Anticholinesterase drugs are a special class of drugs that block the enzyme acetylcholinesterase, which destroys the neurotransmitter acetylcholine at synapses - the points of contact between nerve cells. At the same time, the concentration of acetylcholine in the synaptic cleft increases and its effects are significantly enhanced.
Acetylcholine is a transmitter of impulses in the peripheral nervous system, regulating the functioning of many internal organs and systems (in particular, the brain, heart, bronchi, uterus, gastrointestinal tract, urinary system, etc.).
Acetylcholine realizes its effects by interacting with special structural components of cells - receptors, namely cholinergic receptors. Depending on their location and functions, adrenergic receptors are classified into M- and N-cholinergic receptors.
M-cholinergic receptors are located mainly in the brain, heart, bronchi, gastrointestinal tract, iris, and urinary tract. The effects of M-cholinergic receptor stimulation include pupil constriction, decreased intraocular pressure, increased gastric acid production, increased secretion of digestive glands, increased gastrointestinal motility and peristalsis, increased bladder tone, and decreased heart rate.
N-cholinergic receptors are localized mainly in skeletal muscles, as well as in special structures - autonomic ganglia and carotid glomeruli. When they are stimulated, muscle contraction, vasoconstriction (and, as a consequence, increased blood pressure) and stimulation of the respiratory center in the brain are observed.
There is a separate class of drugs that can directly stimulate cholinergic receptors (cholinomimetics, cholinergic stimulants), as well as a group of drugs that have an indirect effect - by inhibiting the enzyme acetylcholinesterase, they increase the amount of acetylcholine and enhance its connection with cholinergic receptors (and, as a result, effects). These drugs are called anticholinesterase drugs.
Indications for use
Anticholinesterase drugs are used for myasthenia gravis - severe chronic muscle weakness, disorders of muscle tone after injuries to the brain and spinal cord, inflammation of the membranes of the brain and spinal cord - meningitis, polio, encephalitis, as well as neuritis, optic nerve atrophy.
Anticholinesterase drugs are also used for intestinal and bladder atony, including after abdominal surgery, persistent increase in intraocular pressure (glaucoma), as well as in case of overdose of drugs of the class of antidepolarizing muscle relaxants (tubocurarine, pancuronium, pipecuronium, vecuronium, rocuronium, atracurium, etc.) .d.), which are used in complex anesthesia.
In addition, anticholinesterase drugs are used for memory disorders - mental retardation in children, senile dementia (including Alzheimer's disease), as well as in the complex treatment of multiple sclerosis.
Read also[edit | edit code]
- Anatomy and physiology of the nervous system
- Parasympathetic nervous system
- Sympathetic nervous system
- Synaptic transmission
- Acetylcholine
- Cholinergic receptors and synapses
- Anticholinergics
- Nicotine
- M-cholinergic receptor stimulants
- M-cholinergic receptor blockers
- Acetylcholinesterase inhibitors (AChE)
- Poisoning with acetylcholinesterase blockers
- Nerve transmission at neuromuscular synapses and autonomic ganglia N-cholinergic receptors
- Muscle relaxants
- Agents acting on the autonomic ganglia
- Ganglion stimulators
- Ganglioblockers
Features of treatment with anticholinesterase drugs
Anticholinesterase drugs can cause nausea, vomiting, diarrhea, increased production of saliva, convulsions, and bronchospasm. To eliminate the side effects of anticholinesterase drugs, drugs from the group of M-anticholinergic blockers (in particular, atropine sulfate) are used.
Anticholinesterase drugs are contraindicated for use in patients with epilepsy, Parkinson's disease (shaking palsy), bronchial asthma, heart disease, and gastric and duodenal ulcers.
Results and discussion
In the first two weeks, during which patients received the drugs in a hospital setting, no adverse events were reported in any case.
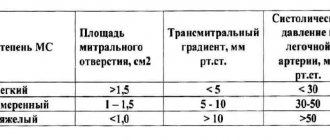
The IOP level (Table 2) was normalized throughout the observation period and was at a level not exceeding 15 mm Hg.
Table 2. Dynamics of ophthalmotonus indicators (mm Hg) Note. Here and in the table. 3: p>0.05 compared to the original data.
This level of IOP corresponded to the target pressure recommended by the European Glaucoma Society, taking into account the stage of the glaucomatous process.
In cases where doubts arose about the actual target IOP, flowmetry was performed, which made it possible to clarify the indicators of the individual level of ophthalmotonus.
One of the criteria for assessing functional capabilities is central visual acuity (Table 3). Neuroprotective therapy, as a rule, does not affect this indicator, however, mentioning it is important as indirect evidence of the dynamics of the process.
Table 3. Dynamics of visual acuity indicators
In our case, central visual acuity remained stable. Some improvement in vision was noted in some patients in both groups.
One of the objective criteria for assessing the effectiveness of neuroprotective therapy, to a certain extent, can be considered visual field testing. We considered the indicators taken into account when assessing changes in visual functions as CPZ, foveal and total photosensitivity, PPV, MD and PSD indicators. The data obtained before and after the course of stabilizing therapy are presented in table. 4.
Table 4. Dynamics of static perimetry indicators by group
The study was conducted before the start of the course of drug therapy and 3.6 months after it. As can be seen from table. 4, all average indicators tended to improve, especially for the central and peripheral visual fields. Moreover, in the group of patients receiving gliatilin, this trend was more significant. This is all the more important because the baseline data of both groups were comparable.
We are inclined to believe that the more pronounced therapeutic effect in patients of group 1 is due to the action of gliatilin. This assumption is confirmed by observation data of a large number of patients periodically receiving such therapy at the institute.
Side effects
The negative effects of drugs are due not only to the chemical characteristics and level of toxicity of the main pharmacologically active component. Side effects can be caused by excipients of the drugs.
Their list is more diverse than the list of cholinomimetic compounds. Therefore, all drugs have a different set of negative manifestations.
Common side effects for topical M-cholinomimetics are distributed according to the frequency of occurrence as follows:
- Migraine is a headache of varying intensity and duration.
- Follicular conjunctivitis is an inflammation of the conjunctival membrane and lymphatic follicles of the eye organ.
- Contact dermatitis of the skin of the eyelids is an allergic reaction to certain components of medications.
- Severe constriction of the pupillary element for a long period of time when using M-cholinomimetics of conditionally irreversible action.
When taken orally, nausea and vomiting are most often observed, which is associated with the increased toxicity of M-cholinomimetic drugs. Chills and increased sweating are less common.
Such side effects are explained by the stimulation of the endocrine system by ammonium compounds. Sometimes, while taking oral or injectable M-cholinomimetics, there is an increase in the urge to urinate.
Renorrhea, lacrimation and increased salivation are associated with the ability of such substances to increase the functional activity of the exocrine glands. With the ophthalmic use of medications of this pharmacological category, temporary visual disturbances are observed.
Other side effects include hyperemia, a flush of heat to the face, and a sharp jump in blood pressure. The respiratory system may respond to the administration of anticholinesterase substances with bronchospasm, swelling of the lung tissue, and difficulty breathing.
Induced myopia develops within 15 minutes. after topical application of the drug and reaches a maximum after 1-1.5 hours.
In ophthalmological practice, some patients experienced:
- nuclear cataract – clouding of the central part of the lens;
- swelling of the corneal endothelium;
- atypical disc-shaped keratopathy, manifested by increased photosensitivity, sensation of a foreign body in the orbit, hyperemia, pain.
The digestive system is characterized by side effects such as pain in the epigastric zone, increased intestinal motility, and stool disturbances.
M-cholinomimetics
There are subtypes of M-cholinergic receptors - M1-, M2- and M3-cholinergic receptors.
M-cholinergic receptors are localized in the central nervous system, in the enterochromaffin cells of the stomach; M2-cholinergic receptors - in the heart; M3-cholinergic receptors - in the smooth muscles of internal organs, glands and in the vascular endothelium (Table 3).
| Organs and tissues | M1 | M2 | M3 |
| CNS | + | – | – |
| Orbicularis iris muscle | – | – | + |
| Ciliary (ciliary) muscle | – | – | + |
| Cardiomyocytes | – | + | |
| Endothelium of blood vessels1 | – | – | + |
| Smooth muscles of the bronchi, gastrointestinal tract | – | – | + |
| Salivary, bronchial, sweat glands | – | – | + |
| Enterochromaffin-like cells of the stomach | + | – | – |
| 1When M3 cholinergic receptors are stimulated in the endothelium of blood vessels, endothelial relaxing factor NO is released; the vessels dilate. |
When M1- and M3-cholinergic receptors are excited through Gq proteins, phospholipase C is activated, inositol 1,4,5-triphosphate (IP3) is formed, which promotes the release of Ca2+ from the sarcoplasmic (endoplasmic) reticulum. The level of intracellular Ca2+ increases, and excitatory effects develop.
When stimulating the M2 cholinergic receptors of cardiomyocytes through Gi proteins, adenylate cyclase is inhibited, the level of cAMP and, accordingly, the activity of protein kinase A and the level of intracellular Ca2+ are reduced. In addition, when M2 cholinergic receptors are excited, K+ channels are activated through G proteins, and hyperpolarization of the cell membrane develops. All this leads to the development of inhibitory effects.
M2-cholinergic receptors are also present at the endings of postganglionic parasympathetic (cholinergic) fibers; when presynaptic M2 cholinergic receptors are excited, the release of the neurotransmitter acetylcholine decreases.
M2-cholinergic receptors are also present at the endings of noradrenergic fibers; upon stimulation of presynaptic M2 cholinergic receptors of noradrenergic nerve endings, the release of the transmitter norepinephrine decreases.
Muscarine is a fly agaric alkaloid, a quaternary ammonium compound (polar compound).
Muscarine does not penetrate the blood-brain barrier and therefore does not have a significant effect on the central nervous system.
Muscarine stimulates all subtypes of M-cholinergic receptors.
Due to the stimulation of M1-cholinergic receptors of enterochromaffin cells of the stomach, muscarine increases the release of histamine, which stimulates the secretion of hydrochloric acid (Fig. 67).
Due to the stimulation of M2 cholinergic receptors, muscarine reduces heart contractions (causes bradycardia) and impedes atrioventricular conduction.
Due to the stimulation of M3 cholinergic receptors, muscarine:
1) constricts the pupils of the eyes (causes contraction of the orbicularis muscle of the iris);
2) causes a spasm of accommodation (contraction of the ciliary, or ciliary, muscle leads to relaxation of the zonular ligament; the lens becomes more convex, the eye is set to the near point of vision); .
3) increases the tone of smooth muscles of internal organs (bronchi, gastrointestinal tract and bladder, with the exception of sphincters);
4) increases the secretion of bronchial, digestive and sweat glands;
5) reduces the tone of blood vessels (most vessels do not receive parasympathetic innervation, but contain non-innervated M3 cholinergic receptors; stimulation of M3 cholinergic receptors of the vascular endothelium leads to the release of NO, which causes relaxation of vascular smooth muscles).
Muscarine is not used in medical practice. The pharmacological effect of muscarine can occur in case of fly agaric poisoning . Constriction of the pupils of the eyes, severe salivation and sweating, a feeling of suffocation (increased secretion of the bronchial glands and increased bronchial tone), bradycardia, decreased blood pressure, cramping abdominal pain, vomiting, and diarrhea are noted.
The muscarine content varies in different types of fly agarics. Due to the action of other fly agaric alkaloids (muscimol, etc.), stimulation of the central nervous system is possible - anxiety, delirium, hallucinations, convulsions.
When treating fly agaric poisoning, the stomach is washed and a saline laxative is given. To weaken the effect of muscarine, the M-anticholinergic blocker atropine is administered. If symptoms of central nervous system excitation predominate, atropine is not used. To reduce the effects of central nervous system excitation, benzodiazepine drugs (diazepam, etc.) are used.
Of the M-cholinomimetics, pilocarpine, aceclidine and bethanechol are used in practical medicine.
Pilocarpine is an alkaloid from the Pilocarpus Jaborandi shrub, native to South America. The drug is used mainly topically in ophthalmic practice (a diagram of the eye is shown in Fig. 20). Pilocarpine constricts the pupils of the eyes and causes a spasm of accommodation (increases the curvature of the lens).
Rice. 20. Diagram of the eye.
Constriction of the pupils of the eyes (miosis) occurs due to the fact that pilocarpine causes contraction of the circular muscle of the iris (innervated by parasympathetic fibers). Pilocarpine stimulates M3 cholinergic receptors of the orbicularis iris muscle; The orbicularis muscle contracts and the pupil narrows. After instillation of a solution of pilocarpine (eye drops) into the conjunctival sac, the constriction of the pupil begins after 10 minutes, the maximum effect is achieved after 30 minutes. The pupil size is restored to its original size after 6 hours.
Pilocarpine increases the curvature of the lens. This is due to the fact that pilocarpine stimulates the M3 cholinergic receptors of the ciliary (ciliary) muscle and causes its contraction. The ciliary muscle forms a ring containing the lens. The ligament of Zinn (ciliary band) connects the lens capsule along its entire perimeter with the ciliary muscle.
When the ciliary muscle contracts, the ligament of Zinn relaxes and the lens tends to take on the ideal shape of a ball. The curvature of the lens increases, its refractive power increases, the eye is set to the near point of vision (a person sees near objects well and far objects poorly). This phenomenon is called a spasm of accommodation (Fig. 21). In this case, macropsia occurs (seeing objects in an enlarged size).
Rice. 21. Effect of pilocarpine on accommodation.
In ophthalmology, pilocarpine in the form of eye drops (1 drop 4–6 times a day), eye ointment, and eye films are used for glaucoma, a disease that is manifested by an increase in intraocular fluid pressure and can lead to visual impairment.
There are closed-angle (narrow-angle) and open-angle (wide-angle) forms of glaucoma.
Intraocular fluid is formed in the ciliary body due to:
1) its secretion by epithelial cells of the ciliary body;
2) filtration of blood plasma through the capillaries of the ciliary body.
Next, the intraocular fluid enters the posterior chamber of the eye (between the lens and the posterior surface of the iris) and through the pupil into the anterior chamber of the eye (between the cornea and the anterior surface of the iris).
The outflow of intraocular fluid from the anterior chamber of the eye occurs through the angle of the anterior chamber, in which the pectineal (pectineal) ligament is located. Through the spaces (crypts) between the trabeculae of the pectineal ligament (fountain spaces), the outflow of intraocular fluid occurs, which then enters Schlemm's canal (venous sinus of the sclera). Trabeculocanalicular outflow accounts for approximately 80% of aqueous humor outflow; about 20% is uveoscleral outflow (outflow of intraocular fluid through the soft choroid of the inner surface of the sclera).
In angle-closure (narrow-angle) glaucoma, the angle of the anterior chamber of the eye (between the cornea and iris) is narrow. When the pupil dilates (relaxation of the circular muscle of the iris and contraction of the radial muscle of the iris), the iris fills the angle of the anterior chamber and prevents the outflow of intraocular fluid - intraocular pressure increases.
Pilocarpine causes constriction of the pupils and thus facilitates access of intraocular fluid to the angle of the anterior chamber of the eye, improves the trabeculo-canalicular outflow of intraocular fluid; at the same time, increased intraocular pressure decreases. The decrease in intraocular pressure under the action of pilocarpine begins after 10–30 minutes and lasts 4–6 hours.
In open-angle (wide-angle) glaucoma, the angle of the anterior chamber of the eye is wide and pupil dilation does not limit the outflow of intraocular fluid. But the outflow of intraocular fluid is reduced due to a decrease in the spaces between the trabeculae of the pectineal ligament (fountain spaces).
In open-angle glaucoma, pilocarpine can improve the outflow of intraocular fluid due to the fact that when the ciliary muscle contracts, tension is transferred to the trabeculae of the pectineal ligament. The trabecular zone expands; at the same time, the spaces between the trabeculae (fountain spaces) increase, and the outflow of intraocular fluid improves.
Sometimes pilocarpine in small doses (5 mg) is prescribed orally to stimulate the secretion of the salivary glands for xerostomia (dry mouth) caused by radiation therapy for tumors of the head or neck.
Aceclidine is a synthetic compound that differs from pilocarpine in less toxicity. Aceclidine is administered subcutaneously for intestinal and bladder atony.
Bethanechol is a synthetic M-cholinomimetic that is used orally and subcutaneously for postoperative atony of the intestine or bladder.
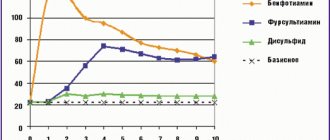
Classification of analeptics
Analeptics are classified mainly according to their mechanism of action and chemical structure:
- Direct-acting drugs (directly stimulate the respiratory and vasomotor centers): xanthines: caffeine-sodium benzoate;
- imidazole dicarboxylic acid derivatives: etimizole;
- dioxopiperidine derivatives: bemegride;
- other drugs: carbon dioxide (CO 2 );
- alkaloids – cytisine, lobeline;
- alkylated acid amides: niketamide;
pharmachologic effect
All analeptics increase the excitability of the respiratory and vasomotor centers. At the same time, breathing accelerates and becomes deeper, and blood pressure rises due to increased tone and vascular spasm, blood circulation is normalized.
The effect of analeptic drugs appears only against the background of suppression of these centers. In a healthy person, analeptic drugs are practically ineffective.
Camphor and its soluble drug sulfocamphocaine increase the strength of heart contractions and blood circulation in the lungs.
Caffeine sodium benzoate, in addition to analeptic, has a psychostimulating effect and increases low blood pressure, in addition, it is effective for migraines.
Cytisine additionally reduces cravings for nicotine and is used to treat tobacco addiction.