Pharmacological properties of the drug Temodal
Pharmacodynamics. Temodal (temozolomide) is an imidazotetrazine alkylating agent with antitumor activity. When entering the systemic circulation (at physiological pH values), it undergoes rapid chemical transformation with the formation of the active compound - monomethyltriazenoimidazolecarboxamide (MTIC). It is believed that the cytotoxicity of the latter is mainly due to alkylation of guanine at the O6 position and additional alkylation at the N7 position. Cytotoxic damage that subsequently develops most likely triggers a mechanism for aberrant reduction of the methyl residue. Pharmacokinetics. Temozolomide is rapidly absorbed after oral administration and is excreted from the body in the urine. Quickly penetrates the BBB and enters the CSF. The maximum concentration in blood plasma is achieved on average 0.5–1.5 hours (as early as 20 minutes) after taking the drug. The plasma half-life is approximately 1.8 hours. Clearance, volume of distribution and half-life are independent of dose. Temozolomide is weakly bound to plasma proteins (10–20%), and therefore interaction of the drug with compounds that are significantly bound to plasma proteins should not be expected. After oral administration, the average excretion rate of 14C-labeled temozolomide in feces over 7 days was 0.8%, indicating complete absorption. The main route of elimination of temozolomide is through the kidneys. 24 hours after oral administration, approximately 5-10% of the dose taken is excreted unchanged in the urine, the rest is excreted as the acid form of temozolomide - 5-aminoimidazole-4-carboxamide and unidentified polar metabolites. Pharmacokinetic analysis showed that plasma clearance of temozolomide was independent of age, renal function, or smoking. In a separate pharmacokinetic study, the pharmacokinetic profile of the drug in patients with mild or moderate hepatic impairment was found to be similar to that in individuals with normal hepatic function. In children, the AUC is higher than in adults, but the maximum tolerated dose in children and adults is the same and is 1000 mg/m2 per treatment cycle.
Use of the drug Temodal
Therapy with Temodal should be carried out by a physician with experience in the treatment of such malignant diseases. Adult patients with newly diagnosed glioblastoma multiforme Treatment phase with Temodal accompanied by radiotherapy. Temodal is administered orally at a dose of 75 mg/m2 every day for 42 days simultaneously with radiotherapy (60 Gy in 30 fractions) followed by a course of adjuvant treatment for 6 cycles. Dose reduction is not recommended; however, interruptions in dosing are possible depending on the patient's tolerance to therapy. At this dose, the use of Temodal can be extended from 42 days of accompanying therapy to 49 days if all of the following conditions are present: absolute neutrophil count 1.5•109/l; platelet count ≥100•109/l; overall toxicity criteria (OTC) non-hematological toxicity ≤grade 1 (excluding alopecia, nausea and vomiting). Dose adjustment. During treatment, a complete complete blood count should be performed weekly. The use of Temodal should be interrupted or stopped completely during the accompanying phase, taking into account the criteria for hematological and non-hematological toxicity in accordance with Table 1. Table 1 Interruption or discontinuation of Temodal use during accompanying therapy (Temodal + radiotherapy)
Toxicity | Interruption* of Temodal use | Stop using Temodal |
| Absolute neutrophil count | ≥0.5 and ≤1.5•109/l | ≤0.5•109/l |
| Platelet count | ≥10 and ≤100•109/l | ≤ 10•109/l |
| OT - non-hematological toxicity (except alopecia, nausea and vomiting) | Degree 2 | Grade 3 or 4 |
*The use of Temodal is resumed in the presence of all the following conditions: absolute neutrophil count ≥1.5•109/l; platelet count ≥100•109l; CAT - non-hematological toxicity ≤1st grade (excluding alopecia, nausea and vomiting).
Adjuvant phase 4 weeks after completion of the Temodal + radiotherapy treatment phase, Temodal is prescribed for 6 additional cycles of adjuvant therapy. The dose during Cycle 1 (adjuvant cycle) is 150 mg/m2 once a day for five days of a 28-day cycle (5 days with Temodal, 23 days without Temodal). The dose of Temodal for Cycle 2 is increased to 200 mg/m2/day if CAT - non-hematological toxicity during Cycle 1 was ≤grade 2 (excluding alopecia, nausea and vomiting), absolute neutrophil count ≥1.5•109/l , platelet count ≥100•109/l. If the dose increase does not occur in cycle 2, the dose is also not increased in subsequent cycles. The dose of 200 mg/m2/day for the first 5 days of each subsequent cycle remains, except in cases of toxicity. In each cycle, Temodal is taken for 5 consecutive days, followed by a 23-day break. Dose reduction or discontinuation of Temodal during adjuvant therapy should be carried out according to Table. 2 and 3. During treatment, a complete complete blood count should be performed on day 22 (21 days after the first dose). Table 2 Temodal dose levels for adjuvant therapy
Dose level | Dose, mg/m2/day | Note |
| –1 | 100 | Reduced with previous toxicity |
| 0 | 150 | Dose during cycle 1 |
| 1 | 200 | Dose during cycles 2–6 if no toxicity |
Table 3 Dose reduction or discontinuation of Temodal during adjuvant therapy
Toxicity | Reduce Temodal dose by 1 level* | Stop using Temodal |
| Absolute neutrophil count | ≤1.0•109/l | b |
| Platelet count | ≤50•109/l | b |
| OT - non-hematological toxicity (except alopecia, nausea and vomiting) | Degree 3 | Degree 4 |
*Temodal dose levels indicated in the table; b - Temodal is discontinued if a dose reduction to ≤100 mg/m2/day is required or if grade 3 non-hematological toxicity (excluding alopecia, nausea and vomiting) remains after dose reduction.
Adult patients with relapse or progression of glioma or malignant melanoma. For patients who have not previously received chemotherapy, Temodal is prescribed orally at a dose of 200 mg/m2 once a day for 5 days of a 28-day cycle. For patients who have previously been treated with chemotherapy, the initial dose is 150 mg/m2 once daily; in the second cycle, the dose can be increased to 200 mg/m2 per day if on the first day of this cycle the absolute neutrophil count is ≥1.5•109/l and the platelet count is ≥100•109/l. Pediatric patients with relapse or progression of glioma. For children over 3 years of age, Temodal is prescribed orally at a dose of 200 mg/m2 once a day for 5 days of a 28-day cycle. For children who have previously received chemotherapy, the initial dose is 150 mg/m2 once daily for five days, increasing to 200 mg/m2 per day during the subsequent cycle if no signs of toxicity are observed. Laboratory values for dosing modification for relapse or progression of glioma or malignant melanoma. Before starting to use the drug, the following laboratory values should be available: absolute neutrophil count ≥1.5•109/l, platelet count ≥100•109/l. A full blood count should be performed on day 22 (day 21 after the first dose) or within 48 hours thereafter and weekly thereafter until the absolute neutrophil count is greater than 1.5 x 109L. and the platelet count will not exceed 100•109/l. If the absolute neutrophil count is ≤1.0•109/L or if the platelet count is ≤50•109/L during any cycle, the dose in the subsequent cycle should be lower by one level. Possible dose levels per day: 100 mg/m2, 150 mg/m2 and 200 mg/m2. The minimum recommended dose is 100 mg/m2/day. The duration of treatment is a maximum of 2 years. If signs of disease progression appear, treatment with Temodal should be discontinued. Temodal should be taken on an empty stomach at least one hour before meals. The prescribed dose should be administered using the minimum number of capsules possible. Temodal capsules are swallowed whole with a glass of water; Capsules should not be opened or chewed. If the capsule is damaged, contact of its contents with the skin or mucous membranes should be avoided. If the powder gets on the skin or mucous membranes, rinse the area with water. Capsules should be stored in the original bottle in a dry place.
Use of the parenteral form of the drug Temodal® (temozolomide) in the treatment of glioblastomas
The article uses a specific example to examine the effectiveness of temozolomide, prescribed at an early stage in the diagnosis of glioblastoma. Chemoradiation therapy with temozolomide followed by single-agent chemotherapy with parenteral Temodal (temozolomide) has been shown to be well tolerated, significantly improve progression-free survival and overall survival compared with other treatment regimens, and are the gold standard first-line therapy in patients with glioblastoma.
Rice. 1. MRI results: the effectiveness of chemoradiotherapy in a patient with glioblastoma (A – after surgery, B – after radiation therapy and six courses of monochemotherapy)
Rice. 2. MRI results: the effectiveness of chemoradiotherapy in a patient with glioblastoma (A – after surgery, B – after radiation therapy and temozolomide monochemotherapy, C – after six courses of monochemotherapy)
Introduction
Malignant gliomas account for 50–60% of all primary tumors of the central nervous system. The prognosis for their treatment is unfavorable, and the quality of life of patients is reduced due to severe neurological disorders and complications associated with the therapy used. The treatment algorithm involves surgical resection followed by radiation therapy and chemotherapy [1]. For glial tumors, antitumor drugs are used: temozolomide, nitroso derivatives (lomustine, nimustine, carmustine, fotemustine), vincristine, procarbazine, the combination of “lomustine + procarbazine + vincristine,” platinum derivatives (cisplatin, carboplatin), etoposide, bevacizumab (in monotherapy or in combination with irinotecan). Temozolomide is recognized as the most effective drug in the treatment of malignant gliomas [2].
Temozolomide is an alkylating drug, the mechanism of action of which is the addition of a methyl group to DNA, which leads to disruption of the structure of the latter and cell death [3]. Oral temozolomide has 100% bioavailability and rapid and complete absorption in the intestine.
It should be noted that the drug is included in the standards for the treatment of malignant gliomas in Russia and is available to patients. In the treatment of malignant gliomas, temozolomide is prescribed at a dose of 150–200 mg/m2 for five days every 28 days [4]. Long-term use of temozolomide during the entire course of radiotherapy leads to depletion of methylguanine methyltransferase (MGMT), an enzyme that ensures cellular DNA repair and affects the prognosis of the effectiveness of chemotherapy, even in the absence of MGMT methylation, which gives hope for treatment success [5, 6].
Today, the standard of treatment for patients with glioblastoma as the first line after removal or biopsy (after histological verification of the tumor) is considered to be combined chemoradiotherapy using temozolomide (daily administration during radiation therapy followed by maintenance courses of chemotherapy with this drug) [2]. The addition of temozolomide to radiation therapy early in the treatment of glioblastomas provides a statistically significant increase in overall survival and time to progression [3]. The results of clinical studies showed that all patients receiving temozolomide in both dosage forms noted better tolerability of intravenous infusion compared to oral capsules. The presence of two dosage forms expands the possibilities of using temozolomide for malignant gliomas, allows treatment with the least toxicity and ensures the highest quality of life for patients during treatment [4].
Clinical case 1
Woman, 40 years old. She became acutely ill in July 2015 and had an attack with loss of consciousness. The patient was taken to the clinic by an ambulance. A computed tomography (CT) scan of the brain revealed a tumor of the head of the caudate nucleus with damage to the corpus callosum and paraventricular parts of the frontal lobe on the right. On July 13, an operation was performed to remove tumors of the cerebral hemispheres using neurosurgical techniques under navigation control. Histologically – G4 glioblastoma. After surgery, there was a slight neurological deficit due to numbness in the left upper limb. The results of magnetic resonance imaging (MRI) of the brain, performed on July 30, showed the presence of a tumor of the right temporofrontal region with spread to the basal ganglia of the brain on the right and the anterior parts of the corpus callosum, and a postoperative porencephalic cyst of the right temporofrontal region. She was prescribed chemoradiotherapy, followed by six courses of temozolomide monochemotherapy. Taking into account the presence of periodic dizziness, nausea and vomiting after meals in the postoperative period, the parenteral form of the drug Temodal® was chosen. Radiation therapy began 25 days after surgery. 3D planning was performed on an Amphora 2.13 planning system using CT topometry and T1 MRI scan fusion to visualize residual tumor. The entire volume of the brain was irradiated (dose 30 Gy), then the residual tumor with a safety margin of 1–2 cm was exposed to reduced fields (total dose up to 60 Gy). Treatment was carried out in the standard fractionation mode on the gamma therapeutic device AGAT-R1. Simultaneously with radiation therapy (30 fractions in a total dose of 60 Gy), the patient received temozolomide at a dose of 75 mg/m2 daily intravenously for 42 days. During treatment, weekly blood tests were performed with cell counts. No hematological toxicity was recorded throughout the entire period of chemoradiation treatment. No dose reduction or temporary discontinuation of the drug was required. Four weeks after the completion of combination therapy, six courses of temozolomide monochemotherapy were completed. During the first course, the drug was prescribed at a dose of 150 mg/m2 intravenously for five days, followed by a 23-day break. Taking into account the fact that no hematological or non-hematological toxicity was recorded in the first cycle, in the second cycle the dose was increased to 200 mg/m2 intravenously. The same daily dose of the drug was prescribed in subsequent cycles. In each cycle, the patient took the drug for five consecutive days, followed by a 23-day break. No neurological deficits were observed during treatment. Control MRI of the brain showed a significant reduction in the size of the area of pathological accumulation of contrast and the area of perifocal edema (Fig. 1).
Situation as of March 2021: the patient is alive, continues to work and lead an active lifestyle, neurological symptoms are completely relieved. No hematological or non-hematological toxicity was recorded throughout the entire treatment period. It is planned to continue monochemotherapy with parenteral temozolomide until the disease progresses, assessing the effect (MRI of the brain) every three months.
Clinical case 2
Male, 39 years old. He became acutely ill; at the end of March 2015, severe headaches, weakness in the right limbs, and slow speech appeared. The patient was taken to the clinic by an ambulance team. A CT scan of the brain revealed a mass formation in the left frontal lobe of the brain. On April 13, an operation was performed - microsurgical removal of the tumor of the left frontal lobe and insula using intraoperative navigation. Histologically – G4 glioblastoma. After the operation, neurological deficits in the form of right-sided hemiparesis and speech impairment were observed. A control MRI of the brain, performed on April 28, showed the condition after subtotal removal of a tumor in the frontoparietal region of the brain on the left, and lateral dislocation of the median structures to the right. Radiation therapy was started 28 days after surgery. 3D planning was performed on the Amphora 2.13 planning system using CT topometry and T1 MRI scanning data fusion to visualize the residual tumor. The entire volume of the brain was exposed to irradiation (dose up to 30 Gy), then the residual tumor with a safety margin of 1–2 cm was exposed to reduced fields (total dose up to 60 Gy). Treatment was carried out in the standard fractionation mode on the gamma therapeutic device AGAT-R1. Simultaneously with radiation therapy (30 fractions in a total dose of 60 Gy), the patient received Temodal® (temozolomide) at a dose of 75 mg/m2 daily intravenously for 42 days. During treatment, weekly blood tests were performed with cell counts. No hematological toxicity was recorded throughout the entire period of chemoradiation treatment. No dose reduction or temporary discontinuation of the drug was required. Four weeks after the end of combination therapy, six courses of temozolomide monochemotherapy were administered. During the first course, the drug was prescribed at a dose of 150 mg/m2 intravenously for five days, followed by a 23-day break. Taking into account the fact that no hematological or non-hematological toxicity was observed during the first cycle, during the second cycle the dose was increased to 200 mg/m2 intravenously. The same daily dose of the drug was prescribed in subsequent cycles. In each cycle, the patient took the drug for five consecutive days followed by a 23-day break. During treatment, clinically pronounced positive dynamics and a decrease in neurological deficit were observed. Control MRI of the brain demonstrated a significant reduction in the size of the area of pathological accumulation of contrast and the area of perifocal edema (Fig. 2).
Situation as of March 2021: the patient is alive, does not work, but does all the housework, takes care of himself completely, and a slight speech impairment persists. No hematological or non-hematological toxicity was recorded throughout treatment. It is planned to continue monochemotherapy with parenteral temozolomide until the disease progresses, assessing the effect (MRI of the brain) every three months.
Discussion
The clinical cases reviewed illustrate the potential beneficial effect of temozolomide prescribed in the early stages of glioblastoma diagnosis in conjunction with radiation therapy, as well as in the form of adjuvant monochemotherapy. Both patients continue to receive parenteral temozolomide with partial remission observed.
This treatment regimen allows not only to increase the median overall survival, but also to significantly extend the time to progression and preserve the quality of life and social status of patients.
The low toxicity of the drug Temodal® (temozolomide) when administered intravenously allows us to recommend infusions in a day hospital or on an outpatient basis. With adjuvant chemotherapy, the risk of undesirable non-hematological effects is higher, and therefore the indications for intravenous administration of temozolomide are expanded: impaired swallowing, difficulty swallowing capsules, severe nausea and vomiting when previously taking capsules, chronic diseases of the gastrointestinal tract. Thus, the presence of two dosage forms expands the possibilities of using temozolomide in malignant gliomas [4].
When choosing and conducting therapy for glioblastomas with G4 differentiation, it should be taken into account that the disease is incurable. Median survival is usually less than a year from diagnosis. Even in the best situations, most patients die within two years. That is why the main goals of treatment are to increase the life expectancy of patients (one- and two-year survival rate), improve the quality of life (compensation for neurological deficits, prevention and treatment of treatment complications), balance the therapeutic effect (including survival) and the quality of life of patients [7].
Currently, the use of radiation therapy in combination with temozolomide is recognized as the standard of treatment for glioblastoma multiforme in most countries, including Russia. It is preferable to start chemotherapy for glioblastoma together with radiation therapy.
Against the background of radiation therapy and the use of temozolomide (75 mg/m2 daily during the entire course of radiation therapy, and then 150–200 mg/m2 for five days every 28 days), an increase in two-year survival rate for glioblastomas was observed to 27.2%, three-year survival - up to 16.7%, four-year – up to 13% (with radiation therapy without temozolomide – 11.2, 3.7 and 3.2%, respectively) [2, 7].
The ability to molecularly diagnose glial tumors makes it possible to predict the success of chemotherapy. Patients with malignant gliomas who have MGMT promoter methylation respond better to temozolomide therapy. Patients with glioblastoma treated with temozolomide along with radiation therapy had an overall survival of 21.7 months in the presence of a methylated MGMT promoter, and only 15.3 months in its absence. In chromosomal analysis, the assessment of loss of heterozygosity 1p/19q (1p/19q loss) in oligodendroglial tumors determines the success of chemotherapy using the “lomustine + procarbazine + vincristine” regimen. However, the results of a number of studies show that loss of 1p/19q heterozygosity is an indicator of less aggressive tumor. In the laboratory of our center today this is becoming a routine study with a moderate cost. Determination of the correlation of genetic aberrations in tumor tissue and in blood plasma is being studied, which makes it possible to determine treatment tactics and prognosis of the disease at the stage of preoperative examination [3, 5, 6].
The next stage in the development of drug treatment for cancer of the central nervous system will most likely be the use of combinations of modern regimens with targeted therapy. If preliminary data from ongoing studies are confirmed, it will be possible to say that patient survival in the near future will increase to 25 months when combining radiation therapy with temozolomide and bevacizumab. Further understanding of the pathogenesis of glial tumors will help to divide them into several nosoforms with different pathogenesis, but with common clinical and morphological manifestations. A clearer understanding of the mechanisms of tumor development will facilitate the targeted and precise use of targeted drugs [8, 9].
The issue of tolerability of chemotherapy treatment is also important: in the clinical cases reviewed, in the absence of hematological and non-hematological toxicity, it was possible to maintain the quality of life and social status of patients throughout the entire treatment period [7, 8].
Conclusion
Chemoradiation therapy with temozolomide followed by parenteral monochemotherapy with Temodal® (temozolomide) is well tolerated and leads to a significant increase in progression-free survival and overall survival compared with other treatment regimens. This regimen is the gold standard for first-line treatment of patients with glioblastoma and serves as the basis for the development of new highly effective treatment regimens [2, 7–9].
Side effects of the drug Temodal
In table Table 4 shows side effects (causality was not determined during the clinical trial) that occurred during the treatment of patients with newly diagnosed glioblastoma multiforme during the accompanying and adjuvant phases of treatment and required immediate treatment. The frequency distribution of side effects was made according to the following gradation: very often 10%, often 1%–≤10%, infrequently 0.1%–≤1%. Table 4
Response frequency | Temodal + radiotherapy (accompanying phase) | Temodal (adjuvant phase) | |
| Infectious manifestations | Often | Oral candidiasis | |
| Infrequently | Oral candidiasis, herpes simplex, pharyngitis, wound infection | Herpes simplex, herpes zoster, flu-like symptoms | |
| Blood and lymphatic system disorders | Often | Leukopenia, lymphopenia, Neutropenia, Thrombocytopenia | Anemia, febrile neutropenia, leukopenia, thrombocytopenia |
| Infrequently | Anemia, febrile neutropenia | Lymphopenia, petechiae | |
| Endocrine disorders | Often | ||
| Infrequently | Cushingoid | Cushingoid | |
| Metabolic and nutritional disorders | Often | Anorexia | Anorexia |
| Often | Hyperglycemia, weight loss | Reducing body weight | |
| Infrequently | Hypokalemia, increased alkaline phosphatase, weight gain | Hyperglycemia, weight gain | |
| Mental disorders | Often | Anxiety, emotional lability, insomnia | Anxiety, emotional lability, insomnia, depression |
| Infrequently | Agitation, apathy, behavioral disturbances, depression, hallucinations | Hallucinations, amnesia | |
| Nervous system disorders | Often | Headache | Headache, cramps |
| Often | Dizziness, aphasia, impaired balance and concentration, confusion, loss of consciousness, seizures, memory impairment, neuropathy, paresthesia, drowsiness, speech impairment, tremor | Dizziness, aphasia, imbalance and concentration, confusion, dysphasia, hemiparesis, memory impairment, neurological disorders, neuropathy, peripheral neuropathy, paresthesia, somnolence, speech impairment, tremor | |
| Infrequently | Ataxia, cognitive disorders, dysphasia, extrapyramidal disorders, gait disturbance, hemiparesis, hyperesthesia, hypoesthesia, neurological disorders, peripheral neuropathy, status epilepticus | Ataxia, impaired coordination and gait, hemiplegia, hyperesthesia, sensory disorders | |
| Visual disorders | Often | Blurred vision | Blurred vision, diplopia, visual field defects |
| Infrequently | Pain in the eyeballs, hemianopsia, visual disturbances, decreased visual acuity, visual field defects | Pain in the eyeballs, dry eyes, decreased visual acuity | |
| Hearing and labyrinth disorders | Often | Hearing impairment | Hearing impairment, ringing in the ears |
| Infrequently | Ear pain, hyperacusis, tinnitus, otitis media | Hearing loss, ear pain, dizziness | |
| Cardiovascular disorders | Often | Edema, swelling of the legs, hemorrhages | Leg swelling, hemorrhages, deep vein thrombosis |
| Infrequently | Palpitations, hypertension, cerebral hemorrhages | Edema, peripheral edema, pulmonary embolism | |
| Respiratory disorders | Often | Cough, shortness of breath | Cough, shortness of breath |
| Infrequently | Pneumonia, upper respiratory tract infections, nasal congestion | Pneumonia, sinusitis, upper respiratory tract infections, bronchitis | |
| Gastrointestinal disorders | Often | Constipation, nausea, vomiting | Constipation, nausea, vomiting |
| Often | Abdominal pain, diarrhea, dyspepsia, dysphagia, stomatitis | Diarrhea, dyspepsia, dysphagia, stomatitis, dry mouth | |
| Infrequently | Abdominal bloating, fecal incontinence, gastrointestinal disorders, gastroenteritis, hemorrhoids | ||
| Dermatological disorders | Often | Alopecia, rash | Alopecia, rash |
| Often | Dermatitis, dry skin, erythema, itching | Dry skin, itching | |
| Infrequently | Photosensitivity reactions, pigmentation disorders, skin peeling | Erythema, pigmentation disorder, increased sweating | |
| Musculoskeletal and connective tissue disorders | Often | Arthralgia, muscle weakness | Arthralgia, musculoskeletal pain, myalgia, muscle weakness |
| Infrequently | Back pain, musculoskeletal pain, myalgia, myopathy | Back pain, myopathy | |
| Urinary system disorder | Often | Urgency, urinary incontinence | Urinary incontinence |
| Infrequently | Dysuria | ||
| Reproductive system and breast disorders | Infrequently | Impotence | Amenorrhea, breast pain, menorrhagia, vaginal hemorrhage, vaginitis |
| Other adverse events | Often | Fatigue | Fatigue |
| Often | Fever, pain, allergic reactions, radiation damage, facial swelling, change in taste | Fever, pain, allergic reactions, radiation damage, taste changes | |
| Infrequently | Hyperemia, hot flashes, asthenia, deterioration of health, chills, change in coloration of the tongue, parosmia, thirst | Asthenia, deterioration of health, pain, chills, dental disorders, facial swelling, change in taste | |
| Laboratory research | Often | Increased ALT | Increased ALT |
| Infrequently | Increased γ-glutamyl transferase, increased liver enzymes, increased AST | ||
| Myelosuppression, neutropenia (in 8% of patients - grade 3 and 4 hematological toxicity), thrombocytopenia (in 14% of patients - grade 3 and 4 hematological toxicity) | |||
Side effects that may occur in patients with relapse or progression of glioma or malignant melanoma The most common adverse events are gastrointestinal disorders, particularly nausea (43%) and vomiting (36%). These events were usually grade 1 or 2, self-limited or easily controlled with standard use of antiemetics. The incidence of severe nausea and vomiting was 4%. Other adverse events that frequently occurred were fatigue (22%), constipation (17%), and headache (14%). Anorexia (11%), diarrhea (8%), rash, fever and drowsiness (6% each) were also reported. Less frequently (2–5% of cases) occurred (in decreasing order) asthenia, pain (including abdominal pain), dizziness, weight loss, malaise, shortness of breath, alopecia, chills, itching, dyspepsia, changes in taste, paresthesia. When treating patients with glioma and metastatic melanoma, cases of thrombocytopenia and neutropenia of the 3rd or 4th degree were observed in 19 and 17%, respectively, in the first disease and in 20 and 22%, respectively, in the second disease. When these adverse events developed, it was necessary to hospitalize patients and (or) discontinue Temodal for patients with glioma in 8 and 4% of cases, respectively, and in 3 and 1.3% for patients with melanoma. Bone marrow suppression was predictable (this phenomenon was noted usually during the first few cycles of treatment, with maximum severity observed between days 21 and 28); recovery was rapid (usually within 1–2 weeks). There were no signs of cumulative bone marrow depression. Pancytopenia, leukopenia and anemia have also been reported. Lymphopenia often developed. Opportunistic infections, including Pneumocystis carinii . Very rarely, erythema multiforme and allergic reactions, including anaphylaxis, were detected. Myelodysplastic syndrome (MDS) and secondary malignancy, including myeloid leukemia, have been very rarely reported with Temodal use. Prolonged pancytopenia, which can cause aplastic anemia, has very rarely occurred.
Temodal, 140 mg, capsules, 5 pcs.
Instructions for use
APPROVED by the Federal Committee of the Ministry of Health of the Russian Federation on October 26, 2000, pr. No. 12
Indications for use.
Temodal is indicated for the treatment of patients with glioblastoma multiforme or anaplastic astrocytoma, in the presence of relapse or progression of the disease after standard therapy. In addition, Temodal is indicated as a first-line therapeutic agent in the treatment of patients with advanced metastatic malignant melanoma. Temodal for the listed indications should be prescribed by a doctor with experience in treating such diseases.
Dosage and method of application.
Temodal capsules are intended for oral administration.
Adults:
For patients who have not previously received chemotherapy, Temodal is prescribed orally at a dose of 200 mg/m2 once a day for 5 consecutive days within a treatment cycle of 28 days. For patients who have previously undergone chemotherapy, the initial dose is 150 mg/m2 once a day; in the second cycle, the dose can be increased to 200 mg/m2 per day, provided that on the first day of the next cycle the absolute neutrophil count is not lower than 1.5·109/l and the platelet count is not lower than 100·109/l.
Children:
For children over the age of 3 years, Temodal is prescribed orally at a dose of 200 mg/m2 once a day for 5 days within a 28-day cycle. For children previously exposed to chemotherapy, the initial dose is 150 mg/m2 once a day for 5 days. From the next cycle, the dose can be increased to 200 mg/m2 if there are no signs of hematological toxicity.
Treatment is continued until the disease progresses; The duration of treatment is a maximum of 2 years.
Temodal should be taken orally on an empty stomach, at least 2 hours before meals. The prescribed dose should be taken using the minimum number of capsules possible. Capsules should not be opened or chewed but should be swallowed whole with a glass of water. If the capsule is damaged, it is necessary to avoid contact of the powdery contents of the capsule with the skin or mucous membranes. If the powder gets on the skin or mucous membranes, rinse the area with water.
Antiemetics can be taken before or after taking Temodal. If vomiting occurs after taking a single dose of Temodal, you should not repeat the drug on the same day.
Contraindications.
Temodal is contraindicated in persons with hypersensitivity to the components of the drug or to dacarbazine (DTIC). Temodal is contraindicated in patients with signs of severe myelosuppression. Temodal is contraindicated in pregnant and lactating women.
Use during pregnancy and lactation.
Temodal has not been studied in pregnant women.
Special warnings.
A prerequisite for starting the use of Temodal is to achieve the following laboratory values: absolute neutrophil count 1.5·109/l, platelet count 100·109/l. A complete clinical blood count should be performed on day 22 (21 days after the first dose), but no later than 48 hours after this day, then weekly until the absolute neutrophil count rises above 1.5 109/l and the platelet count will not exceed 100·109/l. If the absolute neutrophil count is below 1.0 109/L or the platelet count is below 50 109/L during any treatment cycle, the dose in the next cycle should be reduced by 1 step. Possible doses: 100 mg/m2, 150 mg/m2 and 200 mg/m2. The minimum recommended dose is 100 mg/m2.
Patients with severe vomiting (more than 5 attacks within 24 hours) may require antiemetic therapy before starting treatment with Temodal.
The pharmacokinetic parameters of Temodal in individuals with normal liver function and in patients with mild or moderate liver dysfunction are closely comparable. There are no data on the use of Temodal in patients with severe liver dysfunction (class III according to the Child-Pugh classification) or impaired renal function. Based on data from studying the pharmacokinetic properties of Temodal, it seems unlikely that patients, even with severe impairment of liver or kidney function, may require a dose reduction of the drug. However, caution should be exercised when prescribing Temodal to such patients.
Elderly patients (over 70 years of age) have a higher risk of developing neutropenia and thrombocytopenia than younger patients. Therefore, Temodal should be prescribed to elderly patients with caution.
The use of Temodal may cause drowsiness and fatigue, thereby adversely affecting the ability to drive a car and operate complex machinery.
Side effect.
In clinical trials, the most common adverse events with Temodal were gastrointestinal disorders, particularly nausea (43%) and vomiting (36%). These phenomena were usually of moderate or mild severity (no more than 5 bouts of vomiting per day), went away on their own or were easily relieved by standard antiemetic therapy. Severe nausea and vomiting were observed in 4% of cases.
Other commonly encountered adverse events included fatigue (22%), constipation (17%), and headache (14%). Anorexia (11%), diarrhea (8%), rash, fever and drowsiness (6% each) were also reported. Less common (2–5% of cases) adverse events were, in descending order of frequency, asthenia, pain, including abdominal pain, dizziness, weight loss, malaise, shortness of breath, dyspepsia, alopecia, chills, itching, taste distortion and paresthesia.
Changes in laboratory parameters:
When treating patients with glioma and metastatic melanoma, cases of thrombocytopenia and neutropenia of grade 3 or 4 were observed. Hospitalization of the patient and/or discontinuation of Temodal was required in 8 and 4% of cases, respectively, for glioma and in 3 and 1.3% for melanoma. Bone marrow suppression was predictable (usually occurring within the first few cycles of treatment, peaking between days 21 and 28); recovery occurred quickly - usually within 1-2 weeks. There were no signs of cumulative myelosuppression.
Interaction.
Taking Temodal together with ranitidine does not change the degree of absorption of Temodal. Co-administration of dexamethasone, prochlorperazine, phenytoin, carbamazepine, ondansetron, H2 receptor antagonists or phenobarbital does not change the clearance of Temodal.
No studies have been conducted to determine the effects of temozolomide on the metabolism and elimination of other drugs. However, due to the fact that temozolomide is not metabolized in the liver and is weakly bound to proteins, it is unlikely that it could affect the pharmacokinetics of other drugs.
Use of Temodal in combination with other bone marrow depressants may increase the likelihood of myelosuppression.
Overdose.
With a single dose of Temodal (up to 1000 mg/m2), expected effects such as neutropenia and thrombocytopenia occurred.
Release form.
Capsules of 5, 20, 100 or 250 mg, in amber glass bottles; The bottles are equipped with lids that prevent children from opening them. There are 5 or 20 capsules in a bottle, 1 bottle in a box.
Storage conditions.
At a temperature of 2–30 °C. Keep away from children.
Best before date.
2 years. A drug that has expired should not be used.
Conditions for dispensing from pharmacies.
By doctor's prescription.
Special instructions for the use of the drug Temodal
Patients receiving Temodal therapy accompanied by radiotherapy on a 42-day cycle (maximum 49 days) are at particular risk for developing pneumonia caused by Pneumocystis carinii . Therefore, all patients with this treatment regimen require preventive measures aimed against the development of pneumonia caused by Pneumocystis carinii . There is a high risk of developing pneumonia caused by Pneumocystis carinii when using temozolomide for a long period. However, all patients receiving temozolomide, especially those receiving steroids, should be closely monitored for the development of this pneumonia despite the therapy regimen. Antiemetic therapy . Nausea and vomiting are very often associated with the use of Temodal, so the following recommendations should be followed: for patients with newly diagnosed glioblastoma multiforme, antiemetic prophylaxis is recommended before the initial dose of accompanying Temodal therapy and is strongly recommended during the adjuvant phase; In patients with recurrent or progressive glioma, antiemetic therapy may be necessary for severe vomiting (grade 3 or 4) in previous treatment cycles. Patients with impaired liver or kidney function. The pharmacokinetics of temozolomide are comparable in subjects with normal hepatic function and in patients with mild to moderate hepatic impairment. There is no data on the use of the drug in persons with severe impairment of liver function (class III according to the Child-Pugh classification) or kidneys. Given the pharmacokinetic properties of temozolomide, it is unlikely that dose reduction would be necessary in the presence of severe hepatic or renal impairment. However, caution should be exercised when prescribing Temodal to such patients. Use in children. There is no clinical experience with the use of Temodal in the treatment of children under 3 years of age with glioblastoma multiforme. There is limited experience in treating children over 3 years of age with glioma. In the case of melanoma, there is no clinical experience in treating children under 18 years of age. Use in elderly patients. Elderly patients (over 70 years of age) are at increased risk of developing neutropenia and thrombocytopenia compared with younger patients. Therefore, Temodal should be prescribed with caution to patients in this age category. During pregnancy and breastfeeding. No studies have been conducted in pregnant women. When conducting preclinical studies on rats and rabbits receiving the drug at a dose of 150 mg/m2, data on teratogenesis and/or toxicity to the fetus were obtained. Therefore, Temodal is usually not prescribed to pregnant women. If there is a need to use the drug during pregnancy, the woman must be informed of the potential risk to the fetus. Women of reproductive age should be informed of the need to avoid pregnancy while taking Temodal and for 6 months after the end of drug therapy. It is not known whether Temodal is excreted in breast milk, so it should not be taken during breastfeeding. Male patients. Temozolomide may exhibit genotoxic effects. Therefore, men taking Temodal should use effective contraception. Men taking temozolomide should not plan to have a child during treatment and for 6 months after stopping treatment. Men are advised to seek advice about sperm cryopreservation before starting treatment due to the possibility of irreversible infertility caused by temozolomide treatment. Impact on the ability to drive vehicles and operate machinery. The ability to drive vehicles and operate machinery may be impaired when taking Temodal due to the possibility of developing fatigue and drowsiness.
Diagnosis of brain tumors (BTT) is difficult due to the initial asymptomatic stage of the disease. In this regard, and also because of the impossibility of adequate surgical intervention associated with the localization of tumors, as a rule, it is necessary to use additional treatment methods. At the same time, the incidence of AGM is growing and will soon amount to 127 thousand new cases per year. In recent decades, the number of newly diagnosed primary AMCs has increased dramatically, especially in elderly patients [1, 2]. It is difficult to say whether this is directly related to morbidity or to improved diagnosis.
Most GBMs are gliomas of astrocytic, oligodendrocyte, ependymal, and mixed origin. Previously conducted large multicenter randomized trials comparing adjuvant radiotherapy, chemotherapy and chemoradiotherapy showed that chemotherapy (alone or in combination with radiotherapy) does not affect the survival of patients with AGM [3, 4]. Therefore, in the last 20 years, adjuvant radiation therapy at a dose of 60 gray in 30 fractions has remained the standard for such patients.
During this period, a scale of prognostic factors was developed and groups of patients were identified who, according to some authors, needed adjuvant chemotherapy - for example, with anaplastic astrocytomas or anaplastic oligodendrogliomas as the most sensitive tumors. However, the general approach remained the same: radiation therapy as adjuvant treatment, chemotherapy in cases of disease relapse.
For a long time, chemotherapy did not have significant success and was limited mainly to drugs from the class of nitroso derivatives. The combination of procarbazine, carmustine and vincristine (PCV), having low efficacy in case of relapses, often caused hematological toxicity (56% of cycles) and skin reactions (20% of cycles) [5]. Recently, a new drug from the class of alkylating agents has appeared - temozolomide (Temodal; Schering Plow), which is being systematically studied along with other new (including targeted) agents, such as erlotinib (Tarceva), imatinib, gefitinib (Iressa), for AGM .
Temodal is an alkylating drug, an imidazotetrazine derivative, the active metabolite of which is monomethyl-triazeno-imidazole-carboxamide (MTIC). Temodal is prescribed orally as a 5-day regimen of 150 mg/m2/day to patients who have previously received chemotherapy, and 200 mg/m2/day to untreated patients. There is a longer regimen, more often used with chemo-radiation therapy.
The dose-limiting toxicity of Temodal is hematological. The drug is convenient both for monotherapy and in combination with other drugs and/or radiation therapy, as well as for outpatient treatment; it demonstrated good tolerability and safety during phase I and II clinical studies. The drug is rapidly absorbed after oral administration and undergoes spontaneous hydrolysis to form MTIC. The mechanism of action is an alkylation reaction at the O6 position of guanine and additional alkylation at the N7 position. In the brain tissue, Temodal accumulates more intensely than in the contralateral normal brain tissue [6].
The European Organization for Research and Treatment of Cancer (EORTC), in accordance with the New Drug Development Program (NDDP), conducted a series of studies to improve the treatment of AGM (Table 1).
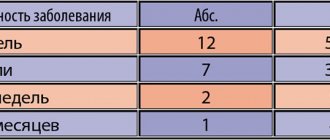
A phase II clinical multicenter study of Temodal (temozolamide) was conducted on 162 patients with the first relapse of malignant astrocytoma. In 111 patients, anaplastic astrocytomas or anaplastic mixed oligoastrocytomas were determined. Patients who had not previously received chemotherapy received Temodal 200 mg/m2/day. (5 days). In previously treated patients, the dose was reduced to 150 mg/m2/day (5 days), then it could be increased if there was no toxicity in the previous course. The courses were repeated every 28 days. Treatment was continued until intolerable toxicity or progression, for a maximum of 2 years. Progression-free survival at 6 months was 46%, at 12 months – 24%. Median progression-free survival was 5.4 months, median overall survival was 13.6 months; The 6- and 12-month survival rates were 75 and 56%, respectively. An objective effect was achieved in 35% of patients, with complete regression in 8%; an additional 26% of patients experienced stabilization of the process with a median progression-free time of 4.4 months. Hematological toxicity did not exceed 10%, side effects were mild, and treatment was accompanied by an improvement in the quality of life of patients [7].
A comparative randomized study of temozolomide (Temodal) and procarbazine, which included 225 patients with the first relapse of glioblastoma multiforme, showed the advantage of Temodal, which, among other things, was well tolerated and provided a fairly high quality of life. Six-month progression-free survival in the Temodal group was 21% versus 8% in the procarbazine group (p = 0.008), median progression-free time was 12.4 versus 8.3 weeks (p = 0.0063),
6-month survival rate – 60 versus 44% (p = 0.019) [8].
In 2002, a study of Temodal in combination with adjuvant radiation therapy for glioblastoma multiforme was started, which was then continued with randomization and inclusion of other research groups. The results of this study, reported at the plenary meeting of the American Society of Oncology (ASCO) in 2004, were sensational. A randomized study of simultaneous chemo-radiotherapy with Temodal compared with radiation therapy alone, conducted in 573 patients in 85 centers (Europe and Canada), showed a significant advantage of the combined method (Table 2) [9].
Temodal was prescribed orally at 75 mg/m2/day daily for up to 42 days simultaneously with radiation therapy in the same regimen as in the group of patients without Temodal (60 gray - 30 daily fractions of 2 gray). Patients in the combination therapy group were then prescribed up to 6 more cycles of Temodal (150–200 mg/m2/day daily for 5 days) every 28 days. Hematological toxicity of grade 3–4 was noted in only 7% of patients during chemo-radiation therapy and in 16% during monochemotherapy with Temodal. In general, the patients tolerated the treatment quite satisfactorily.
Thus, chemo-radiotherapy with Temodal should become the new standard of adjuvant treatment of malignant gliomas.
Currently, a phase II study of Temodal in combination with pegylated liposomal doxorubicin (Kelix, Doxil) is being conducted as adjuvant 1st line therapy for glioblastomas [10]. Temodal is prescribed along with standard radiation therapy, and then on days 1–5 of a 28-day cycle, starting 4 weeks after the end of radiation therapy. The dose of doxorubicin is increased from 5 to 15 mg/m2.
Temodal is also used quite successfully for relapses of acute headaches. Neyns B. et al. (2004), using standard doses of the drug in 117 adult patients, obtained complete and partial regression of tumors in 29% of cases with stabilization of the process in another 34% of patients [11].
The combination of Temodal with irinotecan (Campto) is especially interesting. Irinotecan was studied in combination with carmustine for recurrent glioblastomas in 42 patients as 2nd line chemotherapy [9]. In 9 patients (21.4%) a partial effect was achieved, in 21 (50%) the disease was stabilized. Median survival was 11.7 months. The regimen was found to be highly effective [12]. In a phase II study of irinotecan in 60 patients with recurrent malignant gliomas, a partial effect was achieved in 15% of patients, minimal regression in 7%, stabilization of the process in 48%.
Reardon D. et al. [13] conducted a phase I study of Temodal (200 mg/m2/day * 5 days) and irinotecan with dose escalation from 40 to 225 mg/m2 in 48 patients with recurrent malignant glioblastomas who additionally received anticonvulsants such as phenytoin, carbamazepine or phenobarbital (group A), and in 32 patients who did not receive these drugs (group B). The metabolism of irinotecan increases significantly with simultaneous administration of these anticonvulsants [14]. Preliminary results of this study are shown in Table. 3.
The hypothesis about the advisability of combining irinotecan and Temodal is based on data on increased cytotoxicity of irinotecan after preliminary removal of the methylguanine methyltransferase (MGMT) methyl group as a result of treatment with Temodal.
The combination was tested in 32 patients with recurrent malignant gliomas. Temodal was prescribed at a dose of 200 mg/m2/day for 5 days, irinotecan at a dose of 350 mg/m2 for 2 hours on day 6. Cycles were repeated every 28 days (maximum 6 cycles), then treatment with Temodal alone was continued for up to 6 months. All patients took additional carbamazepine or phenytoin. All of them had previously received radiation therapy, 81% had received chemotherapy, and 34% had received both regimens. In 10 out of 32 patients an objective effect was registered, in 19 – stabilization. Thus, an objective effect was achieved in 28% of patients. Six-month progression-free survival was 39%. In anaplastic astrocytomas, these figures were 36 and 71%, respectively. We have tested this combination in several patients.
We present a discharge summary of a patient who received treatment in the chemotherapy department of the Russian Cancer Research Center of the Russian Academy of Medical Sciences.
Diagnosis: glioblastoma of the brain with damage to the frontal lobes of the hemispheres with transition to the left temporo-parietal region. Condition after chemo-radiation treatment. Histology 01/14857: polymorphic cell variant of glioblastoma.
From the anamnesis: since March 2001 - persistent headaches, memory impairment, convulsive episodes. The examination revealed polymorphic cell glioblastoma of the brain. Due to the prevalence of the process, surgical treatment was considered impossible. In September - October 2001, radiation therapy was performed to the entire brain: 34 gray and locally to the tumor area (SD 63 gray). From December 2001 to March 2002, 4 courses of chemotherapy with Campto and Temodal were administered with stabilization of the tumor process and partial regression of neurological symptoms. Repeated courses of Temodal in mono mode were carried out on an outpatient basis from October to December 2002 and from June to August 2003. Stable stabilization of the tumor process was maintained. One month after the last course of chemotherapy with Temodal - in September 2003 - a deterioration in neurological symptoms was noted.
MRI of the brain 03.10.03: in the right hemisphere, a parasagittal tumor node 2.7 * 3 cm without clear contours with pronounced perifocal edema at the level of the ventricles of the brain merges with the tumor located in the left frontal and parietal lobes. The ventricles of the brain are deformed and compressed, more so on the left. The total size of the tumor lesion is 6.7 * 8 cm in diameter, in the structure of the nodes there are areas of increased intensity of the MR signal, most likely zones of decay. The median structures are slightly displaced. Compared to the study from February 2002, there were negative dynamics in the form of an increase in the size of the tumor lesion and the area of perifocal edema.
On 10/09/03, an attempt was made to chemotherapy with nitroso derivatives: nimustine at a dose of 2.5 mg/kg, a total of 200 mg administered. He tolerated the treatment satisfactorily. There were no side effects. Deterioration of neurological symptoms was noted. In December, an attack of renal colic developed; after removal of a stone from the right ureter and antibiotic therapy, chemotherapy with Temodal and Campto was resumed. 7 courses were carried out at intervals of 3–4 weeks with slowly increasing positive dynamics in terms of general condition and neurological status. At the control MRI of the brain dated 02/19/04: a slight decrease in perifocal edema and the size of the tumor lesion, compression of the left lateral ventricle was less pronounced. During the control MRI from 06/09/04, compared with the study from 02/19/04, no significant dynamics were noted, compared to 10/03/03 - positive dynamics. Upon restoration of blood counts, treatment was administered from August 12 to August 17, 2004: Temodal 300 mg orally from days 1 to 5 (total 1500 mg), Campto - 500 mg intravenously as a 90-minute infusion on day 6. He tolerated the treatment satisfactorily.
Thus, with a significant improvement in cerebral symptoms and long-term stabilization of the process (minimal effect), treatment continues for more than 2.5 years.
Temodal is being studied with interest by many clinicians in patients with metastases of malignant tumors to the brain. Serrone L. et al. [15] reported the use of Temodal after radiation therapy for melanoma metastases to the brain. Initially, radiation therapy was administered at a total dose of 24 gray, and from week 7 Temodal was prescribed at a dose of 150 mg/m2/day for 5 days every 4 weeks, for a total of 6 cycles. Preliminarily, 15 patients were evaluated. In 3 patients partial regression was achieved, in 5 patients the process stabilized.
The Temodal regimen at 200 mg/m2 for 5 days in combination with liposomal doxorubicin at a dose of 40 mg/m2 per day (repeated every 28 days) Caraglis M. et al. was also used to treat 12 patients with brain metastases from various solid tumors, predominantly non-small cell lung cancer (NSCLC) and breast cancer. When using this combination, 2 complete and 2 partial regressions were achieved. The survival rate of patients with complete regression was 27+ months. Clinical effect was achieved in another 4 patients (1 with melanoma, 3 with NSCLC).
The Chemotherapy Department of the Russian Cancer Research Center, Russian Academy of Medical Sciences, studied monotherapy with Temodal in standard doses (150–200 mg/m2/day * 5 days, every 28 days) in 11 patients with metastases of NSCLC, breast cancer and melanoma to the brain. Clinical effectiveness (partial regression + disease stabilization) was 36.3%; partial regression was achieved in one patient with melanoma. Stabilization of the process within 6 months was observed in 3 patients with NSCLC metastases.
Toxicity was assessed across 32 chemotherapy courses; Grade 3–4 hematological toxicity was extremely rare (Table 4). Non-hematological toxicity did not exceed grades 1 and 2 (Table 5)
Fourteen patients with brain metastases received chemo-radiation treatment in the following regimen: Temodal 75 mg/m2/day on days 1–14 along with radiation therapy at a dose of 30 gray (3 gray * 10 fractions). The results of combined treatment are presented in table. 6. The overall effect was 71%, stabilization – 22%. Data on patient survival are presented in table. 7.
For brain metastases, treatment with Temodal and Campto is possible. As an example, we present the discharge summary of a patient who received treatment in the chemotherapy department of the Russian Cancer Research Center of the Russian Academy of Medical Sciences.
Diagnosis: disseminated melanoma of the central nervous system. Condition after surgical interventions in 1996, 2002, chemo-radiation treatment.
Histology 02/17635: epithelial and spindle cell pigment-containing melanoma with a large number of hemorrhages.
Surgery in the posterior cranial fossa for a tumor in Israel in 1996. Surgery for a relapse on June 24, 2002 in the same place (palliative). In August 2002, MRI revealed complete tumor contamination of the central nervous system with intradural blockade at the L1–L2 level, and palliative laminectomy was performed. On admission: severe neurological symptoms, including ataxia, but no headaches. MRI shows a tumor node in the projection of the inferior cerebellar vermis with growth into the lateral cistern of the medulla oblongata, with a second intracranial node nearby. When examining the entire spine and spinal cord, multiple tumor nodes up to 1 cm are detected, mainly located in the lower thoracic and lumbar spine. X-ray of the lungs and ultrasound of the abdominal organs, as well as physical examination, did not reveal any tumor pathology.
02–06.11.02 and 16–20.12.02 against the background of active symptomatic therapy (anticonvulsants and decongestants), 2 courses of chemotherapy with Temodal 150 mg were administered (doses were slightly reduced due to concurrent radiation therapy, the interval between cycles was increased due to thrombocytopenia and neutropenia grade 2). While using ondansetron, he tolerated the treatment satisfactorily.
11/10–21/02 irradiation of the entire brain with 2 side fields (ROD 3 gray, SOD 30 gray, photons 6 meV).
11.27–12.25.02 irradiation of the entire spinal cord in 3 levels (ROD 2 grays, SOD 40 grays, an additional dose of 5 grays was given to the L2-S1 area).
12/20–25/02 4 fractions of 3 grays were applied to the cerebellum area. There was an increase in neurological symptoms at a dose of 21 gray, which was stopped. In a relatively satisfactory condition, the patient is discharged under the supervision of a district oncologist.
After 3 weeks - a repeat MRI with contrast to evaluate the effect and decide whether to continue treatment with Temodal on an outpatient basis. Considering long periods of thrombocytopenia up to 3 tbsp. at long intervals, he is currently receiving repeated courses of Temodal and Campto without signs of progression. The duration of treatment is about 2 years.
Thus, today Temodal has not only revived interest in the drug treatment of acute tumors and metastases of malignant tumors in the brain, but also made it possible to develop new standards of adjuvant therapy for malignant gliomas, significantly advancing the possibilities of treating such patients.
The possibility of using Temodal simultaneously or sequentially with other treatments opens up new promising prospects.
Drug interactions Temodal
The combined use of Temodal with ranitidine or with food does not lead to clinically significant changes in the absorption of the drug. Co-administration of dexamethasone, prochlorperazine, phenytoin, carbamazepine, ondansetron, histamine H2 receptor antagonists or phenobarbital does not change the clearance of Temodal. Co-administration of valproic acid caused a mild but statistically significant decrease in the clearance of temozolomide. Use of Temodal with other bone marrow depressants may increase the likelihood of developing myelosuppression.
Temodal drug overdose, symptoms and treatment
Doses of 500, 750, 1000 and 1250 mg/m2 (total dose over a 5-day cycle) have been evaluated in patients clinically. Dose-related hematologic toxicity occurred at all doses but, as expected, was more severe at higher doses. One patient exceeded the dose of 2000 mg/day for 5 days, which resulted in pancytopenia, pyrexia, multiorgan failure and death. Patients taking recommended doses (150–200 mg/m2) for more than 5 days (up to 64 days) have been reported to develop bone marrow suppression (with or without infection), in some cases severe and prolonged, with death. In case of overdose, it is recommended to perform a hematological study and, if necessary, maintenance treatment.