On July 16, Elena Bogolyubova was detained by employees of the Federal Customs Service at the exit from the post office. The package she had just received contained a medicine - freesium. The drug was intended for her ten-year-old son Misha, who suffers from Batten disease. This is a genetic disease with seizures, vision loss, and impaired mental and physical development. Misha is a bedridden patient and needs constant anticonvulsants.
Bogolyubova was interrogated for seven hours at the post office, despite requests to let her go to her sick child. They were released only at 11 pm. After the intervention of the head of the Vera Hospice Fund, Nyuta Federmesser, she called the government. While the interrogation lasted, the child began to have stomach bleeding. They managed to stop him, but the mother was never given the medicine. The woman was facing a criminal case for smuggling of potent substances.
As the Ministry of Health later emphasized, Russia has a mechanism for importing unregistered drugs; permission is given by the department itself upon application from a medical, scientific or educational organization. The Central Customs Administration said Bogolyubova did not have a prescription for the medicine. Although there was an extract from a consultation of doctors, they can only recommend the drug, and not prescribe it. What saved the woman was the public outcry: after numerous publications in the media and speeches by philanthropists, even the press secretary of the Russian President Dmitry Peskov commented on the case, noting that the Kremlin would ask the Ministry of Health to “intensify work in this direction.”
Meanwhile, the case turned out to be far from isolated. The situation was exactly repeated just a month later. On August 15, another woman was detained at a post office in Moscow while receiving freesium. In August, mothers of 82 children with disabilities wrote an open letter to Russian President Vladimir Putin asking him to solve the problem of anticonvulsant drugs, which are not registered in the country, but are successfully used all over the world (it was published on Facebook by Nyuta Federmesser).
Similar stories happened with other drugs: in 2018, Ekaterina Konnova was detained for trying to sell the psychotropic drug diazepam, which was not suitable for a child with a disability. In April, a resident of Yekaterinburg, Daria Belyaeva, came under criminal investigation for ordering a package of the antidepressant bupropion from Poland.
Brief description of the drug
Frisium is a well-known representative of the clinical and pharmacological group of benzodiazepine derivatives. It was synthesized for the treatment of patients with excessive nervous excitability and anxiety, neuroses, and psychoses. But soon its ability to stop and prevent epileptic seizures was noticed. Therefore, the scope of its application has expanded, including in pediatrics.
The list of contraindications for Frisium is very wide, which explains the presence of a large number of contraindications for the drug. And due to pronounced, rapid psychological and physical addiction, the drug was withdrawn from free sale.
Active composition and release factors
Frisium is produced by the German manufacturer HOECHST in the form of round tablets with a score for convenient dosing. They are placed in 10 pieces in blisters made of metallized foil. The amount of active ingredient in tablets corresponds to 5, 10 or 20 mg. Inside the cardboard box, in addition to 3 blisters, there are detailed instructions for using the tranquilizer.
The active ingredient in Frisium is clobazam. The auxiliary composition is represented by chemically inert ingredients. They act as stabilizers and preservatives and form the basis of the tablet. Microcrystalline cellulose, titanium dioxide, talc and other components ensure the maximum possible absorption of clobazam. At the same time, they protect the active ingredient from destruction by aggressive gastric juices.
Pharmacological properties
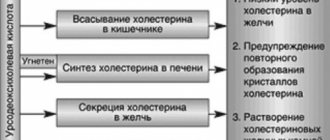
The therapeutic effect of the tranquilizer is based on the ability of clobazam to stimulate benzodiazepine receptors. When in contact with the amygdala complex in the limbic system, it significantly improves the mental state of the patient. Frisium quickly eliminates anxiety, fear, emotional stress, and restlessness. The drug is characterized by the following pharmacological properties:
- central muscle relaxant;
- anticonvulsant;
- sedative;
- hypnotic.
The drug reduces symptoms of neurological origin. It relaxes skeletal muscles, eliminating cramps and painful spasms.
After taking the tablet, the active substance enters the systemic bloodstream after 15-30 minutes (depending on the amount of food in the stomach). Clobazam binds to serum proteins and is then transported to target organs. It is metabolized by liver cells and then evacuated from the body with each bladder emptying.
Indications for treatment
The indication for taking Frisium is a pathological deterioration in a person’s psycho-emotional state. Its typical clinical manifestations are anxiety, acute or chronic feelings of fear, agitation, tension, and increased irritability.
In the treatment of epilepsy in adults and children, Frisium is used only in combination with other drugs.
Doctors include the drug in therapeutic regimens when diagnosing insomnia, organ neurosis, migraines, and menopausal disorders in patients.
The use of anticonvulsants in pediatric practice
The history of drug treatment of epilepsy begins in the mid-19th century, when the anticonvulsant effect of bromides was discovered. Bromine salts suppressed generalized tonic-clonic seizures, but had a strong sedative effect and were toxic with long-term use [1]. Since the beginning of the 20th century. The first anticonvulsant drug from the group of barbiturates, phenobarbital, is widely used. Subsequently, other barbiturates came into practice - primidone (hexamidine) since 1952 and the domestic drug benzonal. However, the sedative effect of barbiturates was still too high. In 1937, the use of phenytoin began. A positive property of phenytoin was the lack of sedation; disadvantages included nonlinear kinetics and pronounced cosmetic side effects. Today, barbiturates and phenytoin are still produced and used in Russia, however, in most developed countries, drugs from these groups are considered obsolete and their use in pediatric practice is not recommended.
60s of XX century. — the time when in developed countries drugs that are now classified as basic anticonvulsants came into practice: valproate, carbamazepine, ethosuximide, benzodiazepines, sulthiam, acetazolamide. This generation of drugs gradually replaced the more toxic older anticonvulsants and dominated the market until the mid-1990s. Benzodiazepines subsequently moved into the category of drugs of the third or fourth line of choice due to the often developing tolerance of attacks to them.
The 1990s saw the emergence of the so-called “new” anticonvulsants: oxcarbazepine, lamotrigine, vigabatrin, gabapentin, felbamate, topiramate, tiagabine, zonisamide, stiripentol (the drugs are listed in the order of their appearance on the market). Some of these drugs are registered in Russia, and not all of them are approved for use in children (Table 1). This review concerns the use of both basic and new anticonvulsants in pediatric epileptology. The daily dose of anticonvulsants in pediatric epileptology is calculated based on the patients' body weight. Dosages, including for outdated anticonvulsants, are given in Table 2.
Major anticonvulsants
Sodium valproate. The history of clinical use of valproate goes back more than 35 years, and during this time it has become one of the most popular anticonvulsants [2]. Valproic acid and its salts have a wide spectrum of action and can be prescribed for almost all forms of epilepsy as first-line drugs of choice, even before the form of the disease is clarified. An exception is West syndrome, in which valproate is significantly inferior in effectiveness to vigabatrin and hormonal therapy. The wide spectrum of action of the drug is usually associated with multiple mechanisms of action. Valproate has been reported to block voltage-gated sodium channels in neurons, however, unlike carbamazepine and phenytoin, it does not affect the restoration of the channel from an inactivated state. Valproate in high concentration acts on T-type calcium channels, reduces the concentration of aspartate and increases the level of GABA [3].
Valproates are also characterized by a low (2%) level of seizure aggravation [4]. The advantages of the drug include the ability, if necessary, to prescribe the drug immediately in the minimum therapeutic dose, bypassing a period of long titration. If the minimum therapeutic dose is ineffective, move to the intermediate and maximum doses before changing the drug or resorting to polytherapy. Since the effect of valproate may be delayed, the interval between dose increases should be 2 weeks to 1 month.
The pharmacy chain has a large number of children's (syrup, drops), divisible retardated forms (Depakine Chrono, Convulex Retard), and enteric forms (Depakine Enteric). Preference should be given to retardated forms, since taking the anticonvulsant twice a day is more convenient for the student’s parents. An individual dose should be prescribed per kg of body weight per day, but so that the daily dose can be easily selected using a measuring spoon or marks on a divisible tablet, since any inconvenience associated with taking the medicine leads to non-compliance (missing doses, unauthorized dose change). Long-term use of valproate requires monitoring of liver enzymes (ALT, AST), pancreas (amylase), and ammonium levels in the blood. An increase in ammonium levels occurs in 20–50% of patients and is most often asymptomatic, but in some cases it can manifest as symptoms of encephalopathy. Another serious complication of valproate therapy is hepatopathy, the risk of which is especially high in children under 2 years of age receiving polytherapy. L-carnitine is used as an antidote for valproic encephalopathy and hepatopathy [2].
The therapeutic concentration of the drug is 50–100 mg/l, but the need to measure it arises either during polytherapy together with enzyme-inducing drugs, or in case of resistance of attacks to therapy.
Carbamazepine. It is believed that carbamazepine (finlepsin, tegretol) stabilizes the voltage-dependent sodium channel in an inactivated state, but other mechanisms are also suggested [3]. Carbamazepine is effective in cryptogenic and symptomatic partial epilepsies (simple, complex and secondary generalized seizures), and isolated primary generalized tonic-clonic seizures. Its use in idiopathic generalized epilepsy is limited due to carbamazepine aggravation of absence seizures and myoclonus. In some cases, in the presence of secondary bilateral synchrony on the EEG in symptomatic frontal lobe epilepsy, carbamazepine is also capable of aggravating seizures.
The risk of atypical evolution associated with the use of carbamazepine has led to restrictions on the use of this drug in rolandic epilepsy. However, carbamazepine is highly effective in childhood occipital epilepsy with late onset (Gastaut form) and in autosomal dominant frontal epilepsy with nocturnal paroxysms [5]. Its structural similarity to tricyclic antidepressants allows it to be used in psychiatric practice; in addition, the drug is effective for trigeminal neuralgia.
In practice, it is important that carbamazepine is completely metabolized to carbamazepine 10-11-epoxide, while inducing microsomal liver enzymes. This means that, having decided on the target dose (in children, usually in the range of 10–30 mg/kg body weight per day), it is necessary to start with a prescription of about 5 mg/kg body weight per day and increase the dosage gradually to avoid dose-dependent side effects. The drug is capable of reducing the concentration of valproate, and although (for resistant partial epilepsies) it can be used in combination with them, such a scheme is not considered rational and may require monitoring the level of drugs in the blood. The therapeutic concentration of carbamazepine is 4–12 mg/l.
In pediatrics, divisible retardated forms of carbamazepine (finlepsin retard, tegretol CR) are convenient for use, allowing the drug to be prescribed 2 times a day, despite the short half-life of carbamazepine. During long-term treatment with carbamazepine, it is necessary to examine the child’s skin and mucous membranes and monitor hematological parameters. For timely diagnosis of secondary bilateral synchrony, control EEG studies should be performed.
Ethosuximide. The only mechanism of action of ethosuximide (Suxilep) is the blockade of voltage-dependent T-type calcium channels [3]. The uniqueness of this mechanism ensures its high effectiveness in absence seizures, both typical (in idiopathic generalized epilepsy) and atypical (in Lennox-Gastaut syndrome, atypical benign partial epilepsy, Landau-Kleffner syndrome, etc.). In addition, ethosuximide is effective for so-called “frontal absence seizures” and negative myoclonus. However, the drug is ineffective against generalized tonic, tonic-clonic and all types of partial seizures, which does not allow the use of ethosuximide as monotherapy; The most commonly used combination is ethosuximide and valproate, which has true synergism for absence seizures in children [2].
The advantages of the drug include the possibility of prescribing it immediately in a therapeutic dose, the disadvantages are the absence of pediatric and divisible forms in Russia.
New anticonvulsants
Lamotrigine. Lamotrigine (Lamictal) blocks voltage-gated sodium channels, but in a different manner than carbamazepine, as might be expected from the broad spectrum of action of this drug. Blockade of voltage-dependent calcium channels has also been reported, leading to a decrease in the excitatory effect of glutamate [1, 3]. The spectrum of action of lamotrigine includes all types of seizures and practically coincides with the spectrum of action of valproate. The interaction of these two drugs is synergistic, with valproate increasing the concentration of lamotrigine, which allows reducing the dose of the latter and thereby affecting the overall cost of treatment.
Disadvantages of lamotrigine include the development of skin rash (in 11% of children) and Stevens-Johnson and Lyell syndromes [1]. The risk of complications is reduced with slow dose titration, but this limits the use of lamotrigine as a first-line drug for newly diagnosed epilepsy. When prescribing the drug for the first time, it is necessary to increase the dose strictly in accordance with the instructions for use of the drug and teach parents to examine the child’s skin and mucous membranes daily. In the future, there will be no need for such control.
The positive properties of lamotrigine include a minimal effect on cognitive function compared to other anticonvulsants and a lower risk of developing ovarian cysts in patients or neural tube defects in a child from a mother with epilepsy than with other drugs [6–9].
Lamotrigine aggravates seizures in severe myoclonic epilepsy of infancy (Dravet syndrome) and is strictly contraindicated in this form. Isolated cases of increased myoclonus have been reported in juvenile myoclonic epilepsy, but this does not prevent the use of lamotrigine, along with valproate and topiramate, in this common form of epilepsy, especially in females.
Topiramate. Topiramate (Topamax) is considered one of the most promising anticonvulsants due to multiple mechanisms of action: blockade of voltage-gated sodium channels and voltage-gated calcium channels; enhancing the effect of GABA on GABAA receptors; blockade of excitatory mediators (glutamate); inhibition of carbonic anhydrase types II and IV [3].
The drug has been shown to have a neuroprotective effect in experimental status epilepticus [10]. Indications for the use of topiramate include most epilepsies and epileptic syndromes, with the exception of absence epilepsies: in this case, it is inferior to valproate. The effectiveness of topiramate in resistant forms of epilepsy is slightly higher than that of basic anticonvulsants [11, 12].
The disadvantages of topiramate include the need for slow titration of the dose (for children - no faster than 1 mg per kg of body weight per week). This titration is necessary to reduce the risk of side effects: hyperactivity, excitability, restlessness. On the other hand, slow titration allows you to more accurately select an individual dose, since the “therapeutic window” of the drug is very wide and control of attacks can be achieved either at a dose of 1 mg per kg of body weight per day or 10–15 mg per kg of body weight per day. The upper limit of the dose of topiramate is being specified and in children under 2 years of age it may be 20–25 mg per kg of body weight per day. During treatment with topiramate, it is necessary to monitor the condition of the kidneys.
Levetiracetam (Keppra). Like many new anticonvulsants, levetiracetam (there are several formulations of the drug on the market) was initially registered as a drug for the adjunctive treatment of cryptogenic and symptomatic partial epilepsies in adults. Subsequently, the drug turned out to be effective in idiopathic generalized epilepsy, including juvenile myoclonic epilepsy [13].
When studying the effectiveness of the drug in children, an increase in concentration was noted as a positive effect in 25% of cases. The most common side effects were excitability and aggressiveness [14].
The mechanism of action of levetiracetam remained unknown for a long time, but recently it was found that levetiracetam binds to the presynaptic protein SV2, located in synaptic vesicles. The function of the protein has not been fully elucidated, but the unique mechanism of action of levetiracetam and its structural similarity to piracetam explain the differences in the spectrum of action of levetiracetam and other new anticonvulsants. Levetiracetam, as monotherapy or in combination with piracetam, effectively relieved myoclonus in patients with Unferricht-Lundborg disease and other progressive myoclonic epilepsies [15–17]. Despite the fact that in Russia the drug is not registered for use in children, its earliest possible use both in progressive myoclonus epilepsy and in the treatment of children with non-progressive myoclonic status (Angelman syndrome, posthypoxic myoclonus) seems promising [15].
Rapid dose titration is possible, but to date the dosage limits in pediatrics have not been precisely defined, and there are also isolated reports of paradoxical reactions when taking high doses of levetiracetam.
In conclusion, it should be noted that today the anticonvulsant market in the Russian Federation offers a sufficient number of drugs for the treatment of most forms of epilepsy in children. A limiting factor is the high cost of treatment with new anticonvulsants. At the same time, niches for the use of drugs effective in certain forms of childhood epilepsy remain unfilled. This is vigabatrin (Sabril) - effective for West syndrome (infantile spasms), especially for tuberous sclerosis; sulthiam (ospolot) is a drug effective for syndromes combined with electrical status epilepticus of slow-wave sleep (Landau–Kleffner syndrome, etc.) and Rolandic epilepsy; Clobazam (Frisium), the benzodiazepine with the lowest degree of tolerance. Apparently, the issue of registration of these drugs in Russia should be raised by associations of neurologists and parent organizations.
A. Yu. Ermakov, Candidate of Medical Sciences Moscow Research Institute of Pediatrics and Pediatric Surgery, Moscow
For questions regarding literature, please contact the editor.
Analogues and substitutes of the drug
Structural analogues of Frisium are not produced by any pharmaceutical factory in Russia. In Europe and the USA, drugs with identical compositions are produced under the names Castilium, Clarmil, Frizin, Maginol, Sentil. Their import into our country is punishable by law. For the needs of medical institutions, active analogues of Frisium are produced, mainly benzodiazepine derivatives.
| A drug | Manufacturer | Active substance | Cost, in rubles |
| Clonazepam | REMEDICA | clonazepam | from 100 |
| Pregabalin | CJSC "Gedeon Richter-RUS" | pregabalin | from 350 |
| Gabapentin | PIK-PHARMA | pregabalin | from 400 |
| Hydroxyzine Canon | Pharmaceutical factory "Canon" | hydroxyzine | from 250 |
| Mezapam | JSC "Organika" | medoazepam | from 200 |
All drugs are substitutes for Frisium and often become the first choice in the treatment of seizures and mental disorders. They are relatively safe, but are also sold from pharmacies only after presenting a prescription from a doctor. Independent replacement of Frisium with analogues is fraught with severe complications.
What does the government intend to do about the problem?
After the summer events, it became impossible to ignore the situation. Prime Minister Dmitry Medvedev spoke on social networks about medications for children suffering from chronic diseases with pain and convulsions. According to him, manufacturers themselves do not register them in Russia.
Health Minister Veronika Skvortsova announced on September 13 that Sanofi will submit documents to register the drug Frisium. “Sanofi is ready to submit a dossier for registration within a month. Taking into account the fact that the drug has been in circulation for more than 20 years, this will be an accelerated, very fast registration without repeating clinical studies, using existing documents,” she promised.
Absolute and relative contraindications
An absolute contraindication to the use of Frizium is individual intolerance to clobazam or one of the auxiliary ingredients. The drug should not be used in the presence of the following pathological conditions:
- myasthenia gravis (muscle weakness);
- severe liver dysfunction;
- breathing problems, especially during sleep (apnea);
- spinal or cerebellar ataxia;
- acute intoxication with alcohol-containing drinks, sleeping pills, analgesics, antipsychotics, antidepressants.
The list of absolute contraindications also includes the first trimester of pregnancy and lactation. Frisium also has age restrictions - in pediatrics it is used in the treatment of children over 3 years of age. The drug should be used with caution in elderly patients. In the presence of chronic kidney pathologies, treatment with Frisium should be accompanied by constant monitoring of their functional parameters.
Legislative regulation of trade turnover
Why Frisium is banned in Russia - it’s all about the pronounced side effects of the benzodiazepine derivative. Even using it in strict accordance with the dosage regimen does not guarantee the absence of painful addiction. For addiction to form, 2-3 weeks of constant use of a sedative is often sufficient. Below are the side effects that explain why it is not available in pharmacy chains:
- suicidal thoughts;
- visual and auditory hallucinations.
Frisium is included in Russia in the list of substances with psychotropic activity that are in demand among people with drug addiction. If it is purchased, stored, transported or processed without proper permits from the Pharmaceutical Inspectorate, then Article 228 of the Criminal Code applies to violators. Selling the tranquilizer in pharmacies without a doctor's prescription is strictly prohibited.
In September of this year, some pharmaceutical factories were allowed to purchase Frisium in limited quantities.
But its distribution is possible only at the request of regional medical centers for pediatric needs. Deliveries of Frisium to Russia are still at the planning stage.
Is this medicine sold in Russia?
No. The medicine has lost its registration number and is no longer sold in Russia (previously, Frizium was part of the group of prescription drugs). To date, this drug has not been registered in the Russian Federation and does not have a license. It contains the substance clobazam, which is included in the third list of Russian Government Decree No. 681, which restricts or prohibits the circulation of narcotic drugs, their precursors and psychotropic substances on the territory of the Russian Federation.
Article on the topic Finding a cure for cancer. Will there be a breakthrough in oncology in Russia?
Proper Use
Compliance with the recommendations of the instructions for use of Frizium is mandatory. The optimal daily dose for the treatment of psycho-emotional instability and neuroses is 20 mg. It can be one-time or divided into 2-3 doses. For acute mental disorders, the treatment of which is carried out in a hospital, the dose is sometimes increased by 3-5 times. The best time to take Frisium tablets is before bed.
The dosage regimen is usually determined by the attending physician. It necessarily takes into account the type and severity of the disease, the severity of symptoms, the patient’s age, and the presence of chronic pathologies. When calculating single and daily dosages for children, the doctor also focuses on the weight and age of the child. The treatment of epilepsy has its own characteristics:
- the initial daily dose does not exceed 15 mg;
- it gradually increases to 80 mg;
- after the patient’s well-being improves, the dose is reduced to 20 mg.
The duration of the therapeutic course of Frizium varies from 4 weeks to several months. If necessary, treatment is resumed after a short break.
Specific side effects
The severity of the side effects of Frisium directly depends on the dosages used. For example, the use of more than 40 mg of a drug is often accompanied by speech disorders, diplopia, nystagmus, weight gain, decreased libido, and menstrual disorders. But the negative effect of the drug is possible even when taken in minimal doses. What are the side effects of a course of treatment with Frisium:
- fatigue;
- disturbances in concentration;
- slow mental and motor reactions;
- drowsiness;
- dry mouth;
- chronic constipation;
- anorexia.
Gastrointestinal disorders occur less frequently, including attacks of nausea, flatulence, and epigastric pain. Local adverse reactions resemble the symptoms of urticaria - rash, swelling and redness of the skin, itching, burning.
Frisium 10mg caps No. 30
Description
Active ingredient, group:
Clobazam, Antidepressant
Dosage form:
pills
Contraindications:
The use of Frisium is contraindicated in the following cases:
in children under 3 years of age, in patients with hypersensitivity to benzodiazepines and any excipients of the drug,
in patients in a state of acute poisoning with alcohol, sleeping pills, painkillers, antipsychotics, antidepressants, lithium salts,
in patients with drug or alcohol dependence (increased risk of developing dependence), in patients with myasthenia gravis (risk of worsening muscle weakness),
in patients with severe respiratory failure (risk of exacerbation), in patients with sleep apnea syndrome (risk of exacerbation),
in patients with spinal and cerebellar ataxia,
in patients with severe liver failure (risk of condensation encephalopathy),
during pregnancy and lactation.
Directions for use and dosage:
The drug is prescribed orally, regardless of food intake. The daily dose of Frisium for adults for the treatment of anxiety is 20-30 mg, usually divided into two doses, with the bulk to be taken in the evening.
To achieve optimal control of epileptic seizures in children and adult patients, it is recommended to begin treatment with low doses of the drug, followed by gradual titration to an effective dose.
Pharmachologic effect:
Frisium refers to psychotropic drugs, benzodiazepine derivatives, acting primarily on the central nervous system. Unlike antipsychotic drugs, it does not cause a pronounced antipsychotic effect.
It has anxiolytic, sedative, hypnotic, muscle relaxant and anticonvulsant effects.
Side effects:
Frisium can cause sedation, drowsiness, fatigue (especially at the beginning of treatment and when using high doses), slower reaction time, decreased excitability, confusion, headache, dizziness, muscle weakness, ataxia, tremor of the fingers; slow or slurred speech (articulation disorders), unsteadiness of gait and other motor dysfunctions, loss of sexual desire. These reactions usually occur due to the use of high doses of the drug or with long-term treatment and are reversible. With prolonged use, especially in elderly patients, signs of impaired consciousness may be observed, sometimes in combination with respiratory disorders.
Antegrade amnesia rarely occurs, especially when using high doses of the drug. This type of amnesia usually manifests itself in inappropriate behavior of patients.
When using Frisium, especially in old age, paradoxical reactions may occur in the form of anxiety, increased irritability, excitability, aggressiveness, difficulty falling asleep, acute agitation, delirium, fits of rage, nightmares, hallucinations, psychotic reactions, suicidal tendencies, frequent muscle spasms (to the point of convulsive seizures). If such reactions occur, treatment should be stopped immediately.
If the patient has a history of one or another form of depression, the use of the drug can significantly alleviate its course.
Tolerance and psycho-physical dependence can develop only with prolonged or uncontrolled use of the drug. It must be remembered that sudden cessation of therapy is not recommended due to the development of withdrawal syndrome.
Diplopia and nystagmus may occur. Such reactions usually develop when using high doses of the drug or with its long-term use and are reversible.
Frisium may cause respiratory depression, especially when administered in high doses.
From the gastrointestinal tract, dry mouth, constipation, decreased appetite, nausea, and sometimes vomiting are possible.
Isolated cases of skin reactions such as rash and urticaria have been observed. Very rarely - Stevens-Johnson syndrome, toxic epidermal necrolysis, including death.
Weight gain is possible, especially with high doses or with long-term treatment.
Special instructions:
When prescribing Frisium to patients with personality disorders, special care must be taken. This applies to patients who are depressed and people with suicidal tendencies, because the use of the drug aggravates these conditions.
Drinking alcohol is not recommended.
The occurrence of anterograde amnesia may occur.
Elderly patients may experience an increased tendency to various negative reactions that develop due to vascular insufficiency (drowsiness, dizziness, muscle weakness, changes in blood pressure), which requires dose adjustment of Frisium.
What should you pay attention to?
Soon Frisium will again be used in our country for medicinal purposes. Therefore, it is advisable to learn about its features in advance. Despite the effectiveness of the drug, there are also pitfalls in therapy. So, if there are no noticeable improvements after 2 weeks of therapy, you should inform your doctor. He will clarify the diagnosis and, if necessary, adjust the therapeutic regimen. The patient will be prescribed a drug with other active ingredients. Parents should constantly monitor the child’s well-being and consult a doctor if side effects become more severe.
Freesium is absolutely incompatible with alcoholic beverages. During treatment, it is necessary to refrain from driving a car or performing work that requires increased concentration. The tranquilizer should not be taken by people with suicidal tendencies, including a history.
How to get freesium, the Ministry of Health told parents
The Ministry of Health of the Russian Federation has approved instructions for parents whose children need unregistered psychotropic drugs. We publish the text of the document (see below). Previously, brief instructions on this topic were compiled by the Moscow Department of Health for families with seriously ill children living in the capital.
We are talking about drugs that are currently being purchased abroad to provide children in need under a temporary scheme. These are Diazepam (rectal solution), Clobazam (capsules, tablets), Midazolam (oromucosal solution), Phenobarbital (elixir, injection solution). In the future, it is planned to provide patients with these and other medicines on an ongoing basis by registering them or organizing the production of analogues in Russia.
The handout for parents consists of two parts. The first of them is intended for families who have already received a conclusion from a council at a federal medical institution about the child’s need for one of the specified medications. The second part contains instructions for parents (legal representatives) of children who have not yet received a consultation conclusion - but “apparently, need these drugs because the prescribed registered drugs or their combinations in various combinations for the treatment of epilepsy turned out to be ineffective and / or it is necessary use of a pediatric form of a psychotropic drug.”
For questions about which of the lists (the first or second section of the memo) the child is on, as well as to appeal the refusal, it is recommended to contact the local health authorities or Roszdravnadzor. The delivery of the first batch of medicines is expected in October, the Ministry of Health reported.
FOR PARENTS OF CHILDREN WHO NEED UNREGISTERED PSYCHOTROPIC DRUGS
Memo
Dear parents!
This memo consists of two sections. The first is for those parents (legal representatives) whose children already have a conclusion from a medical commission of a medical organization of a regional, municipal or private healthcare system and a protocol from a council of a federal medical organization on the need to prescribe psychotropic drugs unregistered in the Russian Federation - one or more of the following: Diazepam ( rectal solution), Clobazam (capsules, tablets), Midazolam (oromucosal solution), Phenobarbital (elixir, injection solution).
The second section is for parents (legal representatives) of children who, apparently, need these drugs because the prescribed registered drugs or their combinations in various combinations for the treatment of epilepsy have proven ineffective and/or the use of a pediatric form of a psychotropic drug (elixir) is necessary , rectal solution, oromucosal solution), but there are no conclusions of medical commissions and protocols of federal councils yet.
For parents (legal representatives) whose children have already undergone medical commissions from a medical organization of a regional, municipal or private healthcare system and consultations from a federal medical organization and confirmed the need to prescribe psychotropic drugs unregistered in the Russian Federation - Diazepam (rectal solution), Clobazam (capsules, tablets) ), Midazolam (oromucosal solution), Phenobarbital (elixir, solution for injection).
- After the first batch of drugs is imported into the Russian Federation (expected in October 2021), regional health authorities (regional ministries, health departments, health committees) will notify parents (legal representatives) in advance about the place and time of free distribution of drugs. If you and your child currently do not live at the address indicated in the conclusion of the federal council, you should inform the health authority of the region whose address is indicated in the conclusion in advance.
- To receive the drug, you must have a passport, a child’s birth certificate, and, if necessary, a document confirming that you are the child’s legal representative.
- Upon receipt of the drug (for one quarter), you will be asked to sign a receipt in duplicate stating that:
- You received the drug (drugs, if several are prescribed).
- You are warned that quality control of the drug (drugs, if several are prescribed) was not carried out on the territory of the Russian Federation.
- You are warned that the drug should be given to the child in accordance with the prescription specified in the protocol of the federal consultation.
- The drug should be stored in accordance with the instructions.
- The drug must not be transferred to other persons for use and (or) sold. In cases where a person illegally acquires, stores, transports, even without the purpose of sale, psychotropic drugs (depending on the size (weight) of the substance, the act entails administrative or criminal liability.
- If there is a balance of drugs, they should be transferred to the institution where you received the drug.
- If undesirable reactions occur or if the drug is ineffective, you must inform your doctor (local pediatrician, neurologist). It is also possible to send information about this by filling out the application form on the Roszdravnadzor website (https://www.roszdravnadzor.ru/services/people) or to the postal address: 109074, Moscow, Slavyanskaya Square, 4, building 1. This is very important , since the drug has not yet been registered.
- If you carry the drug with you, for example, when going to the country, have with you either the conclusion of the medical commission, or the protocol of the federal consultation, or the receipt indicated above.
- The drug is given for three months. Therefore, 2.5 months after receiving the drug, you should contact your doctor and inform about the need to receive the drug for the next three months, he will organize the transfer of this information to the regional health authority (regional ministry, health department, health committees), which will notify you in advance of the place and time of free distribution of drugs.
- During treatment with these drugs, the child should be under medical supervision.
For parents (legal representatives) of children who need these drugs, but there are no conclusions of medical commissions and protocols of federal councils yet.
- If your child is recommended one or more of the following unregistered psychotropic drugs - Diazepam (rectal solution), Clobazam (capsules, tablets), Midazolam (oromucosal solution), Phenobarbital (elixir, injection solution) you need to contact your local clinic or other a medical organization providing specialized medical care to children in the field of “neurology” or palliative medical care, to obtain the conclusion of a medical commission. If you think that the drug is indicated for a child because the prescribed registered drugs or their combinations in various combinations for the treatment of epilepsy turned out to be ineffective and/or the use of a pediatric form of a psychotropic drug (elixir, rectal solution, oromucosal solution) is necessary, then you You can also contact a clinic at your place of residence or another medical organization that provides specialized medical care for children in the field of “neurology” or palliative care, to decide whether there are medical indications for prescribing these drugs and to obtain an opinion from a medical commission if the drugs shown.
- If your child is already being observed in a federal clinic, then a medical commission and consultation may be held at the clinic regarding the prescription of these drugs to him, and the clinic must inform the regional health authority at the child’s place of residence about the fact of prescribing unregistered psychotropic drugs to him, indicating the name drug, dosage, method of administration and annual requirement.
- If necessary, the attending physician at the district clinic or other medical organization where the child is being observed may refer the child to a specialized medical organization, including a hospital, for additional examination (if necessary) and/or to consider whether your child has indications to the use of a psychotropic drug unregistered in the Russian Federation and dose selection.
- If there are grounds, the medical commission of the medical organization makes a decision on whether or not the child has medical indications for prescribing an unregistered psychotropic medication.
- You will be asked to sign a document agreeing to the processing of personal data, including sending it by email, since the protocol of the medical commission will be sent to the regional health authority and then to the Ministry of Health of the Russian Federation.
- The protocol of the medical commission (original or certified copy), containing the proposed treatment regimen for an unregistered psychotropic drug, indicating the release form, dosage and annual requirement, is sent to the ministry (department, committee) of health of a constituent entity of the Russian Federation, and from there to the Ministry of Health of the Russian Federation.
- The Ministry of Health of the Russian Federation sends the protocol of the medical commission to a federal medical organization with experience in treating severe forms of epilepsy in children to conduct an in-person or remote consultation of doctors. A council of doctors from a federal medical organization makes a final decision on prescribing a psychotropic medication to a child that is not registered in the Russian Federation and sends the protocol to the Ministry of Health of the Russian Federation.
- Within a month, the Ministry of Health of the Russian Federation collects protocols of medical commissions (federal councils) from all regions of the country, then sends them to the Ministry of Industry and Trade of the Russian Federation.
- The Ministry of Industry and Trade of the Russian Federation, if necessary, ensures the preparation of additional acts of the Government of the Russian Federation necessary for the import into the territory of the Russian Federation of a psychotropic drug not registered in Russia.
- FSUE "Moscow Endocrine Plant" imports medicines into the territory of the Russian Federation and delivers them to the regional authorized organization subordinate to the ministry (department, committee) of health of the subject of the Russian Federation in which the children to whom these drugs are prescribed live.
- The Ministry (department, committee) of health of a constituent entity of the Russian Federation notifies parents about the receipt of the drug, the place and time of its receipt. The procedure for obtaining the drug is described above.
- If you do not agree with the decision of the attending physician, you can seek help from the chief physician or deputy chief physician for clinical expert work.
For questions about which of the lists (the first or second section of the memo) your child is on, as well as in case of refusal to provide medications for medical indications, you can send a reasoned appeal to the executive authority in the field of health protection of the constituent entity of the Russian Federation , in which you live, or to Roszdravnadzor at the address: https://www.roszdravnadzor.ru/services/people), postal address: 109074, Moscow, Slavyanskaya Square, 4, building 1, or hotline phone number 8 800 550 99 03.
We wish you and your children health and prosperity!