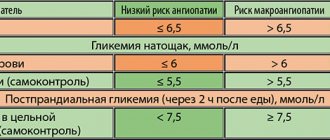
The modern view of the pathogenesis of type 2 diabetes mellitus (T2DM) is reflected in the term “ominous octet”: the classic pathogenetic triad (muscle and liver insulin resistance + progressive β-cell failure) is supplemented by 5 additional elements that contribute to formation and progression of the disease (impaired neuroendocrine interactions in the gastrointestinal tract; increased lipolysis in adipocytes; increased glucagon secretion; increased renal glucose reabsorption; insulin resistance of the central nervous system with the development of appetite regulation disorders) [1]. Therapy based on the incretin effect and represented by two classes of drugs - glucagon-like peptide 1 (GLP-1) receptor agonists and dipeptidyl peptidase-4 (DPP-4) inhibitors, due to its basic and pleiotropic effects, ideally fits into the modern concept of pathogenetically based therapy for T2DM with the influence and on additional and classical mechanisms of disease development. Current understanding of adequate glycemic control, based on analysis of the results of large clinical trials, focuses on reducing the risk of hypoglycemia and weight gain to reduce the likelihood of complications and mortality in diabetes [2]. It is this view that has brought DPP-4 inhibitors into the first line of treatment for T2DM. In the algorithms for specialized medical care for patients with diabetes (2011, issue 5), DPP-4 inhibitors are proposed as one of the classes of first-choice drugs in monotherapy for the initial stages of development of T2DM with a glycated hemoglobin (HbA1c) level of 6.5–7.5% [3] . In the Russian Federation today, three drugs of this group are registered for clinical use - sitagliptin, vildagliptin and saxagliptin. The differences between the currently available DPP-4 inhibitors are determined by the characteristics of metabolism (saxagliptin and vildagliptin are metabolized in the liver, unlike sitagliptin), excretion, recommended doses, and frequency of administration. However, the drugs are similar in effectiveness in terms of the degree of HbA1c reduction, safety profile and tolerability [4].
Sitagliptin: direct and pleiotropic effects
The first DPP-4 inhibitor, sitagliptin, was approved as a treatment for T2DM in 2006 [4]. To date, it remains the most studied representative of the gliptin class, a kind of standard for comparative assessment of the effects of drugs of this or another class of glucose-lowering drugs. An analysis of multiple clinical studies of sitagliptin lasting from 12 to 52 weeks demonstrates that the drug reduces HbA1c levels after 12 weeks of therapy by 0.65%, after 18–24 weeks by 0.84–0.85%, after 30 weeks by 1 .0% and after 52 weeks – by 0.67%. These results are slightly inferior to the effects of sulfonylurea drugs and are comparable to the effects of metformin and glitazones [5]. However, according to a 2-year comparative clinical study by T. Seck et al. (2010), with regard to the effect on HbA1c, sitagliptin demonstrated efficacy comparable to that of glipizide [6].
Sitagliptin is a selective daily action DPP-4 inhibitor, recommended for both mono- and combination therapy (together with metformin, sulfonylureas, glitazones, insulin) for a single dose. At the same time, the glycemic response to taking 100 mg of sitagliptin once and 50 mg twice does not differ [7], which fully justifies the use of a fixed combination of metformin/sitagliptin in a double dose regimen.
The membrane enzyme DPP-4 is expressed in many tissues (kidney, intestine, vascular endothelium, exocrine pancreas, gastrointestinal tract, biliary tract, thymus, lymph nodes, uterus, placenta, prostate gland, myocardium, brain, adrenal glands, mammary and salivary glands) and is involved in a wide range of metabolic processes [8]. DPP-4 is known to be found in seminal and cerebrospinal fluids. However, the function of DPP-4 has not been fully studied to date. The pleiotropic effects of DPP-4 inhibitors known today are determined by their influence on the activity of neuropeptides, gastrointestinal hormones, cytokines and chemokines, as well as their immunomodulatory effect [9]. The presence of pleiotropic effects has prompted interest in the clinical relevance of these drugs, primarily in the context of safety.
Sitagliptin is a safe and effective treatment for diabetes mellitus
Innovative methods of treating type 2 diabetes mellitus undoubtedly include incretin drugs, in particular dipeptidyl peptidase 4 inhibitors. The first representative of dipeptidyl peptidase 4 inhibitors was sitagliptin. Sitagliptin has pharmacokinetic characteristics unique for this class of drugs. Its effectiveness and safety in the form of mono- and combination therapy have been confirmed in a number of placebo-controlled studies.
Diabetes mellitus (DM) occupies a leading position among diseases leading to severe complications and death [1]. First of all, it is associated with high cardiovascular risk [1, 2]. Thus, in patients with diabetes, the likelihood of developing a stroke increases three times, myocardial infarction – five times. Diabetes mellitus worsens the course of diseases of the kidneys, peripheral vessels, and joints. In addition, it increases the risk of purulent complications.
Type 2 diabetes mellitus is a heterogeneous disease with many pathogenetic mechanisms. Its development can be determined both genetically and lifestyle, environmental factors, and stress.
Glucose homeostasis is known to be controlled by a number of mechanisms, most notably by pancreatic β cells. An equally important role in this process is played by the sensitivity to insulin of cells of peripheral tissues (liver, muscles, adipose tissue), as well as to glucagon of liver cells. It is no coincidence that β-cell dysfunction, insulin resistance, and hyperglucagonemia are recognized as the main pathogenetic links of type 2 diabetes. According to modern data, these include increased glucose absorption by the kidneys and insulin resistance of brain cells [3, 4].
Treatment methods for type 2 diabetes are based on data obtained from studying the mechanisms of hyperglycemia. It should be noted that currently some approaches to therapy are being revised taking into account their effect on complications of diabetes mellitus, β-cell function, and insulin resistance [5].
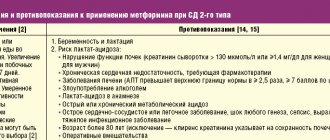
For a long period of time, only two classes of drugs were used to treat patients with type 2 diabetes: biguanides and sulfonylureas. All of them have a good hypoglycemic effect. However, over time, many patients require intensification of therapy due to the progression of diabetes, which in turn increases the risk of developing undesirable reactions, such as lactic acidosis and hypoglycemia.
In 2006, a new innovative class of glucose-lowering drugs appeared - dipeptidyl peptidase 4 (DPP-4) inhibitors.
DPP-4 is an enzyme that hydrolyzes incretins in the blood [5].
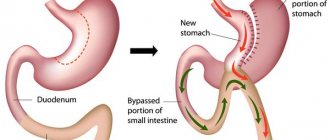
Hormones of the incretin family are synthesized by cells of the small intestine. The level of incretins in the blood increases in response to food intake.
According to the data obtained, incretins are part of the system for regulating glucose homeostasis. At normal or elevated blood glucose levels, they promote an increase in insulin synthesis by pancreatic β-cells through intracellular signaling mechanisms associated with cyclic adenosine monophosphate [6, 7]. Small intestinal hormones such as glucagon-like peptide 1 (GLP-1) and glucose-dependent insulinotropic polypeptide are primarily associated with the hypoglycemic effect. GLP-1 also helps suppress glucagon secretion by alpha cells of the islets of Langerhans. A decrease in glucagon concentration against the background of an increase in insulin levels leads to a decrease in glucose production by the liver. As a result, blood glucose levels decrease [8].
Dipeptidyl peptidase 4 is an enzyme that, by breaking down incretins in the blood, inactivates GLP-1. Inhibition of DPP-4 allows you to prolong the lifespan of GLP-1 and enhance its metabolic effects.
Thus, the mechanism of action of DPP-4 inhibitors is based on increasing the activity of incretins - GLP-1.
Sitagliptin is the first drug from the group of DPP-4 inhibitors (gliptins). Sitagliptin inhibits DPP-4 by 91.7% [8].
To date, sitagliptin is the most studied drug of the gliptin group. It has been used in clinical practice for more than ten years.
Therapy with DPP-4 inhibitors is characterized by an optimal balance of effectiveness and safety. In particular, DPP-4 inhibitors are associated with good tolerability, a low risk of hypoglycemic conditions, and a neutral effect on body weight.
The low risk of hypoglycemia is due to the peculiarities of the mechanism of action of DPP-4 inhibitors. As noted earlier, inhibition of DPP-4 increases the level of incretins in the blood. Incretins in turn stimulate β-cell function.
Stimulation of insulin secretion by drugs of this group is glucose-dependent in nature, that is, the higher the level of glucose in the blood, the higher the insulinemia. β-cell stimulation ceases when normoglycemia is achieved.
In numerous studies, sitagliptin has demonstrated effectiveness both as monotherapy and in combination with other oral hypoglycemic drugs.
In 2009, JA Davidson conducted a placebo-controlled, randomized trial of 530 patients with type 2 diabetes whose glycated hemoglobin (HbA1c) levels ranged from 7.5 to 11.0%. This study assessed the efficacy and safety of sitagliptin as monotherapy. After 12 weeks of treatment, HbA1c levels decreased on average by 0.65%, 18 weeks - by 0.84%, 24 weeks - by 0.85%, 30 weeks - by 1.0%, 52 weeks - by 0.67% [9]. In addition, there was a decrease in fasting and postprandial glycemia - on average by 1.7 and 3.1 mmol/l. During the treatment, there was no increase in body weight and no significant increase in the frequency of hypoglycemic conditions. At the end of the study, more patients in the sitagliptin group achieved target HbA1c values than in the placebo group.
N. Barzilai et al. studied the effectiveness and safety of sitagliptin in elderly patients with type 2 diabetes (mean age 72 years). According to the study results, sitagliptin reduced HbA1c by 0.7%. Moreover, the frequency of adverse reactions in the sitagliptin and placebo groups was comparable [10, 11].
The best results in achieving glycemic control and reducing side effects were obtained by combining sitagliptin and metformin.
M. A. Nauck et al. compared two combination therapy regimens: sitagliptin + metformin and glipizide + metformin. After 52 weeks, in both groups, HbA1c levels decreased by 0.67%, however, the number of patients who experienced at least one episode of hypoglycemia was several times higher in the glipizide group - 32 versus 5%, respectively (p
In a study conducted by SS Kim, the efficacy and safety of a fixed combination of sitagliptin and metformin were compared with the efficacy and safety of glimepiride. It randomized 292 patients with type 2 diabetes. After 30 weeks of treatment, the combination of sitagliptin and metformin was superior to glimepiride in reducing HbA1c levels - 1.49 versus 0.71%, respectively.
In those receiving combination therapy, the treatment goal was achieved in 82.2% of cases.
The study concluded that the use of a fixed combination of sitagliptin and metformin as initial therapy provides better glycemic control and better weight loss with a lower incidence of hypoglycemia [13].
In 2008, following the withdrawal of rosiglitazone from the pharmaceutical market due to evidence of adverse cardiovascular events associated with this therapy, the US Food and Drug Administration required drug manufacturers to conduct clinical studies of their long-term cardiovascular safety. At the same time, for glucose-lowering drugs it is necessary to evaluate the effect on macrovascular complications.
According to a meta-analysis of 70 randomized trials including almost 42,000 patients, treatment with DPP-4 inhibitors for more than 24 weeks led to a reduction in the risk of cardiovascular events, in particular myocardial infarction, and overall mortality in patients with type 2 diabetes [14]. In addition, a number of studies, in addition to a moderate glucose-lowering effect, noted the pleiotropic effect of DPP-4 inhibitors. In particular, the drugs had a positive effect on the lipid spectrum [15], blood pressure [16], endothelium of the vascular wall and myocardium. With the use of DPP-4 inhibitors, the reduction in the risk of myocardial infarction was more significant than with the modification of such known risk factors as HbA1c level, lipid profile, and blood pressure.
It should be emphasized that the meta-analysis included studies that examined DPP-4 inhibitors. Overall, all DPP-4 inhibitors demonstrated a high cardiovascular safety profile.
However, the SAVOR-TIMI 53 study reported an increased risk of adverse events such as hospitalization for heart failure [17].
In this regard, the results of the TECOS study are of particular interest [18]. This is a double-blind, randomized, placebo-controlled study to evaluate the cardiovascular safety of the DPP-4 inhibitor sitagliptin. It involved 14,671 patients with type 2 diabetes. Sitagliptin at a dose of 100 mg/day or placebo was added to the already ongoing diabetes therapy. The average duration of treatment was three years. The initial HbA1c level is from 6.5 to 8.0%. All patients suffered from cardiovascular diseases.
It should be noted that therapy was prescribed taking into account the glomerular filtration rate.
The primary composite cardiovascular endpoint was the time until the onset of a cardiovascular event—cardiovascular death, nonfatal myocardial infarction, nonfatal stroke, or hospitalization for a cardiovascular event. The incidence of these events in those taking sitagliptin and placebo was comparable - 11.4% (4.06/100 patient-years) and 11.6% (4.17/100 patient-years).
The groups also did not differ in time to secondary cardiovascular endpoint (nonfatal myocardial infarction, nonfatal stroke, or hospitalization for a cardiovascular event). The incidence of these events in the sitagliptin and placebo groups was 10.2% (3.58/100 patient-years) and 10.2% (3.62/100 patient-years), respectively.
In addition, sitagliptin therapy did not increase total or cardiovascular mortality.
In the TECOS study, the incidence of hospitalization for chronic heart failure in the sitagliptin and placebo groups was comparable.
Thus, the study once again demonstrated the hypoglycemic effect of sitagliptin, both as mono- and combination therapy [18, 19].
In conclusion, it should be noted that the creation of sitagliptin, as well as other drugs from the group of DPP-4 inhibitors, is a great achievement in the field of diabetology in recent years. Sitagliptin has an extensive evidence base and extensive clinical experience. Its advantages include a glucose-dependent mechanism of action, high efficiency and safety, the presence of pleiotropic effects, the possibility of use both as monotherapy and in combination with other glucose-lowering drugs. In addition, sitagliptin has no restrictions on its use in patients with liver and kidney pathologies. Therefore, it can deservedly take a leading position among drugs used for type 2 diabetes.
Side effects of sitagliptin: data from meta-analyses
Hypoglycemia
In monotherapy, DPP-4 inhibitors can provoke the development of hypoglycemia only in extremely rare cases, the risk of which is comparable to that when using placebo [10]. The risk increases with concomitant use of DPP-4 inhibitors and sulfonylureas or insulin; in these cases, the doses of the latter should be reduced [4, 11].
Effect on body weight (BW)
In clinical studies, sitagliptin demonstrated both a decrease in body weight by 1.5 kg and an increase by 1.8 kg [12]. The explanation for these facts lies in the versatility of the effects of DPP-4 blockade. DPP-4 inhibitors have many physiologically related substrates: in addition to the glucagon family (GIP, GLP-1), the pancreatic polypeptide family (neuropeptide Y and peptide YY), a wide range of cytokines (Mig, I-TAC, eotaxin, RANTES factor, expression and the secretion of which is regulated upon activation of normal T cells), substance P [12]. DPP-4 inhibitors moderately increase the level of the active form of GLP-1, which may cause a moderate decrease in BW in some cases. In addition, in patients with T2DM, it statistically significantly reduces the fasting level of ghrelin [13], produced mainly by endocrine cells of the stomach and involved in the regulation of eating behavior and intestinal motility [14]. This may also contribute to the decrease in BW.
On the other hand, the interaction of DPP-4 with neuropeptide Y, a potentially orexigenic substance, forms a truncated form of neuropeptide Y (3-36) with a corresponding change in affinity for the receptor - a mediator of the antilipolytic function of the peptide. Inhibition of DPP-4 may thus interfere with the effects of neuropeptide Y on appetite and body mass and alter its action in adipose tissue. This may explain the absence of a decrease in BW observed with DPP-4 [12].
Thus, the combined direct and pleiotropic effects of gliptins determine the neutral effect on MT confirmed by controlled clinical studies of DPP-4 inhibitors [4, 10].
It should be noted that the neutral effect of sitagliptin in relation to the level of calorie intake and BW can play an important positive role for the preservation of muscle mass and the protein component of the body in older patients, which may serve as an additional reason for choosing sitagliptin as a priority drug for them compared to agonists GLP-1 receptors [4].
Infections
The role of DPP-4 in regulating the immune response includes the induction of transforming growth factor β1, which is expressed by activated T lymphocytes, suppression of the production of inflammatory cytokines [15], and effects on cell growth, differentiation and apoptosis [16]. The immunomodulatory effect of DPP-4 has led to concern about a possible increased risk of infection when the enzyme is inhibited. The complexity of analyzing the relationship between infections and the use of DPP-4 inhibitors is determined by the known data on a possible direct relationship between diabetes and impaired functioning of the body’s immune system [17].
At the beginning of 2011, the results of an analysis of the incidence of infections while taking antihyperglycemic drugs were published, based on the WHO database (VigiBase, the World Health Organization-Adverse Drug Reactions [WHO-ADR] database) for 1999–2009. The study showed a twofold increase in the incidence of mild infections, mainly of the upper respiratory tract, with the use of DPP-4 inhibitors compared with biguanides. There was no increased risk of more serious infections. However, this analysis has limitations, which the authors themselves point out, concluding that further research is necessary [18]. To date, it can be assumed that taking DPP-4 inhibitors is not associated with any serious human disease [12].
Pancreatitis
Pancreatitis, including fatal and non-fatal, hemorrhagic or necrotizing, has been reported in some patients taking sitagliptin and linagliptin [11]. During post-marketing surveillance from October 2006 to February 2009, 88 cases of acute pancreatitis were reported in patients taking sitagliptin or sitagliptin + metformin, and in 19 cases pancreatitis developed in the first 30 days of therapy [4].
The difficulty of analyzing the relationship between the use of DPP-4 inhibitors and the development of pancreatitis lies in the presence of other risk factors for the occurrence of this pathology, including hypercholesterolemia, hypertriglyceridemia, obesity and diabetes itself [19].
Based on the results of an analysis of 45 clinical studies, 5 pharmacokinetic studies and 28 meta-analyses with observation periods ranging from 7 days to 104 weeks, KR Richard et al. (2011) concluded that the incidence of pancreatitis while taking sitagliptin was significantly lower than with other oral hypoglycemic drugs [10]. However, it is recommended that patients be informed of the symptoms of pancreatitis and advised to discontinue the drug if they occur.
Sitagliptin in mono- and combination therapy with Metformin
For citation. Mkrtumyan A.M., Egshatyan L.V. Sitagliptin in mono- and combination therapy with metformin // Breast Cancer. 2015. No. 27. pp. 1653–1656.
Introduction
The epidemic nature of the increase in the number of patients with type 2 diabetes mellitus (DM) among the population of developing and highly developed industrial countries leads to the emergence of many serious problems in the healthcare system. The growth of the population of patients with diabetes and the frequency of its chronic complications is one of the most pressing problems facing the world community today. It is no secret that diabetes, being, as many put it, “not a disease, but a way of life,” is in fact the cause of many human tragedies. Type 2 diabetes is a severe and progressive disease with a risk equivalent to that of cardiovascular disease (CVD), requiring continuous use of glucose-lowering drugs and intensified therapy. It can be clearly stated that the diabetes SAGA is very tragic: • Blindness: one in five people are blind in the world. • Limb amputation: every seventh amputee in the world (non-traumatic cause). • Hemodialysis: every third in the world. • CABG and stenting: every fifth in the world. When a diagnosis of type 2 diabetes is made, active lifestyle changes and metformin therapy are the first basic measures. However, if monotherapy is insufficient, there is a need for combination therapy to achieve the goal of reducing and maintaining glycemia [1]. In addition to metformin and lifestyle modifications, several groups of drugs are approved. However, it must be recognized that the proposed treatment model for type 2 diabetes is not always effective and has side effects [2]. Sulfonylureas (SUs) cause a risk of hypoglycemia and increase body weight; Thiazolidinediones also increase body weight, retain fluid, and are associated with a risk of congestive heart failure and fractures; side effects of alpha-glucosidase inhibitors include bloating, discomfort, excess gas in the intestines and diarrhea [2]. Therefore, the priority when choosing a drug that should be added to a patient with unsatisfactory compensation of type 2 diabetes during metformin monotherapy (or prescribed as the first drug if it is impossible to take metformin) remains open. One thing is clear: the choice should be given to drugs with minimal side effects. With a number of advantages (increased glucose-dependent β-cell activity, low risk of hypoglycemia, suppression of increased glucagon secretion, ability to control body weight), glucagon-like peptide-1 (GLP-1) receptor agonists and dipeptidyl peptidase-4 (DPP-4) inhibitors have taken their rightful place in hypoglycemic therapy of type 2 diabetes [3, 4]. DDP-4 inhibitors have been shown to be superior to traditional oral hypoglycemic agents in terms of efficacy and tolerability [5–8]. The algorithm of the American Association of Clinical Endocrinologists and the American College of Endocrinologists for the first time classifies incretins as first-line drugs in cases where there is a high risk of hypoglycemia [2]. In 2011, a group of experts from the Russian Association of Endocrinologists determined the possibility of using drugs from the group of DPP-4 inhibitors and GLP-1 inhibitors in the onset of type 2 diabetes as monotherapy or as part of combination therapy with other glucose-lowering drugs, depending on the initial level of glycated hemoglobin (HbA1c ) [9]. Thus, due to the optimal combination of effectiveness and safety, DPP-4, along with metformin, are included in national and international recommendations as drugs for starting therapy for type 2 diabetes. DPP-4 inhibitors are also 2nd and 3rd line drugs if not previously prescribed, as well as in elderly patients. The advantages of using DPP-4 inhibitors in elderly patients include a single dose, safety in case of decreased renal function, and a low risk of hypoglycemia. According to recommendations for the management of patients with type 2 diabetes, the joint prescription of glucose-lowering drugs of different groups with complementary mechanisms of action is justified. Due to the effect on insulin resistance and β-cell dysfunction, the absence of the risk of weight gain and the development of hypoglycemia, combination therapy with DPP-4 inhibitors and metformin is considered the most rational. The combination of DPP-4 inhibitors and metformin provides an additional hypoglycemic effect compared to monotherapy and does not increase the side effects of metformin on the gastrointestinal tract. This combination may be able to delay the administration of SM derivatives and the start of insulin therapy. This article discusses the use of the DPP-4 inhibitor sitagliptin and its combination with metformin, which improves disease outcomes.
Dipeptidyl peptidase-4 inhibitors
GLP-1 occupies a central place among incretins in maintaining normal carbohydrate metabolism. Its beneficial effects include improved β-cell function, glucose-dependent insulin secretion, suppression of glucagon production, including extrapancreatic properties such as slowing gastric emptying and suppressing appetite [10]. GLP-1 does not exert its effects for long due to rapid dehydration and loss of insulinotropic effect under the influence of the serine protease, DPP-4. Understanding the role of DPP-4 served as the basis for the creation of a new group of drugs – its inhibitors with the aim of increasing the duration of action of GLP-1 [11]. DPP-4 inhibitors exist in oral form, they are reversibly and to a small extent bound to plasma proteins (38% for sitagliptin, 10% for vildagliptin, insignificant for saxagliptin), which determines the predominantly renal route of their elimination. The maximum concentration of the drugs is achieved in less than 4 hours. Sitagliptin and vildagliptin have high bioavailability (~85-87%), it is slightly lower for saxagliptin (~67%) [12, 13]. A randomized, open-label study examined the efficacy and safety of DPP-4 inhibitors (saxagliptin 5 mg and sitagliptin 100 mg once daily, vildagliptin 50 mg twice daily) in decompensated patients with type 2 diabetes with an HbA1c level of 7.5– 10% treated with metformin and another antihyperglycemic drug (glimepiride, acarbose or pioglitazone). At the end of the study, there was a decrease in HbA1c, fasting and postprandial blood glucose levels in all groups (saxagliptin vs vildagliptin vs sitagliptin: HbA1c: -1.2 vs -1.3 vs -1.1%; fasting blood glucose: -1.8 vs - 2.4 vs -1.5 mmol/l; postprandial glycemia: -3.4 vs -3.7 vs -3.2 mmol/l). The difference in the reduction in HbA1c and postprandial glycemia levels between the groups was not significant. The proportion of patients achieving target HbA1c <7% was similar between groups (saxagliptin 59%, vildagliptin 65%, sitagliptin 59%). Mild hypoglycemia was observed in all groups (saxagliptin - 6%, vildagliptin - 2%, sitagliptin - 3%). There were no significant differences in adverse events among the groups. Thus, gliptins have been shown to have similar glycemic control and incidence of side effects [14].
Sitagliptin
DPP-4 inhibitors have proven glycemic control activity and do not cause severe side effects or deplete pancreatic reserves. Research on the effects of DPP-4 inhibitors in preventing loss of β-cell function is encouraging. Saxagliptin and sitagliptin were experimentally shown to have similar improvements in glycemic control and β-cell mass in mice on a high-fat diet following streptozotocin administration [15]. Such properties help to use it most effectively in patients with newly diagnosed type 2 diabetes. In a 12-week study that examined the hypoglycemic effect of sitagliptin, use of the drug at a dose of 100 mg 1 time / day led to a decrease in HbA1c levels by an average of 0.6% compared with the placebo group (p < 0.001) [16]. The observed difference was greater the higher the initial HbA1c level. With an initial HbA1c level of less than 7%, the reduction was -0.4%, with a level of 7–8.5% – -0.6%, and with an HbA1c level of 8.5–10% – -0.8%. In recent years, the results of some studies using drugs often used in patients with diabetes (glycemic, lipid-lowering, weight-reducing) have received resonance due to the unexpected detection of undesirable effects, including CVD. This necessitates a balanced assessment of the safety of new drugs, especially their potential cardiovascular risk. The rosiglitazone story in 2007 led to the FDA introducing unprecedented new evidence requirements for the safety of hypoglycemic agents. The safety of sitagliptin in patients with type 2 diabetes in relation to the risk of developing CVD is very important, since the presence of type 2 diabetes is already an independent risk factor for CVD. Data on the cardioprotective properties of DPP-4 inhibitors in general and sitagliptin in particular were obtained from a retrospective analysis of the Danish register (2007–2011), which included 40,028 patients with type 2 diabetes without previous myocardial infarction (MI) and stroke [17]. Patients received metformin with drugs SU, DPP-4 inhibitors, GLP-1 inhibitors or insulin. There was a decrease in the proportion of patients receiving the combination of metformin + SM, and an increase in the proportion of patients receiving sitagliptin + metformin (up to 61.9%). With the latter combination, the hazard ratio (HR) for overall mortality decreased by 35%, cardiovascular mortality by 43%, and combined endpoints (MI, stroke, cardiovascular events) by 30%. The innovative research poster session at the 75 Scientific Readings of the American Diabetes Association in 2015 demonstrated the results of a retrospective study assessing the risk of hospitalization for heart failure (HF) when using DPP-4 inhibitors with SM drugs, based on data obtained in real-world clinical practice in patients with and without a history of CVD [18]. When comparing DPP-4 inhibitors and SM drugs in patients with a history of CVD, the RR was 0.95: 95% confidence interval (CI): 0.78, 1.15; in patients without CVD – RR 0.59: 95% CI: 0.38, 0.89. In conclusion, this study demonstrates that there is no increased risk of hospitalization due to HF or other cardiovascular events in patients with type 2 diabetes treated with DPP-4 inhibitors compared with SM, as well as in patients in the DPP-4 inhibitor subgroups. TECOS (Trial Evaluating Cardiovascular Outcomes with Sitagliptin) is a large, multicenter, placebo-controlled, double-blind, randomized, parallel-group study evaluating cardiovascular outcomes in 14,671 patients with type 2 diabetes treated with sitagliptin 100 mg/day compared with placebo when added to treatment for more than 3 months. antidiabetic therapy (oral hypoglycemic drugs ± insulin). The median duration of therapy was 3 years [19]. The primary composite endpoint was time to cardiovascular death, nonfatal MI and stroke, and hospitalization for unstable angina. Secondary composite endpoints - time to primary event included in the primary endpoint, first fatal or non-fatal MI, first fatal or non-fatal stroke, death from all causes, hospitalization for HF or cardiovascular death, changes in HbA1c levels, change in function kidneys, in patients who did not receive insulin initially, the time until the start of continuous insulin therapy, in all patients, the time until the start of the next additional drug, seeking medical care (for example, hospitalization, outpatient visit). Analysis of the primary composite endpoint demonstrated identical indicators in both groups (Fig. 1). Thus, the frequency of hospitalizations for unstable angina in the sitagliptin group was 1.5% of cases, in the placebo group – 1.6%. Overall, components of the primary endpoint were recorded in 11.4% of patients in the sitagliptin group and in 11.6% of patients in the placebo group. The RR was 0.98, 95% CI 0.88–1.09.
In summary, sitagliptin was neither inferior nor superior to placebo when analyzing the primary composite endpoint. A similar result was obtained for the secondary composite endpoint (Fig. 2).
The study also demonstrated that the incidence of severe hypoglycemia did not differ between the sitagliptin and placebo treatment groups. The benefit of sitagliptin as a hypoglycemic drug was confirmed by the more frequent initiation of insulin therapy, as well as a higher need for additional glucose-lowering drug in the placebo group compared with the sitagliptin group. In contrast to the SAVOR-Timi study (saxagliptin), where a significant increase in the indicator “hospitalization due to HF” was noted (by 27%) [20], and the EXAMINE study (alogliptin), where a non-significant increase in this indicator was noted (by 19%) [21 ], in the TECOS study, the incidence of hospitalization for HF did not differ between the sitagliptin and placebo groups. Based on the results of the TECOS study, it can be stated that sitagliptin therapy is not inferior to standard glucose-lowering therapy and is not superior to it. The addition of sitagliptin to glucose-lowering therapy appeared to be safe with respect to the risk of developing a new cardiovascular event.
Combination of sitagliptin and metformin
Metformin is the most frequently prescribed drug at the onset of type 2 diabetes, and later in combination with various glucose-lowering drugs. Metformin therapy, in addition to its effect on plasma glucose levels, has many other – so-called pleiotropic – effects on the body of a patient with type 2 diabetes. In addition to the well-known effects of metformin, it has been found that it can help increase the concentration of circulating GLP-1 in the blood, improving glycemic control [22, 23]. DPP-4 inhibitors are an ideal partner for metformin. One of the most interesting options for using DPP-4 inhibitors in combination with metformin is the initial treatment of type 2 diabetes, since titrating the dose of DPP-4 inhibitors is easy, and they do not have additional adverse effects when combined with metformin. This combination is aimed at achieving target glycemic values and, possibly, can delay the prescription of SM derivatives and the start of insulin therapy. It was shown that the addition of 100 mg sitagliptin to metformin therapy in patients with poor glycemic control (HbA1c 7–10%) led to a significant decrease in HbA1c levels (–0.7% compared with placebo, p < 0.001) [24]. Taking into account the pharmacodynamics of metformin, the combination is prescribed 2 times a day, which allows maintaining stable inhibition of DPP-4. According to a retrospective analysis of a US medical records database, starting combination therapy allows one to maintain the achieved glucose-lowering effect for more than six months compared to starting with metformin monotherapy [25]. Another study demonstrated that the effect of combination therapy including sitagliptin with metformin and the effect of the drug SM (glimepiride) with metformin are comparable. The target HbA1c <7% was achieved in 63 and 59% of patients, respectively. At the same time, the combination of sitagliptin + metformin contributed to a reduction in body weight by 2.3 kg and the frequency of hypoglycemia episodes by 6 times (compared to the combination of SM + metformin) [26]. In summary, the results of these studies show a clinically and statistically significant improvement in HbA1c levels with the combination of sitagliptin and metformin in patients with type 2 diabetes.
Conclusion
Since their introduction, DPP-4 inhibitors have managed to take a strong place among drugs for the treatment of type 2 diabetes. Additional advantages of this class of drugs: low risk of hypoglycemia, no effect on body weight and no side effects from the gastrointestinal tract. The results of the TECOS study confirm the cardiovascular safety profile of sitagliptin in patients at high risk of cardiovascular complications - there are no statistically significant differences in the incidence of combined cardiovascular events compared with conventional treatment. There was also no increase in hospitalizations for HF compared with placebo. The presented data from numerous studies have shown that sitagliptin in mono- and combination therapy improves glycemic control, reduces the need for insulin, and the risk of cardiovascular complications.
Sitagliptin and β-cells
In vitro studies on experimental models have shown the potential ability of incretins to increase β-cell mass by increasing the expression of key transcription factors, stimulating neogenesis and β-cell proliferation, differentiating β-cells from progenitor cells, and inhibiting apoptosis [20]. Data from clinical studies in this regard also look encouraging.
According to a meta-analysis of randomized clinical trials, sitagliptin is superior to placebo in its effect on the HOMA-β index (12.03% increase) and the proinsulin/insulin ratio [21]. Recently published results from a prospective, randomized, placebo-controlled trial showed that sitagliptin monotherapy, as well as the sitagliptin + metformin combination, improved β-cell function with maintenance of this effect over 2 years of follow-up [22].
Use of sitagliptin at various stages of T2DM
DPP-4 inhibitors are the first choice drugs in the treatment of T2DM in the early stages of the disease. At the same time, according to some data, increased degradation of GLP-1 is not significant in the pathogenesis of T2DM at the onset of its development [23]. The results of a double-blind, placebo-controlled study of the use of sitagliptin in patients with impaired fasting glycemia demonstrated the absence of a significant effect of DPP-4 inhibitors on fasting and postprandial blood glucose levels, which supports this hypothesis [24].
According to experimental data, chronic hyperglycemia significantly increases DPP-4 activity and mRNA expression in human glomerular endothelial cells in vitro [23]. Clinical studies have shown that in patients with T2DM and HbA1c levels > 8.5%, DPP-4 activity is significantly higher than in patients with newly diagnosed diabetes or impaired glucose tolerance. A significant positive correlation has been established between the level of HbA1c and the activity of DPP-4 in microvascular endothelial cells - the most important pool of this enzyme, which plays a major role in the pathogenesis of diabetes: with poor metabolic control, chronic hyperglycemia induces a significant increase in the activity of DPP-4 in patients with T2DM, which reduces the level of circulating active GLP-1 and maintains postprandial hyperglycemia [25].
Thus, the use of sitagliptin in the later stages of T2DM seems more than justified from the point of view of its pathogenesis. The results of clinical observations suggest that starting therapy with sitagliptin in T2DM may provide additional benefit even in the event of an absolute requirement for insulin [26]. According to a prospective placebo-controlled study in a group of patients with T2DM with a disease duration of more than 10 years, the addition of sitagliptin to insulin therapy at a constant dose (long-acting insulin, intermediate-acting insulin, or mixed insulin) with inadequate glycemic control during 24 weeks of observation provided improvement in glycemic control with good tolerability and lack of weight gain [27].
Sitagliptin
International name of the medicinal substance:
Sitagliptin (Staglyptine) The list of drugs containing the active substance Sitagliptin is given after the description.
Pharmacological action:
Selective inhibitor of the enzyme dipeptidyl peptidase 4 (DPP-4).
In chemical structure and pharmacological action it differs from other hypoglycemic drugs. By inhibiting DPP-4, sitagliptin increases the concentration of hormones of the incretin family: GLP-1 and glucose-dependent insulinotropic peptide (GIP), which are part of the internal system for regulating glucose homeostasis. Incretins are secreted in the intestine and their concentration increases in response to food intake. At normal or elevated blood glucose concentrations, incretins enhance insulin synthesis, as well as its secretion by beta cells of the pancreas due to intracellular signaling mechanisms associated with cyclic AMP. GLP-1 suppresses increased secretion of glucagon by alpha cells of the pancreas. A decrease in glucagon against the background of an increase in insulin concentration helps to reduce the production of glucose by the liver, which ultimately leads to a decrease in glycemia. Incretins do not affect insulin synthesis and glucagon secretion in response to hypoglycemia. Under physiological conditions, the DPP-4 enzyme hydrolyzes incretins to form inactive products. Sitagliptin, by inhibiting the DPP-4 enzyme, suppresses the hydrolysis of incretins, increasing the concentrations of active forms of GLP-1 and GIP, increases insulin release and reduces glucagon secretion. In type 2 diabetes mellitus with hyperglycemia, these changes lead to a decrease in the concentration of glycosylated Hb and a decrease in plasma glucose concentration determined on an empty stomach and after an exercise test. Taking one dose inhibits the activity of the DPP-4 enzyme for 24 hours and increases the concentration of circulating incretins by 2-3 times. Pharmacokinetics:
Absorbed quickly, regardless of food intake (fatty foods do not affect pharmacokinetics). Absolute bioavailability - 87%. Cmax - 950 nmol, TCmax - 1-4 hours. AUC is dose-dependent - 8.52 µmol x h (at a dose of 100 mg), has low variability between patients. When steady state is reached, repeat doses of 100 mg increase AUC by 14%. The volume of distribution is 198 l (after taking a single dose of 100 mg). Protein binding - 38%. A small part of the drug is metabolized; the enzymes CYP3A4 and CYP2C8 are involved in the process. 6 metabolites were discovered that do not have DPP-4 inhibitory activity. Renal clearance - 350 ml/min. Sitagliptin is a substrate for the human organic anion transporter type 3 and p-glycoprotein, which may be involved in the process of drug excretion by the kidneys. T1/2 - 12.4 hours. Excreted within 1 week after taking the drug: by the intestines (13%), by the kidneys by tubular secretion (79% - unchanged, 16% - in the form of metabolites). In patients with chronic renal failure with CC - 50-80 ml/min, the concentration of sitagliptin in plasma does not change. When CC is 30-50 ml/min, there is a 2-fold increase in AUC compared to the control group. With CC less than 30 ml/min, as well as in patients with end-stage chronic renal failure, a 4-fold increase in AUC is observed. In patients with CC - 30-50 ml/min and CC less than 30 ml/min, dose adjustment is required to achieve a therapeutic concentration of the drug. With liver failure of 7-9 points on the Child-Pug scale, AUC and Cmax increase by 21% and 13%, respectively (when taking 100 mg of the drug). With liver failure of more than 9 points on the Child-Pug scale, there is no significant change in pharmacokinetics, because the drug is primarily excreted by the kidneys. In patients 65-80 years old, the concentration of sitagliptin is 19% higher (clinically not significant).
Indications:
Type 2 diabetes mellitus: as monotherapy (as an addition to diet and exercise) or as part of combination therapy with metformin or the peroxis proliferator agonist thiazolidinedione.
Contraindications:
Hypersensitivity, type 1 diabetes mellitus, diabetic ketoacidosis, pregnancy, lactation, childhood and adolescence (up to 18 years).
Side effects:
From the digestive system: abdominal pain, nausea, vomiting, diarrhea.
Laboratory indicators: hyperuricemia, decreased activity of the total and partially bone fraction of alkaline phosphatase, leukocytosis due to an increase in the number of neutrophils. Other (a cause-and-effect relationship with the drug has not been established): upper respiratory tract infections, nasopharyngitis, headache, arthralgia. The incidence of hypoglycemia is similar to that observed with placebo. Interaction:
There was a slight increase in the AUC (by 11%), as well as the average Cmax (by 18%) of digoxin when used with sitagliptin, which does not require dose adjustment.
Cyclosporine (a potent inhibitor of p-glycoprotein) increases the AUC and Cmax of sitagliptin by 29% and 68%, respectively, when used together with 100 mg of sitagliptin and 600 mg of cyclosporine (orally), which does not require dose adjustment (including when used with other drugs). p-glycoprotein inhibitor ketoconazole). Preparations containing the active substance Sitagliptin:
Xelevia, Januvia, Yasitara
The information provided in this section is intended for medical and pharmaceutical professionals and should not be used for self-medication. The information is provided for informational purposes only and cannot be considered official.
Sitagliptin for T1DM
To date, the theoretical justification for the use of gliptins in patients with type 1 diabetes (T1DM) is the effect of preserving and even increasing β-cell mass, which has been demonstrated so far only in vitro, which may be important in the early stages of development of T1DM or its preclinical stage as an addition to measures modeling or inhibiting the autoimmune process. According to E. Bosi (2010), the argument in favor of the use of DPP-4 inhibitors in T1DM may be, in particular, the ability to regenerate islet tissue that persists for quite a long time after the onset of the disease [28]. Perhaps a more significant prerequisite for the use of these drugs in T1DM is the modulating effect of DPP-4 on the subpopulation of T lymphocytes involved in the autoimmune process. CD26-membrane-associated glycoprotein (cluster of differentiation) with DPP-4 activity, expressed on lymphocytes, is involved in the regulation of the development, maturation and migration of T-lymphocytes, production of cytokines and antibodies [29]. Inhibition of the surface enzyme DPP-4 suppresses the proliferation of T lymphocytes, the production of Th1, and increases the secretion of the stimulator of cell differentiation - transforming growth factor β1 [30].
Sitagliptin modulates the migration of splenic CD4+ cells, which is associated with suppression of the direct effect of DPP-4 on T lymphocytes to a greater extent than with an increase in the level of incretin activity [31]. The latter mechanism, however, is also possible, since GLP-1 receptors are expressed by lymphoid tissue [32]. The experiment demonstrated that in vivo, sitagliptin reduces the migration of CD4+ cells from the lymph nodes and spleen due to both incretin-dependent and incretin-independent effects [33].
The experiment also showed that DPP-4 inhibitors are able to prevent the development of T1DM by suppressing the development of insulitis, modulating T-lymphocyte function and stimulating β-cell replication [34]. Theoretically, candidates for gliptin therapy are patients with newly diagnosed T1DM and patients at its various preclinical stages. Currently, enrollment of T1DM patients in a phase II clinical trial is ongoing, in which it is planned to evaluate the ability of diamide (GAD specific immunomodulator), lansoprazole (proton pump inhibitor) and sitagliptin to form antigen-specific tolerance and induce β-cell regeneration [35].
Sitagliptin and post-transplant diabetes
The incidence of diabetes after solid organ transplantation, according to various sources, varies from 2 to 53% [36]. Transplant-associated hyperglycemia (HAH) is a comorbid condition associated with the development of graft failure (up to 63% of cases), increased cardiovascular risks in recipients, and increased risk of death (up to 87%). In addition, with the development of HAT, the recipient may experience microvascular complications associated with diabetes. In this regard, effective management of hyperglycemia is fundamental to optimizing the management of patients after organ transplantation [36].
Drug therapy for transplant-associated diabetes includes, in addition to insulin, other hypoglycemic agents, based on the general principles of their selection. Taking into account the need for recipients to take immunosuppressants, which have known side effects, the problem of tolerability of any drug therapy is especially acute. In this regard, gliptins stand out from a number of hypoglycemic agents due to their excellent tolerability and ease of use. According to recent observations, the use of sitagliptin in diabetes after liver and kidney transplantation is effective and safe with respect to the development of hypoglycemia [37, 38].
Sitagliptin and cardioprotection
GLP-1 receptors are widely distributed in islet cells, kidneys, lungs, brain, gastrointestinal tract and heart [39]. Experimental models have demonstrated that GLP-1 infusion increases myocardial glucose uptake, improves left ventricular contractility in dogs with heart failure (HF), protects against ischemic myocardial stunning [40, 41], and limits the infarct area [42]. In an experiment modeling HF, sitagliptin helped maintain the level of glomerular filtration, modulated stroke volume and heart rate, and potentiated the positive inotropic effect of brain natriuretic peptide without increasing the energy needs of the myocardium [43].
Data from recent studies suggest a cardioprotective effect of gliptins in humans. In particular, the administration of sitagliptin at a dose of 100 mg/day to patients with coronary artery disease and preserved left ventricular function in a small prospective study improved the LV myocardial response to stress, attenuated post-ischemic stunning, and improved global and regional left ventricular contractility compared with placebo [44]. .
The results of the use of sitagliptin in combination with the mobilization of stem cells under the influence of granulocyte colony-stimulating factor in myocardial infarction look encouraging. When used, such therapy had a positive effect on myocardial regeneration and was safe, which may open up new prospects for the use of sitagliptin [45].
Several clinical studies have demonstrated the effect of DPP-4 inhibitors on blood pressure. In a group of 19 patients with mild to moderate hypertension without diabetes who received chronic antihypertensive therapy, taking sitagliptin for 5 days significantly reduced systolic and diastolic blood pressure compared with placebo (p < 0.05) [46]. However, most clinical studies demonstrate the absence of a significant effect of the drug on blood pressure [12].
Trulicity solution 1.5 mg/0.5 ml syringe pen 4 pcs ➤ instructions for use
Security Profile Overview
The safety of dulaglutide was studied during initial phase II and III clinical studies, where patients received dulaglutide alone or in combination with other hypoglycemic drugs. The most common adverse reactions (ADRs) in clinical studies were gastrointestinal reactions, including nausea, vomiting and diarrhea. In general, these reactions were mild to moderate and temporary in nature. The results of the long-term cardiovascular outcome study were similar.
ADRs identified during the assessment of the results of clinical trials of phases II and III, a long-term study of cardiovascular outcomes and post-registration experience of use are distributed according to systemic classes indicating the frequency of their occurrence according to WHO recommendations: very often: ≥1/10; often: ≥1/100 - <1/10; uncommon: ≥1/1000 - <1/100; rare: ≥1/10000 - <1/1000; very rare: <1/10000; frequency unknown (cannot be determined from available data).
Immune system disorders: uncommon – hypersensitivity, rare – anaphylactic reaction#;
Metabolic and nutritional disorders: very often - hypoglycemia* when used in combination with insulin, glimepiride, metformin† or metformin and glimepiride; often – hypoglycemia* when used as monotherapy or in combination with metformin and pioglitazone; uncommon – dehydration;
Gastrointestinal disorders: very common - nausea, diarrhea, vomiting†, abdominal pain†; often - loss of appetite, dyspepsia, constipation, flatulence, bloating, gastroesophageal reflux disease, belching; rarely – acute pancreatitis; with unknown frequency - non-mechanical intestinal obstruction;
Disorders of the liver and biliary tract: infrequently - cholelithiasis, cholecystitis;
Disorders of the skin and subcutaneous tissue: rarely - angioedema;
General disorders and disorders at the injection site: often - weakness; uncommon – reactions at the injection site;
Laboratory and instrumental data: often - sinus tachycardia, first degree atrioventricular block.
# Post-registration experience of use
* Documented symptomatic hypoglycemia with blood glucose concentration ≤3.9 mmol/L.
†For dulaglutide 1.5 mg only. The incidence of adverse reactions for dulaglutide 0.75 mg is in the lower category.
Description of individual HP
Hypoglycemia
When using dulaglutide in doses of 0.75 mg and 1.5 mg once a week as monotherapy or in combination with metformin or metformin and pioglitazone, the frequency of documented symptomatic hypoglycemia ranged from 5.9% to 10.9%, or from 0. 14 to 0.62 events/patient/year, no cases of severe hypoglycemia were observed.
When using dulaglutide in doses of 0.75 mg and 1.5 mg once a week in combination with a sulfonylurea derivative and metformin, the frequency of documented symptomatic hypoglycemia was 39.0% and 40.3%, respectively, or 1.67 and 1.67 events/patient/year, respectively. The incidence of severe hypoglycemia events was 0% and 0.7%, or 0.00 and 0.01 events/patient/year, for each dose, respectively. The incidence of documented cases of symptomatic hypoglycemia when using dulaglutide 1.5 mg with a sulfonylurea was 11.3% and 0.90 episodes/patient/year. There were no cases of severe hypoglycemia.
The incidence of documented cases of symptomatic hypoglycemia when using dulaglutide 1.5 mg with insulin glargine was 35.3% and 3.38 episodes/patient/year. The incidence of severe hypoglycemia was 0.7% and 0.01 episodes/patient/year.
When using dulaglutide in doses of 0.75 mg and 1.5 mg once a week in combination with prandial insulin, the incidence of hypoglycemia was 85.3% and 80.0%, or 35.66 and 31.06 events/patient/year. respectively. The incidence of severe hypoglycemia events was 2.4% and 3.4%, or 0.05 and 0.06 events/patient/year, respectively.
Adverse reactions from the gastrointestinal tract
Cumulative reporting of GI events up to 104 weeks with dulaglutide 0.75 mg and 1.5 mg once weekly, respectively, included nausea (12.9% and 21.2%), diarrhea ( 10.7% and 13.7%) and vomiting (6.9% and 11.5%). They were usually mild or moderate in severity, peaking in frequency during the first 2 weeks of therapy and decreasing rapidly over the next 4 weeks, after which the frequency remained relatively constant.
In clinical pharmacological studies that were conducted in patients with T2DM and lasted up to 6 weeks, most gastrointestinal events were observed within the first 2-3 days after taking the first dose, their frequency decreased with subsequent doses.
Acute pancreatitis
The incidence of acute pancreatitis in phase II and III clinical trials was 0.07% with dulaglutide compared with 0.14% with placebo and 0.19% with comparators, with or without additional baseline hypoglycemic therapy.
Pancreatic enzymes
When using dulaglutide, the average increase in the activity of pancreatic enzymes (lipase and/or pancreatic amylase) is 11-21% compared to baseline values. In the absence of other signs and symptoms of acute pancreatitis, elevated pancreatic enzymes are not predictive of the development of acute pancreatitis.
Increased heart rate
When using dulaglutide in doses of 0.75 mg and 1.5 mg once a week, a small average increase in heart rate of 2-4 beats per minute (bpm) was observed, with the incidence of sinus tachycardia with an increase in heart rate compared with a baseline rate of ≥15 beats/min was 1.3% and 1.4%, respectively.
First degree atrioventricular block/increased PR interval
When using dulaglutide in doses of 0.75 mg and 1.5 mg once a week, a small average increase in the PR interval of 2-3 ms was observed compared to baseline, while the frequency of first degree atrioventricular block was 1.5% and 2. 4%, respectively.
Immunogenicity
In clinical studies, the use of dulaglutide was accompanied by the detection of antibodies to dulaglutide with a frequency of 1.6%, indicating that structural changes in GLP-1 and modified IgG4 regions in the dulaglutide molecule, along with high homology to native GLP-1 and native IgG4, minimize the risk development of an immune response during dulaglutide therapy. Patients who developed antibodies to dulaglutide generally had low antibody titers; however, despite the small number of patients who developed antibodies to dulaglutide, evaluation of the results of phase III clinical trials did not reveal a clear effect of antibodies to dulaglutide on changes in HbA1c. None of the patients with systemic hypersensitivity developed antibodies to dulaglutide.
Hypersensitivity
In phase II and III clinical studies, systemic hypersensitivity events (eg, urticaria, edema) were observed in 0.5% of patients receiving dulaglutide. In post-registration experience with dulaglutide, cases of anaphylactic reactions have been reported rarely.
Reactions at the injection site
Administration site reactions were observed in 1.9% of patients treated with dulaglutide. Potentially immune-mediated injection site adverse events (eg, rash, erythema) were reported in 0.7% of patients and were usually mild.
Early termination of participation in clinical trials due to an adverse event
In 26-week studies, the rate of early withdrawal due to adverse events was 2.6% (0.75 mg once weekly) and 6.1% (1.5 mg once weekly) with dulaglutide compared with 3.7% with placebo. Throughout the study (up to 104 weeks), the rate of early discontinuation due to adverse events with dulaglutide was 5.1% (0.75 mg once a week) and 8.4% (1.5 mg once a week). . The most common adverse events that led to early discontinuation of participation in the dulaglutide 0.75 mg and 1.5 mg once weekly groups were nausea (1.0% and 1.9%), diarrhea (0.5% and 0.6%) and vomiting (0.4% and 0.6%), mainly such reactions were observed during the first 4-6 weeks of therapy.
Gliptins and bone tissue
Bone is one of the target organs in diabetes. An increased risk of osteoporotic fractures has been established in both types of diabetes [47]. Recently, the results of a meta-analysis of 28 randomized clinical trials with a follow-up period of at least 24 weeks in patients with T2DM were published, which compared gliptins (including sitagliptin) with placebo or an active drug. DPP-4 inhibitors, compared with placebo and other antidiabetic agents, were associated with a reduced risk of bone fractures [48].
Description of the drug INDAPRIL
In some patients with arterial hypertension without previous obvious renal impairment, laboratory signs of functional renal failure may appear during therapy. In this case, treatment should be stopped. When resuming combination therapy, the components should be used in low doses or only one of them should be used. Such patients require regular monitoring of potassium levels and creatinine concentrations in the blood serum - 2 weeks after the start of therapy and every 2 months thereafter. Renal failure occurs more often in patients with severe chronic heart failure or underlying renal impairment, incl. with renal artery stenosis.
In the case of initial hyponatremia, there is a risk of sudden development of arterial hypotension, especially in patients with renal artery stenosis. Therefore, during dynamic monitoring of patients, attention should be paid to possible symptoms of dehydration and decreased electrolyte levels in the blood plasma, for example, after diarrhea or vomiting. Such patients require regular monitoring of blood plasma electrolyte levels.
The combined use of perindopril and indapamide does not prevent the development of hypokalemia, especially in patients with diabetes mellitus or renal failure. As with the combination of any antihypertensive drug and a diuretic, regular monitoring of plasma potassium levels is necessary.
The simultaneous administration of perindopril and potassium-sparing diuretics, as well as potassium supplements, potassium-containing table salt substitutes and food additives is not recommended.
In patients with normal renal function and without concomitant risk factors, neutropenia rarely occurs. Perindopril should be used with extreme caution against the background of systemic connective tissue diseases (including systemic lupus erythematosus, scleroderma), as well as while taking immunosuppressants, allopurinol or procainamide, or a combination of these factors, especially in patients with initially impaired renal function . Some of these patients developed severe infections, in some cases resistant to intensive antibiotic therapy. When prescribing perindopril to such patients, it is recommended to periodically monitor the number of leukocytes in the blood. Patients should report any signs of infectious diseases (eg, sore throat, fever) to their doctor.
When taking ACE inhibitors, including perindopril, in rare cases, the development of angioedema of the face, extremities, lips, tongue, vocal folds and/or larynx may occur. This can happen at any time during treatment. If symptoms appear, the drug should be stopped immediately and the patient should be observed until signs of edema completely disappear. If the swelling affects only the face and lips, it usually goes away on its own, although antihistamines can be used as symptomatic therapy. Angioedema, accompanied by swelling of the larynx, can be fatal. Swelling of the tongue, vocal folds, or larynx can lead to airway obstruction. If such symptoms appear, you should immediately begin appropriate therapy, for example, administer subcutaneous epinephrine (adrenaline) in dilution 1:
- 1000 (0.3-0.5 ml) and/or ensure airway patency.
A higher risk of developing angioedema has been reported in black patients.
Patients with a history of angioedema not associated with taking ACE inhibitors may have an increased risk of developing it when taking drugs of this group.
In patients with abdominal pain receiving ACE inhibitors, when carrying out differential diagnosis, it is necessary to take into account the possibility of developing angioedema of the intestine.
There are isolated reports of the development of prolonged, life-threatening anaphylactoid reactions in patients receiving ACE inhibitors during desensitizing therapy with hymenoptera venom (bees, wasps). ACE inhibitors should be used with caution in patients prone to allergic reactions undergoing desensitization procedures. Prescription of an ACE inhibitor should be avoided in patients receiving immunotherapy with hymenoptera venom. However, anaphylactoid reaction can be avoided by temporary withdrawal.
In rare cases, life-threatening anaphylactoid reactions have developed in patients receiving ACE inhibitors during LDL apheresis using dextran sulfate. To prevent an anaphylactoid reaction, ACE inhibitor therapy should be temporarily discontinued before each apheresis procedure.
Anaphylactoid reactions have been reported in patients receiving ACE inhibitors during hemodialysis using high-flux membranes (eg, AN69®). Therefore, it is advisable to use a different type of membrane or use an antihypertensive agent of a different pharmacotherapeutic group.
In some pathological conditions, significant activation of the RAAS may be observed, especially with severe hypovolemia and a decrease in plasma electrolytes (due to a salt-free diet or long-term use of diuretics), in patients with initially low blood pressure, renal artery stenosis, chronic heart failure or cirrhosis of the liver with edema and ascites. The use of an ACE inhibitor causes a blockade of this system and therefore may be accompanied by a sharp decrease in blood pressure and/or an increase in the concentration of creatinine in the blood plasma, indicating the development of functional renal failure. These phenomena are more often observed when taking the first dose of the drug or during the first two weeks of therapy. Sometimes these conditions develop acutely and during other periods of therapy. In such cases, when resuming therapy, it is recommended to use the drug at a lower dose and then gradually increase it.
Before starting to take the drug, it is necessary to assess the functional activity of the kidneys and the potassium content in the blood plasma. At the beginning of therapy, the dose of the drug is selected taking into account the degree of reduction in blood pressure, especially in the case of dehydration and loss of electrolytes. Such measures help to avoid a sharp decrease in blood pressure.
The risk of arterial hypotension exists in all patients, however, special care should be taken when using the drug in patients with coronary artery disease and cerebrovascular insufficiency. In such patients, treatment should be started with low doses.
Treatment with the combination of perindopril/indapamide in patients with diagnosed or suspected renal artery stenosis should begin with a low dose of the drug in a hospital setting, monitoring renal function and potassium levels in the blood plasma. Some patients may develop functional renal failure, which disappears when this combination is discontinued.
In persons with severe heart failure (NYHA functional class IV) and patients with type 1 diabetes mellitus (risk of spontaneous increase in potassium levels), treatment should begin with a low dose of the drug and under close medical supervision.
During the first month of therapy with ACE inhibitors, plasma glucose concentrations should be carefully monitored in patients with diabetes mellitus and treated with oral hypoglycemic agents or insulin.
Perindopril, like other ACE inhibitors, apparently has a less pronounced antihypertensive effect in patients of the Black race compared to representatives of other races. This difference may be due to the fact that black patients with arterial hypertension are more likely to have low renin activity.
Carrying out general anesthesia while using ACE inhibitors can lead to a significant decrease in blood pressure, especially when using general anesthesia agents that have a hypotensive effect. It is recommended, if possible, to stop taking long-acting ACE inhibitors, incl. perindopril, the day before surgery. It is necessary to warn the anesthesiologist that the patient is taking ACE inhibitors.
If jaundice appears or a significant increase in the activity of liver enzymes while taking ACE inhibitors, you should stop taking the drug and consult a doctor.
Hyperkalemia may develop during treatment with ACE inhibitors, incl. and perindopril. Hyperkalemia can cause serious, sometimes fatal, abnormal heart rhythms. Risk factors for hyperkalemia are renal failure, deterioration of renal function, age over 70 years, diabetes mellitus, certain concomitant conditions (dehydration, acute decompensation of heart failure, metabolic acidosis), concomitant use of potassium-sparing diuretics (such as spironolactone and its derivative eplerenone, triamterene, amiloride ), as well as a number of medicines. In such cases, treatment should be carried out with caution and regular monitoring of serum potassium levels.
Before starting treatment, it is necessary to determine the content of sodium ions in the blood plasma. While taking the drug, this indicator should be regularly monitored. All diuretics can cause hyponatremia, which sometimes leads to serious complications. Hyponatremia at the initial stage may not be accompanied by clinical symptoms, so regular laboratory monitoring is necessary. More frequent monitoring of sodium ion levels is indicated for patients with liver cirrhosis and elderly patients.
Therapy with thiazide and thiazide-like diuretics is associated with a risk of hypokalemia. Hypokalemia (less than 3.4 mmol/L) should be avoided in the following high-risk patients:
- elderly patients, malnourished patients (both those receiving and not receiving concomitant drug therapy), patients with liver cirrhosis (with edema and ascites), coronary artery disease, heart failure. Hypokalemia in these patients increases the toxic effect of cardiac glycosides and increases the risk of developing arrhythmias.
Patients with a prolonged QT interval, either congenital or drug-induced, are also at increased risk.
Hypokalemia, like bradycardia, contributes to the development of severe heart rhythm disturbances, especially polymorphic ventricular tachycardia of the “pirouette” type, which can be fatal. In all the cases described above, more regular monitoring of the content of potassium ions in the blood plasma is necessary. The first measurement of potassium ion content should be carried out within the first week from the start of therapy. If hypokalemia is detected, appropriate treatment should be prescribed.
Thiazide and thiazide-like diuretics may reduce the excretion of calcium ions by the kidneys, leading to a slight and temporary increase in plasma calcium concentrations. Severe hypercalcemia may be a consequence of previously undiagnosed hyperparathyroidism. Before studying the function of the parathyroid glands, you should stop taking diuretics.
It is necessary to monitor blood glucose concentrations in patients with diabetes mellitus, especially in the presence of hypokalemia.
When the concentration of uric acid in the blood plasma increases during therapy, the frequency of gout attacks may increase.
Thiazide and thiazide-like diuretics are fully effective only in patients with normal or slightly impaired renal function (plasma creatinine concentration in adults below 25 mg/l or 220 µmol/l).
At the beginning of diuretic treatment, patients may experience a temporary decrease in GFR and an increase in plasma urea and creatinine concentrations due to hypovolemia and hyponatremia. This transient functional renal failure is not dangerous for patients with initially normal renal function, but its severity may increase in patients with renal failure.
Indapamide may give a positive reaction during doping control.
Impact on the ability to drive vehicles and machinery
The action of indapamide and perindopril, either individually or in combination, does not lead to impaired psychomotor reactions. However, some people may develop different individual reactions in response to lowering blood pressure, especially at the beginning of treatment or when other antihypertensive drugs are added to the therapy. In this case, the ability to drive a car or operate other machinery may be reduced.