Published 06/21/2019
Cervical cancer is the leading cause of death in women aged 30 to 35 years. At the same time, a woman often cannot detect the pathology on her own, experiencing minor complaints.
The cervix has a special anatomical structure. It is designed in such a way that the gynecologist can only see gross changes in the cervix, which, as a rule, are an indicator of an advanced process. A more detailed examination of the cervix for pathology is possible only under high magnification, which is precisely provided by a device called a colposcope.
Colposcopy of the uterus
Colposcopy of the uterus is a diagnostic procedure that is performed using a colposcope (a special optical instrument with a lighting device) and is aimed at examining the walls of the vagina and the visible vaginal part of the cervix.
During the examination, the doctor may:
- perform a biopsy of certain areas of the cervix for subsequent histological analysis;
- collect the necessary material for subsequent laboratory diagnostics of bacteriological and cytological smears;
- enlarge the image 2, 5, 7, 10, 15 or more times for a more detailed study of the structure of tissues.
In our clinic, this diagnostic procedure is performed using an expert-class colposcope. Its results will allow the doctor to identify pathology at the initial stage of its development, draw up a detailed picture of the disease and prescribe an effective course of treatment.
What is colposcopy?
Gynecological examination, which is carried out using a colposcope - a medical optical or video device.
During the procedure, the doctor carefully examines the vaginal part of the uterus and cervix, vagina and vulva under magnification.
Medical equipment used
Optical colposcopes are devices that have built-in lenses (optical unit) and a powerful light source with adjustable brightness. Modern devices allow examining the tissue under study under magnification up to 30–40 times.
Video colposcopes are equipped with high-resolution digital video cameras that provide high-quality and color images. The “picture” is transmitted to the colposcope or computer monitor. The image is saved in the memory of the device or computer, which makes it possible to subsequently compare the results of several studies.
Indications for colposcopy
Indications for colposcopy may include the following diseases:
- true erosion and pseudo-erosion of the cervix;
- cervical polyps;
- cervical endometriosis;
- inflammatory diseases of the cervical canal and vagina (vaginosis, colpitis, cervicitis, gonorrhea, trichomoniasis, etc.);
- suspected carriage of human papillomavirus;
- endometrial hyperplasia;
- uterine fibroids.
Indications for this study may include the following conditions:
- discharge and itching in the vagina;
- identifying signs of cell atypia in a cytological smear;
- intermenstrual bleeding;
- pain during or after sexual intercourse;
- discharge after sexual intercourse;
- frequent and prolonged pain in the lower abdomen;
- detection of genital warts on the external genitalia;
- detection of ruptures after childbirth;
- monitoring the condition of women with uterine erosion;
- monitoring the condition of women at risk for the development of cervical cancer;
- monitoring the condition of women after treatment of cervical pathologies.
Colposcopy: why is it needed and what will it show?
The doctor has referred you or your loved one for a colposcopy. Marina Viktorovna Peshina, an obstetrician-gynecologist of the highest category at the Expert Clinic Perm, told us about what this procedure is, for what purpose it is performed, and whether colposcopy is painful.
— Marina Viktorovna, what is colposcopy? Why is it carried out?
— This is a study used in gynecology to examine the cervix in order to identify underlying, inflammatory diseases or oncological processes.
— What types of colposcopy are there?
— There are two types of colposcopy: simple and extended. Simple is just an examination of the cervix under a microscope. And the extended one always includes testing, i.e. treatment with a solution of acetic acid, Lugol's solution (an aqueous solution of iodine). In practice, extended colposcopy is mainly used, since a simple one gives us little information. With a simple colposcopy, the doctor can see, for example, only condyloma, polyp, advanced cervical cancer, etc. But precancerous processes cannot be seen without testing.
— Please tell us in more detail what colposcopy shows. What pathologies can be identified using this study?
— Colposcopy allows the doctor to see the epithelium of the cervix under magnification of 30–60 times. What pathologies can we identify on the cervix? These are pathologies of the cervix itself:
- chronic cervicitis, or erosion, as it is popularly called, i.e., an inflammatory process;
- dysplasia;
- cancer;
- some proliferative processes (for example, polyp of the cervical canal, cysts on the cervix);
- scars or tears after childbirth.
When we examine the cervix, we also see the entire vagina. You can see, for example, vaginal cysts, growths of condylomas on the cervix and on the walls of the vagina.
— How to prepare for colposcopy?
— No special preparation is needed for colposcopy. But it is advisable that the woman keep sexual rest the day before, because there may be some irritating factors or allergic reactions, for example, to latex. You can't douche. In addition, the procedure is not performed during menstruation.
— On what day of the cycle can a colposcopy be done?
— It is advisable to do both simple and extended colposcopy in the first phase of the cycle after menstruation, because during the second phase there may be a little more discharge in the vagina that interferes with examination of the cervix. If your period lasts up to a maximum of 7 days, then starting from the 7th to the 14th–16th day of the cycle are the best days for colposcopy. Everyone’s cycle is different: 25, 28 days, some women even have 33 days. The first phase is, roughly speaking, half of the cycle.
— Marina Viktorovna, is it possible to do colposcopy during pregnancy?
- Yes. The study does not pose any threat to either the expectant mother or the baby. The doctor simply inserts a vaginal speculum and examines the desired area.
— How is colposcopy done? Is this a painful procedure?
- This is the same as an examination in a gynecological chair, only we also conduct an examination through a microscope. The procedure is completely painless. Many women confuse colposcopy with a biopsy or with cauterization (a type of cervical treatment). But these are completely different things. Colposcopy – from the Greek word “skopiya”, i.e. to look. This is just an inspection. And if any additional manipulations are needed, the doctor, based on the results of the colposcopy, decides what to do next: either simply observe the patient, or actually need to give her a biopsy.
— In addition to colposcopy, doctors can prescribe other diagnostic methods. Among them, for example, cytological examination. What is better to do: colposcopy or cytology smear?
— There is such a thing as cancer screening. What does it include? For example, to prevent breast cancer, mammography is performed throughout Russia. Gynecological cancer screening includes a cytological smear. What is cytology? This is a smear taken from the cervical canal to detect cancer cells. We look to see if there are any changes in the canal, because very often oncological processes begin there. And this screening is not discussed. That is, all gynecologists a priori, without waiting for complaints, at almost every first appointment the patient takes a smear for oncocytology. The question here is not what is best to do. Cytology is mandatory for all women of childbearing age and older women. We decide whether to do a colposcopy either based on the results of a cytological smear, or based on some of the woman’s complaints, or based on a visual examination in the chair. That is, colposcopy is an additional research method.
Read more about cytology smears in our article: Cytology smears: how to decipher correctly?
— To make a diagnosis, a woman is often prescribed an ultrasound examination of the pelvis. Is it possible to perform an ultrasound and colposcopy on the same day?
— Nowadays, for most patients (except virgins), ultrasound is usually performed with a gynecological sensor, which is inserted into the vagina. And, of course, a condom and a special lubricating gel are used. Therefore, if you have these two procedures on the same day, then it is advisable to do a colposcopy before the ultrasound so that there is no lubricating gel or anything else irritating in the vagina. And so both procedures can be done on the same day without problems.
But ultrasound does not particularly help us in diagnosing cervical pathology. If, of course, we see some formations on the cervix that look like cancer, then we also refer you for an ultrasound regarding the pathology of the cervix to see whether there is growth into neighboring tissues, space-occupying formations in the pelvis or not.
You can sign up for a pelvic ultrasound here. ATTENTION: the service is not available in all cities
— Who should not have a colposcopy? Are there any contraindications to this study?
— There are almost no contraindications to this diagnostic method. Colposcopy is technically impossible for virgins, although we have special mirrors. But this procedure is performed very rarely on girls.
Contraindications for colposcopy are mainly menstrual days. In addition, many doctors (including me) do not perform colposcopy when the patient has bad tests and smears. If there is a pronounced inflammatory process in the vagina (itching, pain, a lot of discharge, the walls and epithelium are irritated), then it is better to postpone the study. First you need to relieve inflammation and only then perform colposcopy. This is done in order to correctly interpret the study result and not confuse one disease with another.
I would like to add that colposcopy is becoming increasingly important, since quite often during a routine appointment the beginning changes in the cervix are not visible. There is currently a very high level of infection with the human papillomavirus (HPV). This is a virus that, according to all data, contributes to the future development of cervical cancer. And if a woman is diagnosed with HPV, then, I would say, she must undergo a colposcopy.
You can make an appointment with an obstetrician-gynecologist here. ATTENTION: the service is not available in all cities
Interviewed by Marina Volovik
The editors recommend:
What will a gynecological ultrasound show? What does an MRI of the pelvis show in women? Polycystic ovary syndrome: how is it diagnosed and treated? Cervical polyp: why does it appear and what to do with it?
For reference:
Peshina Marina Viktorovna
In 1998 she graduated from the Perm State Medical Academy with a degree in General Medicine. 1999 – internship in obstetrics and gynecology. Gynecologist of the highest category. Work experience 22 years. Proficient in all methods of diagnosis and treatment of any gynecological diseases, including aesthetic gynecology and cervical pathology. Currently, he is an obstetrician-gynecologist and endocrinologist at the Expert Clinic in Perm. Reception is conducted at the address: st. Monastyrskaya, 42a.
Why is cervical colposcopy performed?
The main purpose of colposcopy is aimed at determining the boundaries, malignancy or benignity of the pathological focus. During the research process the following can be determined:
- border of pathology;
- differentiation of the tumor process;
- identification of the inflammatory process;
- the need to perform a tissue biopsy from the pathological focus;
- exact area of tissue for biopsy.
After analyzing all the data obtained, the results of colposcopy allow the doctor to draw up a plan for further effective treatment.
About the colposcope
We are talking about a microscope that is specially designed for non-contact study. The device has a fairly simple structure. The doctor freely places the device near the patient, choosing the most convenient location for better study.
Content:
- Brief information
- About the colposcope
- Objectives of the method
- Indications for the procedure
- Manipulation technique
- What is being assessed?
- Preparing for colposcopy
- Varieties of techniques
- Colposcopic tests
- Is there any danger to the procedure?
- Contraindications to manipulation
- The effectiveness of the technique
- After the procedure
The optical part of the device is a prismatic binocular with interchangeable eyepieces. The stereoscopic part of the device is equipped with an additional illuminator.
Types of colposcopy of the uterus
Depending on the colposcope model used and the research methodology, the following types of colposcopy are distinguished:
- simple (overview);
- extended;
- chromocolposcopy;
- fluorescent;
- with color filters;
- colpomicroscopy.
Depending on the type of colposcope, the following can be performed:
- simple colposcopy;
- photocolposcopy (the results are reflected in photographs);
- video colposcopy (results can be recorded on various media and the patient herself can observe the examination process).
Composition of a colposcope
Colposcopes come in two types: those with a fixed focal length lens whose magnification can be changed by changing the power of the eyepieces, and those with a fixed focal length lens but with multiple magnifications where the dial setting can be changed or a button pressed. .
Increase
Multiple magnifications are preferred, starting at ×5 or ×7.5, ×20 or ×30. The lowest magnification gives a bird's eye view and is great for locating or zooming in on an area of interest. The magnification commonly used for detailed examination is ×15. The modern colposcope is based on the original prototype, but differs from the original in that the magnification varies from 6 to 40 times, as opposed to the original 7.5 times. 10x magnification is suitable for everyday use. Higher magnification allows you to recognize some minor points, but it is not necessary to use it for an accurate diagnosis.
The most important accessories for a colposcope are photographic equipment and special spare parts for teaching. Also, simple low-power devices without any accessories are always available on the market, as well as more complex ones with electrical control, a zoom lens with fine tuning and a camera. For routine use, a simple colposcope is fine, but for training, both the camera and viewing tube are essential. All colposcopes have lenses, eyepieces, filters, a light source and a stand.
Lens
This in turn affects the focal length and therefore the working distance. The best focal length is between 250mm and 300mm. This allows you to easily operate and manipulate tools without interfering with your vision.
Eyepieces
Eyepieces must have the following good characteristics: the axes of the eyepieces can be straight or inclined at an angle of 45° to the optical axis of the device, they must have rubber cups installed on them, they must have independent focusing elements that adapt to human vision. Also one very important feature is the convergent line of sight for fatigue-free working.
Filters
Most colposcopes are equipped with green filters. They absorb red light and enhance the image of blood vessels that appear black. The contrast between normal and abnormal epithelium is also enhanced.
Light source
The light source must be at least 30,000 lux, must be constantly centered, and must have a rheostat to vary the light intensity. Some equipment has automatic brightness adjustment depending on the magnification used. Most colposcopes are equipped with a halogen lamp with a power of 6 to 12 W and 20 to 75 W. A recent innovation is the light emitting diode (LED), which is a better light source. They generate light through semiconductor processes rather than heating a wire filament, as in a halogen lamp. The advantages of an LED light source are that its light output is five to seven times higher than that of a lamp; this light uses a different optical system, significantly improving contrast, and with it overall visibility improves. The service life of an LED is also many times higher (up to 10,000 hours) than a halogen lamp. It lasts for approximately 10 years with daily use of approximately 4 hours.
Simple colposcopy
During a simple colposcopy, the doctor examines the surfaces of the walls of the vagina and cervix under magnification. Then, using a tampon, the discharge is removed and the examination is repeated.
Using a simple colposcopy, the doctor can roughly assess:
- shape and size of the cervix and external os;
- relief and color of the mucous membrane;
- the severity of the vascular pattern;
- boundaries of flat and columnar epithelium.
This procedure is performed without prior preparation of the patient. It takes little time, is absolutely safe and painless.
To obtain a more detailed clinical picture, our clinic may prescribe other more informative types of colposcopies.
Colposcopy and pregnancy
The study is done in pregnant women to determine whether invasive cervical cancer exists. Because the procedure is more difficult in a pregnant woman due to several factors such as increased mucus and uterine production.
If the initial test is inconclusive, the test should be repeated every six to twelve weeks or after 20 weeks. Because the pregnant cervix tends to bleed excessively, a biopsy is usually avoided for fear of harming the unborn baby. Typically, a biopsy is performed on a pregnant woman if all evidence indicates a huge risk of developing cancer or dysplasia. A colposcopy done correctly will never harm the patient if she is pregnant, and it will not harm her fetus in any way.
Extended colposcopy
Extended colposcopy provides more accurate and detailed results. It is carried out using various tests and dyes. For the standard procedure, 3% solutions of acetic acid and Lugol with glycerin are used as dyes. When conducting this type of examination, the woman undergoes special training, and before it begins, secretions are removed from the surface of the vagina and cervix using a sterile swab.
When performing an extended colposcopy, the doctor can evaluate:
- appearance and color of the cervix;
- the severity and condition of the vascular pattern;
- relief of the mucous layer of the cervix;
- the junction of the epithelium of the cervix and the cervical canal;
- condition and presence of glands;
- mucosal reaction to vinegar solution;
- reaction of the mucous membrane to Lugol's solution (Schiller test);
- type of epithelium;
- clarity or blurring of the boundaries of formations.
Also, for extended colposcopy, color filters, Chrobok's test (with a probe) and staining of the mucous membrane with methylene blue, eosin, hematoxylin (Derazhne test), fluorochrome or trichlortetrazole can be used. These types of this procedure make it possible to draw up a more detailed picture of the disease, determine the malignancy of the tumor and more clearly visualize the contours of blood vessels.
Historical facts
In 1924, Hinselmann was asked to write a chapter based on the etiology, symptoms and diagnosis of uterine cancer in the third edition of the Handbook of Gynecology. Hinselmann faced this challenge most successfully. He performed gynecological examinations and often encountered early detection of cervical cancer, which he believed could only be improved by optical means. He believed it was necessary to "provide an intense light source for the magnified image without sacrificing binocular vision."
Content:
- Historical facts
- Composition of a colposcope
- Indications for the use of colposcopy
- Differences between simple and extended colposcopy
- Preparing for the examination
- Methodology
- Complications after extended colposcopy
- Contraindications for the study
- Colposcopy and pregnancy
- Study protocol
By 1925, he reported the construction of the first colposcope. To this end, he connected a light source to Lake's binocular biological microscope. He connected the optical system to a stand that allowed movement in each direction and also supported a small screw for fine adjustment. After the invention of the colposcope, Hinselmann was able to state that “with regard to so-called early problems, colposcopy makes it possible to detect earlier cases.” Even a tiny tumor the size of a dot did not disappear and was visible even with an initial magnification of 7.5 times. Thus, Hinselmann discovered a completely new invention and proved its significance in the field of medicine.
Fluorescence colposcopy
Fluorescence colposcopy allows to detect the malignancy of a cervical tumor in 98% of cases. This type of colposcopy is performed using a special dye and UV rays.
After treating the cervix with fluorochrome, the cervix is examined under UV rays and the doctor evaluates the resulting glow:
- Normally, the unchanged mucous membrane has a violet or dark blue glow;
- in the early stages of a malignant tumor – the mucous membrane has a crimson, light green or bright yellow glow;
- in the later stages of a malignant tumor, the glow goes out.
Study protocol
Best materials of the month
- Coronaviruses: SARS-CoV-2 (COVID-19)
- Antibiotics for the prevention and treatment of COVID-19: how effective are they?
- The most common "office" diseases
- Does vodka kill coronavirus?
- How to stay alive on our roads?
Each woman who has undergone this diagnostic method is given a protocol with the results of the examination. It must be completed by the doctor who examined the patient. The results sheet includes the following items: type of cervix (cylindrical, conical, hypertrophied, deformed), type of external uterine pharynx (round, slit-like, semilunar), rupture (yes, no, post-traumatic deformation), ectropion (yes, no), ectopia columnar epithelium (yes, no). Normal transformation zone: open glands or closed (Nabothian cysts), keratinized glands. Atypical transformation zone: acetate, iodine-negative epithelium, punctation (pinpointing - tender, rough), mosaic - tender, rough. Presence of vessels (yes, no, regular type, strengthening, atypical), leukoplakia (yes, no), cervical relief (smooth, uneven, raised), presence of scar changes, coagulated cervical syndrome, endometriosis, polyps, exophytic condylomas, inflammation (diffuse and local), atrophy, ulcers (true erosions), pinpoint ulcerations.
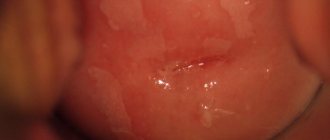
Normal cervical mucosa
The mucous membrane of the vaginal part of the cervix is covered with stratified squamous epithelium; upon examination, it has a pale pink color and shines. It has a cyanotic tint in the second half of the menstrual cycle in women. The pattern of vessels is of the correct type, evenly spaced, the relief of the cervix is even. Any other pathologies are a signal for further research and treatment.
It can be concluded that this research technique is absolutely safe and painless, it allows you to carry out both diagnostic and therapeutic measures, for example, it can be used to remove polyps and condylomas, and perform a biopsy of a suspicious area. The study allows us to identify inflammatory diseases, carry out differential diagnostics, and identify serious pathologies in the early stages with the possibility of early treatment.
More fresh and relevant information about health on our Telegram channel. Subscribe: https://t.me/foodandhealthru
We will be grateful if you use the buttons:
What time of day is best to perform a colposcopy?
Colposcopy can be performed at any time of the day. The most favorable moment for its implementation is the days of the first half of the menstrual cycle. It is best to carry out this procedure 2-3 days after the end of menstrual bleeding.
Colposcopy is not performed during menstruation, because bleeding and rejection of areas of the uterine cavity mucosa interfere with a detailed examination of the vaginal walls and the visible part of the cervix. Such a procedure will be uninformative and meaningless.
It is undesirable to perform colposcopy during the first 2-3 days after ovulation, because during this period of the cycle a large amount of mucus accumulates in the cervical canal, which distorts the results and interferes with the procedure. In the second half of the menstrual cycle, performing this diagnostic procedure is also undesirable, because after its implementation, the mucous membrane of the cervix will take a longer time to recover.
Why is a colposcope examination performed?
The examination allows us to identify benign, precancerous and already developed tumor processes, inflammation, and erosive changes in the mucous membrane. Diagnostics helps to timely monitor women's health by treating precancerous processes and cancer. The device clearly shows destructive ectropia, endometriosis, genital warts, and erythroplakia.
The tests use a green filter and fairly bright lighting to improve visualization of the choroidal network.
Indications for colposcopic examination:
- itching in the genital area;
- lower abdominal pain;
- discharge unusual for menstruation;
- inflammation of the cervix, especially chronic;
- vaginal bleeding (except menstrual bleeding);
- cell changes identified by the results of an oncocytological smear;
- the likelihood of leukoplakia, erythroplakia and other pathologies.
Pain in the lower abdomen
Examination for the prevention of precancer, chronic endometriosis, erosions, polyps and ectopia of the cervix is carried out twice a year.
Preparing for colposcopy
After prescribing colposcopy, the doctors of our clinic will definitely familiarize the patient with the simple rules of preparation for this diagnostic procedure, since the accuracy of their implementation may depend on the reliability of the results obtained.
Preparation for colposcopy should begin 4-5 days before the procedure. The set of these measures includes the following recommendations:
- 4-5 days before the procedure, stop using any medications that are inserted into the vagina;
- 2-3 days before the procedure you should stop douching;
- 2 days before the procedure, you should use only warm water for washing and refrain from using any detergents;
- 1-2 days before the procedure, you must stop using lubricants;
- 1-2 days before the procedure, you should abstain from vaginal intercourse (if it is impossible to exclude sexual intercourse, you should use a condom).
No other specific preparation is required for cervical colposcopy.
How to prepare for research?
No specific preparation is required. One should only take into account the fact that since During the procedure, test solutions will be used - it is advisable to take a thin sanitary pad with you to protect your underwear from contamination by them.
If you are planning to take a cytological smear, you should follow several recommendations for two days before taking the test:
- refrain from intimacy;
- do not use suppositories and vaginal ointments (unless your doctor recommends otherwise);
- use intimate cosmetics and tampons.
Stages of cervical colposcopy
Colposcopy is performed on an outpatient basis or in a hospital after completing preparation for this procedure.
Colposcopy includes the following steps:
- the woman is examined on a gynecological chair using a regular gynecological speculum, which remains in the vagina throughout the entire subsequent procedure;
- the vaginal walls and cervix are dried with sterile cotton swabs to remove mucus;
- the colposcope is installed at the gynecological speculum a few centimeters from the entrance to the vagina;
- the doctor, using a colposcope, sequentially examines the walls of the vagina and the visible part of the cervix and selects areas for testing or biopsy;
- using a clamp with a tampon soaked in a 3% solution of acetic acid, the doctor treats the cervix;
- Normally, under the influence of acetic acid, the walls of blood vessels undergo spasm and completely disappear after 30-60 seconds;
- in the presence of cancerous degeneration of cells after treatment with acetic acid, the disappearance of the vascular pattern is not observed;
- after assessing the results of treating the epithelium with vinegar, the doctor performs a Schiller test, which is carried out by applying a 3% Lugol’s solution with glycerin to the cervix;
- Normally, under the influence of this test, the entire surface of the mucous membrane turns dark brown;
- in the presence of cancerous degeneration of cells, after testing, unpainted areas are revealed on the surface of the cervix;
- after performing the Schiller test, other additional research techniques can be performed (fluorescence colposcopy, chromocolposcopy and colpomicroscopy);
- if necessary, the doctor uses special forceps to perform a tissue biopsy from suspicious areas;
- a sample of tissue taken for histological examination is placed in a test tube and sent to the laboratory;
- After completion of the procedure, the colposcope is moved back and the gynecological speculum is removed from the vagina.
After colposcopy, the woman receives a doctor’s report, an invitation to the next appointment, and can go home. The results of the biopsy (if performed) will be ready in 1-2 weeks.
“Look” from the inside: why do you need colposcopy?
The examination helps to diagnose diseases in a timely manner with subsequent monitoring of the effectiveness of treatment.
Basic goals
1. Detection of pathologically altered tissue areas - neoplasms of the female reproductive system in the early stages.
The most serious is cancer of the female reproductive system. In the world, cervical cancer ranks 2nd in the frequency of malignant tumors among women; in the Russian Federation it ranks 6th. Every year, 200–300 thousand women die from this pathology in the world, and about 6,000 patients in the Russian Federation.
2. Choosing the optimal treatment method: cauterization with medications, removal with a laser, surgical instrument, etc.
3. Evaluation of treatment results and dynamic monitoring of previously detected pathological formations.
Detected diseases:
* cancer of the cervix, vagina and vulva;
* erosion/ectopia - mucosal cells from the cervical canal move to the vaginal part of the cervix (looks like ulceration on the mucous membrane);
* dysplasia is the most common form of cervical precancer, in which the normal structure of mucosal cells on the surface of the cervix is disrupted;
* cervicitis - inflammation of the mucous membrane of the cervical canal;
* anogenital condylomas or warts - formations in the form of papillae or flesh-colored nodules and many others.
Is it painful to have a cervical colposcopy?
Colposcopy is not accompanied by pain, since the colposcope is not inserted into the vagina. During the study, some women may feel discomfort from the cold gynecological speculum and slight tingling after treating the cervix with a solution of acetic acid.
The biopsy that may be performed during this test may cause short-term discomfort or mild pain. The painlessness of this manipulation largely depends on the skill of the doctor.
In our clinic, the colposcopy procedure is performed only by experienced gynecologists and patients do not experience pain.
Contraindications
Despite the simplicity of the study, there are a number of contraindications to colposcopy:
- first 8 weeks after birth,
- 3-4 weeks after the abortion,
- recent treatment of the cervix using cryodestruction or surgical treatment.
When performing a special, extended colposcopy, a contraindication is an allergy to iodine or acetic acid.
Temporary contraindications for colposcopy may include:
- bleeding from the uterus or cervix, including menstruation,
- pronounced inflammatory process,
- severe state of ectocervix atrophy.
See also: Diabetes School
What happens after colposcopy of the uterus?
After colposcopy of the cervix for 3-5 days, a woman may experience slight dull and nagging pain in the lower abdomen and bloody, pink, dark brown or greenish discharge from the genital tract. The appearance of discharge is explained by the healing of the scar left on the cervix after cutting off sections of tissue for biopsy, or by the removal from the vagina of remnants of dyes used for colposcopy.
These symptoms are normal, go away on their own and do not require seeing a doctor. After completing the procedure, the doctor must warn the woman about the possibility of pain and discharge and recommend:
- use sanitary pads for 3-5 days;
- do not use vaginal tampons;
- After the biopsy, for 10 days do not take medications that thin the blood (Aspirin, Ibuprofen, etc.), do not visit the sauna or bathhouse, do not take a bath, do not have sex, and avoid heavy physical activity.
In some cases, colposcopy may be complicated by infection of the genital tract or bleeding after the biopsy. A woman should seek medical help if symptoms such as:
- profuse bleeding from the genital tract;
- temperature increase;
- chills;
- intense pain in the abdomen or lower back;
- discharge from the genital tract with an unpleasant odor.
Abnormal colposcopic patterns
The presence of pathological changes may be indicated by detection during extended colposcopy:
- acetowhite epithelium;
- iodine-negative zones;
- signs of leukoplakia;
- punctuation;
- mosaics;
- atypical transformation zone;
- signs of invasive cancer.
All these cases require an individual approach and additional diagnostic procedures, including biopsy, PAP test, etc. Mild lesions are characterized by the detection of dense acetowhite epithelium with clear boundaries, delicate mosaics and punctures. With pronounced changes, rapid whitening of the treatment area is observed with the appearance of dense acetowhite epithelium and a rim around the open glands. Also in such situations, rough mosaic and punctation, signs of tuberosity, are observed.
Separately, mixed colposcopic patterns are distinguished, which are difficult to unambiguously classify. These include such “findings” as genital warts, inflammatory processes, atrophic changes in the mucous membrane, endometriosis, polyps, etc. In such cases, treatment is also prescribed, which can be either conservative or surgical, or additional examination.
Acetowhite epithelium
The appearance of areas of white or acetowhite epithelium when exposed to 3% acetic acid is one of the most important signs of pathology. Most researchers agree that the vast majority of areas in which the development of malignant processes is observed turn white with varying intensity under the influence of acetic acid.
Detection of acetowhite epithelium is typical for all degrees of CIN and makes it possible to diagnose the presence of changes at the earliest stages of development. CIN refers to cervical dysplasia, which is accompanied by the formation of cells with varying degrees of atypia in the covering epithelium. Untreated dysplasia can lead to cervical cancer, and each case of its development is the result of missed opportunities and ignoring the importance of regular colposcopy.
It is important to differentiate white epithelium from areas of dyskeratosis, i.e. leukoplakia. Some blanching of the mucous membrane can also be observed with:
- disturbances in the structure of epithelial cells;
- inflammatory process;
- papillomavirus infection;
- some other benign changes.
The more intense the whitening of the tissue and the longer it persists after exposure to acetic acid, the more serious and profound the changes.
Iodine-negative zones
A typical sign of pathology is the identification of so-called silent iodine-negative areas of the mucosa after applying Lugol's solution. In most cases, they are represented by keratinized epithelium and require a more detailed examination by performing a biopsy.
Leukoplakia
Leukoplakia is a pathology accompanied by keratinization of the epithelium of the vagina, vulva or cervix. Colposcopically, it looks like a white spot of arbitrary shape with clear boundaries, which can be noticeable even before treatment of the mucous membrane with solutions. Most often, leukoplakia is observed in the area of the transformation zone and can have different sizes. The true size of the modified area is determined after treatment with Lugol's solution, since it does not turn brown. The main danger of leukoplakia is the inability to determine, without the use of invasive methods, what changes are located under the layer of keratinized cells. Therefore, if it is detected, a targeted biopsy is indicated.
punctuation
Puncture refers to multiple red dots on the background of the epithelium, caused by its atypical vascularization, i.e., the formation of blood vessels. The degree of violation is determined based on the size and uniformity of the points. They are clearly visible after exposure to acetic acid, and sometimes have the appearance of papillae.
Mosaic
This term refers to the zone of the mucous membrane, which, after treatment with acetic acid, is delimited by red lines into yellowish-white segments. This area is devoid of open and closed glands. Based on the intensity of the mosaic, the degree of tissue damage is determined. Thus, with a rough mosaic, the mucous membrane takes on the appearance of a paved pavement, but more often a delicate mosaic is observed - the segments do not protrude above the level of the surrounding tissues and have a marble pattern. Most often, the mosaic is iodine-negative.
Atypical transformation zone
It is formed on the basis of normal ST, but differs in the presence of:
- atypical blood vessels;
- acetowhite epithelium;
- keratinized glands;
- leukoplakia;
- mosaics;
- punctuation;
- areas not stained with iodine.
This indicates the presence of significant changes in the structure of the epithelium and the likelihood of developing dysplasia.
Invasive cancer
The most distressing “finding” during colposcopy may be the discovery of signs of invasive carcinoma:
- atypical transformation zone with uneven tuberosity and the presence of a limited area rising above the level of surrounding tissues (plus tissue);
- ulcers;
- atypical vessels, characterized by fragility, which leads to bleeding.
As a rule, oncology develops against the background of benign changes in the cervix, which were not diagnosed and eliminated in time.
Thus, the possibilities of colposcopy are truly wide, and its accessibility, low cost and ease of implementation are its indisputable advantages. Therefore, it is important not to ignore preventive gynecological examinations and doctor’s recommendations to perform colposcopy. Often this is what makes it possible to diagnose severe pathologies in the early stages, carry out the necessary treatment and save the patient’s life.
0 0 votes
Article rating
Colposcopy after childbirth
Colposcopy after childbirth is a relevant and necessary procedure, since the cervix after this important event in a woman’s life can undergo various scarring and other changes. Also, this diagnostic study can be indicated in the presence of various diseases of the cervix, erosion, ectopia, etc. in the prenatal period.
Colposcopy in the postpartum period is recommended by the doctors of our clinic 6 weeks after the date of birth. If necessary, a cervical biopsy may be performed during this procedure.
The results of colposcopy will convince you of the absence of pathologies or will allow you to promptly identify the disease and carry out its effective treatment.
Is it possible to have a colposcopy during pregnancy?
This examination is safe. Colposcopy and tests can be performed even during pregnancy. After all, the expectant mother needs to carefully monitor her health and prepare for future births.
The best way to determine whether you need a colposcopy is to consult with your doctor. There are also contraindications to such an examination. For example, at least 2 months must pass after childbirth or surgery. After menstruation, you should wait a few days. And if inflammatory processes have already been diagnosed in the uterine area, colposcopy should be postponed.
What does this study provide?
First of all, the diagnosis of a formidable disease - cervical ectopia, with a large lesion, excessive mucous discharge from the vagina or bloody discharge is observed after sexual intercourse. In the absence of these symptoms, treatment is not required. When diagnosing erosion, the level of damage to epithelial cells is clarified to exclude precancerous processes.
Colposcopy is very important in diagnosing dysplasia (precancerous conditions), and the doctor makes an accurate diagnosis, which guarantees correct treatment tactics. The mucous membrane of the cervix is normally pink, smooth with an even network of vessels, but pathological areas resemble a bunch of grapes, have dotted or mosaic changes, and whitish areas. An irregular vascular pattern or keratinization is characteristic of cancer.
During the procedure, tissue proliferation, inflammation, erosion, and epithelial atrophy may be observed. Histological analysis of tissue confirms the results of the research.
Pregnancy and colposcopy
The question of performing colposcopy during pregnancy is relevant. This procedure is recommended for questionable results of a cervical smear in early pregnancy. The main goal is to determine the tactics for managing a pregnant woman before childbirth when diagnosed with cancer. At later dates, the procedure is not indicated due to the risk of complications.
Colposcopy becomes less comfortable and technically more complex during pregnancy. Only simple colposcopy is recommended during this period, which does not pose a threat to the fetus or the pregnant woman. After childbirth, a repeat procedure with a biopsy is performed.