Coprogram is a comprehensive analysis of feces, which allows you to evaluate the functioning of the digestive system as a whole, and the functionality of each organ separately. In order for the research results to be accurate, it is necessary to adhere to certain rules for the preparation, collection and storage of material.
General analysis (coprogram)
- 2 days before collecting biomaterial, discard tomatoes, tomato juice, pasta, beets, blueberries, pomegranates and other vegetables and fruits containing dyes.
- For 3 days, stop taking antibiotics, laxatives, and drugs that cause changes in intestinal motor function. Do not use rectal suppositories, ointments, or oils.
- Do not eat exotic fruits, vegetables and foods that are not typical for your diet as a whole. Do not overeat, exclude fatty, spicy, pickled foods.
- If you are taking medications containing iron and bismuth, they must be discontinued 2 days before stool collection.
Attention. After radiography with a contrast agent (barium), collect feces for coprogram no earlier than 7–10 days after the examination. Women are not recommended to take the test during menstruation.
Procedure for collecting stool:
Collect stool for examination in the morning, on an empty stomach. If this is difficult, you can prepare the sample in advance, but no more than 8 hours before submitting it to the laboratory. In this case, store the sample in the refrigerator (do not freeze!).
- Carry out hygiene procedures and first urinate in the toilet and flush.
- Place sterile paper (or an ironed sheet) or a disposable plastic plate in the bowl or bottom of the toilet and perform a bowel movement.
- Collect feces immediately after defecation from different places in a single portion with a special spoon mounted in the lid of a plastic container in a volume of 1–2 g (no more than 1/3 of the container’s volume). Avoid contact with urine and pieces of undigested food.
- Deliver the sample to the laboratory on the day of collection. Before delivering the sample to the laboratory, the container with stool should be kept in the refrigerator at 2–4 °C. Storage at 2-8 °C is allowed - up to 72 hours.
Coprogram: senseless and merciless
Coprogram (general stool analysis) is one of the most common tests in a domestic children's clinic or hospital. If you open the medical history of a patient with ARVI, tonsillitis, or even a traumatic brain injury, there, along with a clinical analysis of blood and urine, you will definitely find a coprogram. Most doctors have become so accustomed to this since Soviet times that the question does not even occur to them: why, in fact, stool microscopy in the treatment of otitis media or pneumonia?
We sometimes see the same picture in outpatient settings. Let’s say the child is healthy, gaining weight well, and has normal stools—it seems, what else is needed for happiness? Of course, it is a coprogram, which pediatricians must prescribe to all healthy infants at least twice, without any indication.
According to the “protocol,” the coprogram is the most important diagnostically significant analysis and is used to diagnose various diseases of the gastrointestinal tract (GIT).
Dysbacteriosis, intestinal group
To obtain the correct result, material for research is taken before the start of antibacterial therapy or in the intervals between courses of treatment, but not earlier than 2 weeks after its completion.
Attention Do not collect feces from diapers. For infants, collect material from a sterile diaper or pre-ironed onesies. If liquid feces are collected, it can be collected by placing an oilcloth under the baby.
Collection rules
- Feces should be collected in the morning, on an empty stomach.
- Carry out hygiene procedures and first urinate in the toilet and flush.
- Place sterile paper (or an ironed sheet) or a disposable plastic plate in the bowl or bottom of the toilet and perform a bowel movement.
- Collect feces immediately after defecation from different places in a single portion with a special spoon mounted in the lid of a plastic container in a volume of 1–2 g (no more than 1/3 of the container’s volume). Avoid contact with urine and pieces of undigested food.
- Deliver to the laboratory on the day of collection.
The sample can be stored for no more than 2 hours at room temperature; no more than 6 hours at 2-8 °C, more than 6 hours - frozen.
Kinds
There are several types of steatorrhea:
- Intestinal. In this case, the mucous membrane is unable to fully absorb triglycerides, so they leave the body along with the feces.
- A food type that occurs due to consumption of large amounts of fatty foods. The intestines cannot cope with digesting such amounts of fat and try to get rid of them naturally. Also, food pathology can develop as a result of acute poisoning with products with high levels of triglycerides.
- Pancreatic view. The occurrence of the disease is the result of a malfunction of the pancreas. As a result, the body stops producing enough enzymes called lipases, which help break down triglycerides.
The disease occurs in several forms:
- With a high content of neutral fat in the stool, which does not mean the development of serious pathology.
- With the presence of fatty acid in the stool.
- A form in which the symptoms of the first two types of disease are combined.
Protozoa and helminth eggs
To obtain the most reliable results, three stool examinations are recommended with an interval of 3–7 days.
Attention You cannot collect stool earlier than 3 days after an enema, an X-ray examination of the stomach and intestines, or a colonoscopy. The day before, do not take laxatives and drugs that affect intestinal motility (belladonna, pilocarpine), activated carbon, iron, copper, bismuth, barium sulfate, use fat-based rectal suppositories. Women should not collect stool during menstruation.
Collection rules
- Feces should be collected in the morning, on an empty stomach. If this is difficult, you can prepare the sample in advance, but no more than 8 hours before submitting it to the laboratory. In this case, the sample should be stored in the refrigerator (do not freeze!).
- Carry out hygiene procedures and first urinate in the toilet and flush.
- Place sterile paper (or an ironed sheet) or a disposable plastic plate in the bowl or bottom of the toilet and perform a bowel movement.
- Collect feces immediately after defecation from different places in a single portion with a special spoon mounted in the lid of a plastic container in a volume of 1–2 g (no more than 1/3 of the container’s volume). Avoid contact with urine, water and pieces of undigested food;
- Deliver to the laboratory on the day of collection.
General stool analysis
Interpretation of the results of the study “General stool analysis”
Interpretation of test results is for informational purposes only, is not a diagnosis and does not replace medical advice.
Reference values may differ from those indicated depending on the equipment used, the actual values will be indicated on the results form. Feces in infants have their own characteristics; in the first 2-3 days after birth, the child excretes original feces (meconium), which in its characteristics differs significantly from the usual feces of both children and adults. The feces of breastfed or bottle-fed infants also have their differences.
Original feces (meconium). Meconium passage occurs 8-10 hours after birth and continues for 2-3 days. The consistency of meconium is sticky, viscous, thick, dark green in color, no odor; pH 5.0-6.0; the reaction to bilirubin is positive. Meconium is recommended to be examined in maternity hospitals to diagnose the intestinal form of cystic fibrosis in newborns.
Feces of a healthy baby during breastfeeding. Feces are a homogeneous, unformed mass, semi-viscous or semi-liquid, golden yellow, yellow or yellow-green in color with a slightly sour odor, pH 4.8-5.8. The reaction to bilirubin remains positive until 5 months of age, then, in parallel with bilirubin, stercobilin begins to be detected as a result of the restorative effect of the normal bacterial flora of the colon. By 6-8 months of age, only stercobilin is detected in the feces.
Microscopic examination of feces against the background of detritus reveals single drops of neutral fat and a meager amount of fatty acid salts. There is a small amount of mucus in the stool; the mucus contains no more than 8-10 leukocytes in the field of view.
Feces of a healthy baby with artificial feeding. The color of stool is light yellow or pale yellow, when standing in air it becomes gray or colorless, but can take on brown or yellowish-brown shades depending on the nature of the food, pH 6.8-7.5 (neutral or slightly alkaline reaction). The smell is unpleasant, slightly putrid due to the rotting of cow's milk casein. Microscopic examination reveals a slightly increased amount of fatty acid salts. In a meager amount of mucus mixed with feces, single leukocytes are found.
The table shows changes in coprogram in adults with various disorders of the digestive system.
| Insufficiency of gastric digestion | Macroscopic examination: consistency - stool is dense or mushy (formed or unformed); color - dark brown; the smell is putrid. Chemical research: pH >7.5; protein - yes; bilirubin - absent; stercobilin - present. Microscopic examination: muscle fibers without striations - in moderate or large quantities; muscle fibers with striations - in moderate quantities; connective tissue - in moderate or large quantities; indigestible plant fiber - in large quantities; digestible plant fiber - in large quantities; soap - in small quantities; starch - in small quantities; iodophilic flora - in small quantities. |
| Pancreatic insufficiency | Macroscopic examination: consistency - ointment-like; color - grayish-yellow; the smell is foul. Chemical research: pH >7.5; protein - yes; bilirubin - absent; stercobilin - present. Microscopic examination: muscle fibers without striations - in moderate or large quantities; muscle fibers with striations - in moderate quantities; connective tissue - in small quantities; indigestible plant fiber - in moderation; digestible plant fiber - in moderation; neutral fat - in large quantities; fatty acids - in small quantities; soap - in moderation; starch - in small quantities; iodophilic flora - in small quantities. |
| Lack of bile flow | Macroscopic examination: consistency - hard or ointment-like; color - grayish-white; the smell is foul. Chemical research: pH <7.0; protein - yes; bilirubin - absent; stercobilin is absent. Microscopic examination: muscle fibers with striations - in moderate quantities; muscle fibers without striations - in small quantities; indigestible plant fiber - in small quantities; digestible plant fiber - in small quantities; neutral fat - in small quantities; fatty acids - in small quantities; soap - in small quantities; starch - in small quantities. |
| Digestive insufficiency in the small intestine | Macroscopic examination: consistency - liquid; yellow color; the smell is weak. Chemical research: pH >7.5; protein - yes; bilirubin - present; stercobilin - present. Microscopic examination: muscle fibers without striations - in moderate quantities; muscle fibers with striations - in small quantities; indigestible plant fiber - in large quantities; digestible plant fiber - in large quantities; neutral fat - in moderation; fatty acids - in moderation; soap - in moderation; starch - in large quantities; iodophilic flora - in small quantities. |
| Digestive insufficiency in the large intestine: | |
| fermentative dyspepsia | Macroscopic examination: consistency - mushy, foamy; yellow color; the smell is sour. Chemical research: pH <7.0; protein - yes; bilirubin - absent; stercobilin - present. Microscopic examination: muscle fibers without striations - in small quantities; muscle fibers with striations - in small quantities; indigestible plant fiber - in small quantities; digestible plant fiber - in large quantities; neutral fat - in small quantities; fatty acids - in small quantities; soap - in small quantities; starch - in large quantities; iodophilic flora - in large quantities; mucus - in small quantities. |
| putrefactive dyspepsia | Macroscopic examination: consistency - liquid; color - dark brown; the smell is putrid. Chemical research: pH >7.5; protein - yes; bilirubin - absent; stercobilin - present. Microscopic examination: muscle fibers without striations - in small quantities; muscle fibers with striations - in small quantities; indigestible plant fiber - in small quantities; digestible plant fiber - in small quantities; neutral fat - in small quantities; fatty acids - in small quantities; soap - in small quantities; starch - in small quantities; iodophilic flora - in small quantities; mucus - in small quantities. |
| Inflammatory process in the large intestine | |
| colitis with constipation | Macroscopic examination: consistency - hard (sheep feces); color - dark brown; the smell is putrid. Chemical research: pH >7.5; protein - yes; bilirubin - absent; stercobilin - present. Microscopic examination: muscle fibers without striations - in small quantities; indigestible plant fiber - in small quantities; soap - in small quantities; mucus - in moderation. |
| colitis with diarrhea | Macroscopic examination: consistency - mushy or liquid; color - dark brown; the smell is sour. Chemical research: pH <7.0; protein - yes; bilirubin - absent; stercobilin - present. Microscopic examination: muscle fibers without striations - in small quantities; muscle fibers with striations - in small quantities; indigestible plant fiber - in small quantities; digestible plant fiber - in large quantities; neutral fat - in small quantities; fatty acids - in small quantities; soap - in small quantities; starch - in large quantities; iodophilic flora - in large quantities; mucus - in small quantities. |
| dysentery, ulcerative colitis | Macroscopic examination: consistency - mushy or liquid; color - dark brown or creamy; the smell is not strong. Chemical research: pH >7.5; protein - yes; bilirubin - absent; stercobilin - present. Microscopic examination: muscle fibers without striations - in small quantities; muscle fibers with striations - in small quantities; indigestible plant fiber - in small quantities; digestible plant fiber - in small quantities; soap - in small quantities; mucus - in small quantities; in mucus - erythrocytes, leukocytes. |
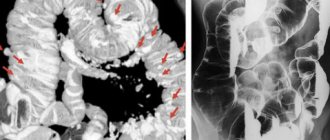
A general stool analysis (coprogram) is an auxiliary study. The study is most often indicative in nature; if a digestive disorder is suspected, additional laboratory tests (biochemical, serological, bacteriological) and instrumental studies (fibrogastroscopy, colonoscopy, ultrasound of the abdominal organs, etc.) should be carried out.
Bacteriology
To obtain a reliable result, material for research is taken before the start of antibacterial therapy or in the intervals between courses of treatment, but not earlier than 2 weeks after its completion.
- 3-4 days before the study, it is necessary to stop taking laxatives, castor and petroleum jelly and stop administering rectal suppositories.
Attention: Feces obtained after an enema, as well as after taking barium (during an X-ray examination), are not suitable for research.
Collection rules
- Feces should be collected in the morning, on an empty stomach.
- Carry out hygiene procedures and first urinate in the toilet and flush.
- Place sterile paper (or an ironed sheet) or a disposable plastic plate in the bowl or bottom of the toilet and perform a bowel movement.
- Collect feces immediately after defecation from different places in a single portion with a special spoon mounted in the lid of a plastic container in a volume of 1–2 g (no more than 1/3 of the container’s volume). Avoid contact with urine and pieces of undigested food.
- Deliver to the laboratory on the day of collection.
Decoding the results of scatological research
When the results are ready, the person will receive a form indicating normal indicators and the results obtained from the study of the material. It is better to consult a doctor for a decoding, since even a deviation from the norm of several indicators does not always indicate the presence of pathologies.
Normally, an adult's feces should be uniformly brown in color, dense, and have a characteristic odor.
The feces of a healthy person are free of foreign impurities, food debris, protozoa and parasite eggs. The presence of undigested fiber in the stool indicates low acidity of gastric juice, the presence of blood and pus indicates serious gastrointestinal pathologies.
PCR studies
Collection rules
- Feces should be collected in the morning, on an empty stomach.
- Carry out hygiene procedures and first urinate in the toilet and flush.
- Place sterile paper (or an ironed sheet) or a disposable plastic plate in the bowl or bottom of the toilet and perform a bowel movement.
- Collect feces immediately after defecation from different places in a single portion with a special spoon mounted in the lid of a plastic container in a volume of 1–2 g (no more than 1/3 of the container’s volume). Avoid contact with urine and pieces of undigested food.
- Deliver to the laboratory on the day of collection.
general characteristics
Coprogram - analysis of the physical, chemical and microscopic characteristics of feces. The method is an important diagnostic component for identifying dysfunctions of the stomach, intestines, pancreas, and liver. Macroscopic examination of feces includes the study of physical characteristics: quantity, consistency, color, smell, presence of impurities. During microscopic examination of stool, native and colored preparations are examined. The method is used at the diagnostic stage and to monitor the effectiveness of treatment.
Culture for microflora and sensitivity to antibiotics
3-4 days before the study, it is necessary to stop taking laxatives, castor and vaseline oil, and stop administering rectal suppositories. Feces obtained after an enema, as well as after taking barium (during X-ray examination) are not accepted for examination!
Attention: Feces are collected before starting treatment with antibacterial and chemotherapy drugs.
Collection rules
- First urinate in the toilet and flush.
- Place sterile paper (or an ironed sheet) or a disposable plastic plate in the bowl or bottom of the toilet and perform a bowel movement.
- Collect feces immediately after defecation from different places in a single portion with a special spoon mounted in the lid of a plastic container in a volume of 1–2 g (no more than 1/3 of the container’s volume). Avoid contact with urine and pieces of undigested food.
- Deliver to the laboratory on the day of collection. If it is impossible to quickly deliver the sample to the laboratory, you can store it in the refrigerator for no more than 4 hours at 2-8 °C.
Chemical research
Fecal reaction
An acidic reaction (pH 5.0-6.5) is observed when iodophilic flora is activated, producing carbon dioxide and organic acids (fermentative dyspepsia). An alkaline reaction (pH 8.0-10.0) occurs with insufficient digestion of food, with colitis with constipation, sharply alkaline with putrefactive and fermentative dyspepsia.
Reaction to blood (Gregersen reaction)
A positive reaction to blood indicates bleeding in any part of the gastrointestinal tract (bleeding from the gums, rupture of varicose veins of the esophagus, erosive and ulcerative lesions of the gastrointestinal tract, tumors of any part of the gastrointestinal tract in the stage of decay).
Reaction to stercobilin
The absence or sharp decrease in the amount of stercobilin in the feces (the reaction to stercobilin is negative) indicates obstruction of the common bile duct with a stone, compression by a tumor, stricture, stenosis of the common bile duct, or a sharp decrease in liver function (for example, in acute viral hepatitis). An increase in the amount of stercobilin in feces occurs with massive hemolysis of red blood cells (hemolytic jaundice) or increased bile secretion.
Reaction to bilirubin
The detection of unchanged bilirubin in the stool of an adult indicates a disruption in the process of bilirubin recovery in the intestine under the influence of microbial flora. Bilirubin can appear during rapid evacuation of food (sharp increase in intestinal motility), severe dysbiosis (syndrome of bacterial overgrowth in the colon) after taking antibacterial drugs.
Vishnyakov-Triboulet reaction (for soluble protein)
The Vishnyakov-Triboulet reaction is used to identify a hidden inflammatory process. The detection of soluble protein in stool indicates inflammation of the intestinal mucosa (ulcerative colitis, Crohn's disease).
For carbohydrates
- Carry out hygiene procedures and first urinate in the toilet and flush.
- Place sterile paper (or an ironed sheet) or a disposable plastic plate in the bowl or bottom of the toilet and perform a bowel movement.
- Collect feces immediately after defecation from different places in a single portion with a special spoon mounted in the lid of a plastic container in a volume of 1–2 g (no more than 1/3 of the container’s volume). Avoid contact with urine and pieces of undigested food.
- Deliver the sample to the laboratory within 4 hours.
Attention Storing a stool sample for more than 4 hours, including in the refrigerator, is not allowed.