Prednisolone ()
There may be pharmaceutical incompatibility of prednisolone with other intravenously administered drugs - it is recommended to administer it separately from other drugs (intravenous bolus (bolus), or through another dropper, as a second solution).
When mixing a solution of prednisolone with heparin, a precipitate forms.
Concomitant use of prednisolone with:
- inducers of microsomal liver enzymes (phenobarbital, rifampicin, phenytoin, theophylline, ephedrine) leads to a decrease in its concentration;
- diuretics (especially thiazide and carbonic anhydrase inhibitors) and amphotericin B can lead to increased excretion of potassium from the body and an increased risk of developing heart failure;
- sodium-containing drugs can lead to the development of edema and increased blood pressure;
- cardiac glycosides - their tolerability worsens and the likelihood of developing ventricular extrasystole increases (due to hypokalemia);
- indirect anticoagulants - weakens (less often enhances) their effect (dose adjustment required);
- anticoagulants and thrombolytics - increases the risk of bleeding from ulcers in the gastrointestinal tract;
- ethanol and nonsteroidal anti-inflammatory drugs (NSAIDs) - increases the risk of erosive and ulcerative lesions of the gastrointestinal tract and the development of bleeding (in combination with NSAIDs in the treatment of arthritis, it is possible to reduce the dose of GCS due to the summation of the therapeutic effect);
- paracetamol - the risk of developing hepatotoxicity increases (induction of liver enzymes and the formation of a toxic metabolite of paracetamol);
— acetylsalicylic acid — accelerates its elimination and reduces its concentration in the blood (when prednisolone is discontinued, the concentration of salicylates in the blood increases and the risk of side effects increases);
- insulin and oral hypoglycemic drugs, antihypertensive drugs - their effectiveness decreases;
- vitamin D - its effect on calcium absorption in the intestine is reduced;
- growth hormone - reduces its effectiveness, and with praziquantel - its concentration in the blood;
- m-anticholinergic blockers (including antihistamines and tricyclic antidepressants) and nitrates - helps to increase intraocular pressure;
- tricyclic antidepressants - may increase the severity of depression caused by taking corticosteroids (not indicated for the treatment of these side effects);
- isoniazid and mexiletine - increases their metabolism (especially in “slow” acetylators), which leads to a decrease in their plasma concentrations.
Carbonic anhydrase inhibitors and loop diuretics may increase the risk of osteoporosis.
Indomethacin, displacing prednisolone from its connection with albumin, increases the risk of developing its side effects.
ACTH enhances the effect of prednisolone.
Ergocalciferol and parathyroid hormone prevent the development of osteopathy caused by prednisolone.
Cyclosporine and ketoconazole, by slowing down the metabolism of prednisolone, can in some cases increase its toxicity.
The simultaneous use of androgens and steroidal anabolic drugs with prednisone contributes to the development of peripheral edema and hirsutism, and the appearance of acne.
Estrogens and oral estrogen-containing contraceptives reduce the clearance of prednisolone, which may be accompanied by an increase in the severity of its action.
When used simultaneously with live antiviral vaccines and against the background of other types of immunization, the risk of viral activation and the development of infections increases.
Antipsychotics (neuroleptics) and azathioprine increase the risk of developing cataracts when prednisolone is prescribed.
When used simultaneously with antithyroid drugs, the clearance of prednisolone decreases and with thyroid hormones increases.
Hypokalemia caused by GCS can increase the severity and duration of muscle blockade due to muscle relaxants.
Mitotane and other inhibitors of adrenal function may necessitate an increase in the dose of prednisolone.
Immunosuppressants increase the risk of developing infections and lymphoma or other lymphoproliferative disorders caused by the Epstein-Barr virus.
Concomitant use of prednisolone with sulypopride increases the risk of arrhythmia.
Concomitant use of prednisolone with antihypertensive drugs may cause a decrease in the hypotensive effect due to sodium and water retention.
The simultaneous use of prednisolone with fluoroquinolones increases the risk of developing tendinitis, and in rare cases can lead to tendon rupture.
Compound
Composition of Prednisolone in ampoules: active substance at a concentration of 30 mg/ml, as well as sodium pyrosulfate (additive E223), disodium edetate, nicotinamide, sodium hydroxide, water for injection.
Composition of Prednisolone tablets: 1 or 5 mg of active substance, colloidal silicon dioxide, magnesium stearate, stearic acid, starch (potato and corn), talc, lactose monohydrate.
Prednisolone ointment contains 0.05 g of active substance, soft white paraffin, glycerin, stearic acid, methyl and propyl parahydroxybenzoate, Cremophor A25 and A6, purified water.
Pharmacodynamics and pharmacokinetics
Pharmacodynamics. Prednisolone - what is it?
The mechanism of action of Prednisolone is associated with its ability to interact with certain intracellular (cytoplasmic) receptors. These receptors are found in all tissues of the body, but most of them are in the liver.
As a result of this interaction, complexes inducing the synthesis of proteins (including enzymes that regulate vital intracellular processes) are formed.
Acts at all stages of development of the inflammatory process: suppresses the synthesis of Pg at the level of arachidonic acid, and also prevents the formation of pro-inflammatory cytokines - IFN-β and IFN-γ, IL-1, TNF, neopterin; increases the resistance of plasma membranes to damaging factors.
It affects the metabolism of lipids and proteins, and also, to a slightly lesser extent, the exchange of water and electrolytes.
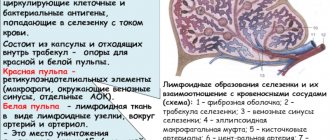
The immunosuppressive effect is realized due to the ability of the drug to cause involution of lymphoid tissue , inhibit the proliferation of lymphocytes , migration of B cells, and the interaction of B and T lymphocytes , inhibit the release of IFN-γ, IL-1 and IL-2 from macrophages and lymphocytes , reduce the formation antibodies .
Inhibition of the allergic reaction is carried out by reducing the secretion and synthesis of allergic , reducing the number of circulating basophilic leukocytes , suppressing the release of histamine from sensitized mast cells and basophilic leukocytes , suppressing the development of connective and lymphoid tissue , reducing the number of mast cells, B- and T-lymphocytes , reducing allergy mediators , suppression of antibody , changes in the immune response.
Inhibits the synthesis and secretion of corticotropin and, secondarily, endogenous corticosteroids.
When applied externally, it relieves inflammation, inhibits the development of an allergic reaction , relieves itching and inflammation, reduces exudation , and suppresses the activity of the immune system in relation to type III-IV hypersensitivity reactions.
Pharmacokinetics
After taking the tablet, it is quickly and completely absorbed from the gastrointestinal tract. TSmax - from 60 to 90 minutes. Up to 90% of the administered dose of prednisolone is bound to plasma proteins.
The substance undergoes biotransformation in the liver. From 80 to 90% of metabolic products are excreted in urine and bile, about 20% of the dose is eliminated in its pure form. T1/2 - from 2 to 4 hours.
Contraindications
If systemic use of the drug is necessary for health reasons, the only contraindication may be intolerance to one or more of its constituent components.
Other contraindications to the use of solution and tablets are:
- infectious and parasitic diseases caused by bacteria, fungi or viruses (including those recently transmitted by a person, including contact with a sick person). Such diseases include: herpes virus infection , measles , strongyloidiasis (or suspicion of it), amoebiasis , tuberculosis (active or latent), systemic mycosis .
- Diseases of the digestive tract ( peptic ulcer of the duodenum/stomach , peptic ulcer , ulcerative colitis with threat of abscessation or perforation, recently performed anastomosis of the intestinal tube , diverticulitis ).
- Cardiovascular pathologies , including recent myocardial infarction (in patients with acute/subacute myocardial infarction, the use of Prednisolone can provoke the spread of a necrotic lesion and slow down the formation of scar tissue, which in turn increases the risk of rupture of the heart muscle), decompensated CHF , arterial hypertension .
- Hyperlipidemia.
- Immunodeficiency conditions (including HIV infection , AIDS ).
- Post-vaccination period (the drug is not prescribed during the period of 8 weeks before and 2 weeks after the vaccine).
- Lymphadenitis developed after BCG vaccination .
- Diseases of the endocrine system : Itsenko-Cushing's disease , hyper- or hypothyroidism , diabetes mellitus .
- Severe degree of functional kidney/liver failure.
- Urolithiasis disease.
- Hypoalbuminemia , as well as conditions predisposing to its development.
- Systemic osteoporosis.
- Acute psychosis.
- Myasthenia gravis.
- III-IV stages of obesity.
- Closed and open angle glaucoma.
- Poliomyelitis (with the exception of the form of bulbar encephalitis).
- Lactation.
- Pregnancy.
For patients with severe infectious diseases, Prednisolone tablets and injections are prescribed only against the background of specific therapy.
Contraindications to intra-articular administration of the drug are:
- pathological bleeding (due to the use of anticoagulants or endogenous );
- pyogenic arthritis and periarticular infections (including a history);
- transarticular bone fracture;
- systemic infections;
- “dry” joint (no signs of inflammation in the joint: for example, with osteoarthritis without signs of inflammation of the synovial membrane );
- severe joint deformity , bone destruction or periarticular osteoporosis ;
- developed due to arthritis ;
- aseptic necrosis of the epiphyses of the bones that form the joint;
- pregnancy.
On the skin Prednisolone should not be used for:
- mycoses, viral and bacterial skin lesions;
- skin manifestations of syphilis ;
- skin tumors;
- tuberculosis;
- acne (in particular, with rosacea and acne vulgaris);
- pregnancy.
Eye drops are not prescribed to patients with fungal and viral eye infections , impaired integrity of the corneal epithelium, trachoma , acute purulent and viral conjunctivitis , purulent infection of the eyelids and mucous membrane , purulent corneal ulcer , eye tuberculosis , as well as for conditions that developed after removal of a foreign object from the cornea of the eye.
Instructions for use of Prednisolone (Method and dosage)
Instructions for the use of Prednisolone in injections
The solution is administered intravenously, intramuscularly and intraarticularly.
The method of administration and dosage of Prednisolone ( Prednisolone Nycomed , Prednisolone hemisuccinate ) are selected individually by the attending physician, taking into account the type of pathology, the severity of the patient’s condition, and the location of the affected organ.
In severe and life-threatening conditions, the patient is prescribed pulse therapy using ultra-high doses for a short period of time. For 3-5 days, he is given 1-2 g of prednisolone daily by intravenous drip infusion. The duration of the procedure is from 30 minutes to 1 hour.
During treatment, the dosage is adjusted depending on the patient's response to therapy.
It is considered optimal to administer Prednisolone intravenously. For intra-articular administration, ampoules with Prednisolone are used only in cases where the tissue inside the joint is affected by the pathological process.
Positive dynamics are a reason to transfer the patient to tablets or suppositories with prednisolone. Treatment with tablets is continued until stable remission develops.
If it is not possible to administer Prednisolone intravenously, the medicine should be injected deep into the muscle. However, it should be borne in mind that with this method it is absorbed more slowly.
In the human body, the release of adrenal hormones into the bloodstream occurs between 6 and 8:00 am, so injections should also be given at this time. The entire daily dose is usually administered at once. If this is not possible, at least ⅔ of the prescribed dose is administered in the morning, the remaining third should be administered at lunchtime (at approximately 12:00).
Depending on the pathology, the dose can range from 30-1200 mg/day. (with its subsequent decrease).
Children aged from two months to 1 year are administered from 2 to 3 mg/kg. Dosage for children from one to 14 years of age is 1-2 mg/kg (as a slow, 3-minute intramuscular injection). If necessary, after 20-30 minutes the medicine is re-administered in the same dose.
If a large joint is affected, 25 to 50 mg of prednisolone is injected into it. From 10 to 25 mg is injected into medium-sized joints, and from 5 to 10 mg into small joints.
Prednisolone tablets: instructions for use
The patient is transferred to taking tablets, following the principle of gradual withdrawal of GCS.
If HRT is used, the patient is prescribed 20 to 30 mg of prednisolone per day. Maintenance dose - from 5 to 10 mg/day. For some pathologies - for example, with nephrotic
syndrome - it is advisable to prescribe higher doses.
For children, the starting dose is 1-2 mg/kg/day. (it should be divided into 4-6 doses), maintenance - from 0.3 to 0.6 mg/kg/day. When prescribing, take into account the daily secretory rhythm of endogenous steroid hormones .
Recommendations regarding the use of drugs from different manufacturers are the same. That is, the instructions for Nycomed tablets do not differ from the instructions for tablets produced by.
Prednisolone ointment: instructions for use
The ointment is a means of external therapy. It should be applied to the affected areas of the skin in a thin layer from 1 to 3 times a day. An occlusive dressing can be applied to limited pathological lesions to enhance the effect.
When used in children over one year of age, the drug should be used for the shortest possible course. You should also exclude measures that enhance the absorption and resorption of prednisolone (occlusive, fixing, warming dressings).
Eye drops: instructions for use
Instillations of the drug are carried out 3 times a day, instilling 1-2 drops of solution into the conjunctival cavity of the affected eye. In the acute phase of the disease, the instillation procedure can be repeated every 2-4 hours.
For patients who have undergone ophthalmic surgery, drops are prescribed 3-5 days after surgery.
How long can you take Prednisolone?
Glucocorticosteroid therapy is aimed at achieving maximum effect with the lowest possible doses.
The duration of treatment depends on the patient's diagnosis and individual response to treatment. In some cases, the course lasts up to 6 days; with HRT it lasts for months. The duration of external therapy using Prednisolone ointment is usually from 6 to 14 days.
Dosage for animals
The dosage for dogs and cats is selected individually depending on the indications.
So, for example, with infectious peritonitis, a cat should be given orally 1 r./day. 2-4 mg/kg of prednisolone, for chronic panleukopenia - 2 times/day. 2.5 mg each.
The standard dosage for a dog is 1 mg/kg 2 times a day. Treatment lasts 14 days. Upon completion of the course, you must take tests and be examined by a doctor. When discontinuing the drug, the dose for dogs should be reduced by 25% every 14 days.
What is hormone therapy?
Hormones are biologically active substances produced by the body that control cell growth. Some organs in our body require sex hormones, such as estrogen and testosterone, to function and develop properly. In addition, there are thyroid hormones, as well as the insulin hormone, which have different functions. The development of some types of cancer can also be caused by the action of hormones. Therefore, in their treatment, drugs are used that disrupt, block and stop their work. This type of treatment is called "hormone therapy."
pharmachologic effect
Pharmacological group: Corticosteroids (drug group - I, this means that prednisolone is a weakly active GCS).
Prednisolone - hormonal or not?
Prednisolone is a hormonal drug for local and systemic use with an average duration of action.
It is a dehydrated analogue of the hormone hydrocortisone . Its activity is four times higher than the activity of hydrocortisone.
Prevents the development of an allergic reaction (if the reaction has already begun, it stops it), suppresses the activity of the immune system , relieves inflammation, increases the sensitivity of β2-adrenergic receptors to endogenous catecholamines, and has an anti-shock effect.
special instructions
Treatment with Prednisolone should be stopped slowly, gradually reducing the dose.
For patients with a history of psychosis , high doses are allowed to be prescribed only under the strict supervision of a physician.
How to “get off” Prednisolone?
Treatment with Prednisolone should be discontinued gradually. Dose reduction is carried out by weekly reducing the dose used by ⅛ or taking the last dose every other day and reducing it by ⅕ (this method is faster).
With the fast method, on a day without Prednisolone, the patient is shown stimulation of the adrenal glands using UHF or DQV on their projection, taking ascorbic acid (500 mg/day), administering insulin in increasing doses (starting - 4 units, then for each dose it is increased by 2 units; highest dose - 16 units).
Insulin should be injected before breakfast, and the person should remain under observation for 6 hours after the injection.
If Prednisolone is prescribed for bronchial asthma , it is recommended to switch to inhaled steroids . If the indication for use is an autoimmune disease , use mild cytostatics .
Features of the diet when taking Prednisolone
When taking Prednisolone, it is recommended to exclude fried and spicy foods from the diet, as well as fruits and sour juices, which stimulate the secretion of hydrochloric acid.
In addition, it is necessary to limit the amount of high-calorie foods high in carbohydrates and fats (their consumption during GCS therapy increases blood glucose levels and rapid weight gain), table salt and liquid.
When preparing food, you need to use products that contain potassium salts, calcium and protein (dietary meats, dairy products, fruits, hard cheeses, baked potatoes, prunes, apricots, nuts, zucchini, etc.).