews. Since these medications have similar effects, they are interchangeable. But the choice of a particular one should be determined by the doctor in accordance with the diagnosis and individual characteristics.