In the early stages of pancreatic cancer, there are almost always no symptoms. In this regard, a malignant tumor can most often be detected only when the process progresses, which significantly complicates treatment and worsens the prognosis.
Manifestations of the disease are the same in women and men. There is no dependence on the gender of the patient: the symptoms of pancreatic cancer in women are no different from the health problems that occur in men. At the same time, their nature differs depending on the location, as well as the type of tumor: exocrine and endocrine tumors behave differently.
In 99% of cases, the lesion forms in the tissues of the exocrine part of the organ, whose task is to produce digestive enzymes and deliver them to the intestines.
Causes of pancreatic cancer, key risk factors
This is a small organ that is located in the abdominal cavity below the liver and behind the lower half of the stomach.
There are two types of cells in the gland: exocrine cells produce enzymes that help the body digest food, and endocrine cells produce hormones, including insulin, that help control blood glucose. Tumors form when damaged or mutated cells grow uncontrollably, divide and damage gland tissue and surrounding organs. Most malignant processes develop in exocrine cells. The exact cause and mechanism of how pancreatic cancer develops is unknown, but several risk factors are associated with the disease. These include:
- long history of smoking and drinking alcoholic beverages;
- obesity, especially with a BMI exceeding 30;
- having a close relative with pancreatic problems;
- diabetes (mainly type 2 Source: The relationship between diabetes mellitus and pancreatic cancer. Kashintsev A.A., Kokhanenko N.Yu. Siberian Journal of Oncology, 2013. pp. 36-39);
- chronic pancreatitis, especially in males Source: Chronic pancreatitis and pancreatic cancer. Lazebnik L.B., Vinokurova L.V., Yashina N.I., Bystrovskaya E.V., Bordin D.S., Dubtsova E.A., Orlova Yu.N. Experimental and clinical gastroenterology, 2012. p. 3-9.
The risk of developing signs of pancreatic cancer increases dramatically as you age. According to international statistics, 97.5% of all new diagnoses occur in people 45 years of age and older. Approximately 89% of all new diagnoses occur in people 55 years of age and older. 66.5% of all new cases are in people over 65 years of age.
Varieties
Oncologists distinguish two main types of pathology:
- exocrine form;
- endocrine form.
Depending on where the malignant tumor was localized, according to the examination, patients may be diagnosed with:
- head cancer, during which jaundice and skin itching develop;
- tail cancer;
- carcinoma of the gland body.
If you are concerned about the pancreas, the signs of cancer of the body of the gland and tail are in many ways similar to the manifestations of diabetes mellitus and chronic pancreatitis. With cancer of the body and tail, blood flow through the splenic vein is disrupted, as a result of which varicose veins of the stomach and esophagus are observed, and gastrointestinal bleeding develops.
The first symptoms do not allow one to accurately determine the location of the formation without examination using modern diagnostic equipment.
Pancreatic cancer: possible symptoms and warning signs
Sometimes the first symptoms of pancreatic cancer are atypical, mild and vague, similar to many other problems.
Pain (usually in the abdomen or back), weight loss, jaundice (yellowish discoloration of the skin and/or eyes) with or without itching, loss of appetite, nausea, bowel changes, pancreatitis and sudden onset diabetes are symptoms that may indicate pancreatic cancer. glands. If a patient experiences one or more of these symptoms, it is strongly recommended to immediately consult a doctor and undergo a diagnosis. Neuroendocrine tumors are rarely diagnosed, accounting for about 7% of all organ cancers. They can cause the pancreas to overproduce hormones. High levels of these hormones in the blood lead to symptoms such as weight loss, nausea, vomiting, muscle weakness and skin rashes. The very first signs of pancreatic cancer:
Bloating (ascites) is an abnormal accumulation of fluid in the abdominal cavity. Excess fluid causes swelling and bloating.
Pain syndrome, mainly in the upper abdomen or middle back, can be caused by the pressure of the tumor on the nerves or organs near the pancreas as the tumor grows into them. Pain may also occur if a tumor blocks the digestive tract.
Poor appetite, indigestion and nausea are common symptoms of pancreatic cancer. Some or all of these symptoms may occur when the tumor presses on the stomach or the beginning of the small intestine. In this case, food may remain in the stomach and cause some digestive problems, including nausea and vomiting. Symptoms of indigestion may also occur due to a blockage of the pancreatic duct through which enzymes flow, or due to changes in the activity of the organ.
Jaundice is a yellowing of the skin and eyes caused by excess bilirubin (a component of bile) in the blood. A tumor in the head of the pancreas can cause a narrowing of the bile duct and block the flow of bile from the gallbladder into the small intestine. A blocked bile duct causes bilirubin to accumulate. People with jaundice may also experience itchy skin, abnormally dark urine, and light-colored or clay-colored stools.
One of the manifestations of pancreatic cancer is intestinal symptoms and stool changes. Many patients with pancreatic cancer experience diarrhea, constipation, or both. Diarrhea – loose, watery, greasy stool with an unpleasant odor, can be caused by insufficient pancreatic enzymes in the intestines. This leads to malabsorption as undigested food quickly passes through the digestive tract. Constipation is also a common problem, especially in patients taking painkillers. These medications slow down the passage of food through the intestines. If the digestive system works too slowly, stools may become dry, hard, and difficult.
Acute weight loss (also known as cancer cachexia) is a complex problem that affects how the body uses calories and protein. Cancer cachexia can cause the body to burn more calories than usual, break down muscle, and reduce appetite. The person may also notice a change in appetite or desire to eat certain foods.
Cancer causes changes in the blood that can increase the chance of clots (blood clots) forming. Blood clots may go undetected and cause no symptoms. However, they are often associated with swelling, pain, and tenderness in the affected area.
Consequences and complications
Complications include:
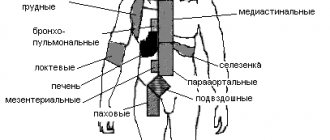
- Metastases to the lungs, lymph nodes and liver. Peritoneal metastases can compress the intestine and cause constipation or intestinal obstruction .
- The occurrence of thrombosis (with adenocarcinoma the risk is much higher than with squamous cell carcinoma).
- Stenosis and bleeding when the tumor grows into the stomach and duodenum.
- Hepatocerebral insufficiency , which is manifested by lethargy.
- Splenomegaly and bleeding from the veins of the esophagus when the tumor is located in the body or tail.
Types of pancreatic cancer
Experts identify several forms of pancreatic cancer. Exocrine cells, which make up the majority of pancreatic cells, are found in the glands and ducts of the organ. About 90% of all pancreatic cancers form in exocrine cells and are considered pancreatic adenocarcinomas. Adenocarcinomas are tumors that form in mucus-secreting glands.
About 5% of all pancreatic cancers form in endocrine cells and are considered neuroendocrine tumors (NETs). They are also called islet cell cancer because the endocrine cells are often found in clusters called islets.
Risks of occurrence
Scientists have not yet established the exact cause of pancreatic cancer. The growth of a malignant neoplasm can begin under the influence of the following provoking factors:
- Excessive smoking – causes ischemia (oxygen starvation) of organ tissue;
- Excess of easily digestible carbohydrates in the diet creates additional stress on the gland;
- Chronic pancreatitis - the development of atypical cells occurs against the background of an uncontrolled inflammatory process in the pancreas;
- Excess body weight - fat deposits affect internal organs, including the pancreas, and additional load increases the risk of developing tumors;
- Chronic intoxication – long-term toxic effects negatively affect the structure and functions of the pancreas;
- Oral diseases - caries, periodontitis, periodontal disease, which significantly increase the risk of the formation of tumor foci in the pancreas.
The highest incidence of pancreatic cancer is typical for economically developed countries, which are characterized by urbanization and high socio-economic indicators. Malignant neoplasms develop with a burdened heredity.
Tumor cells from other organs affected by the tumor process metastasize to the pancreas. More than 75% of patients with pancreatic cancer have reached 70 years of age. However, the pathology also affects younger people.
Expert opinion
Author:
Alexey Andreevich Moiseev
Oncologist, chemotherapist
Pancreatic cancer is a malignant tumor that develops in the glandular tissue or ducts of the organ. The tumor very quickly destroys tissue and grows into neighboring organs, so it is important to know the main symptoms of the disease in order to consult a doctor in a timely manner.
According to doctors, the main cause of the tumor is a genetic failure at the cellular level. As a result, the affected cells cannot perform basic functions, but multiply intensively, which leads to the formation of a tumor. Medicine is unable to find the root cause of oncology and answer the question of what gives impetus to the degeneration of healthy cells into cancerous ones. Research has been conducted for many years, but no clear cause of the pathology has been found.
Provoking factors are considered to be smoking, excessive alcohol consumption, diabetes mellitus, surgical interventions on the gastrointestinal tract, and poor environmental conditions.
Not a single doctor will answer you how long a patient will live or whether a patient will live at one or another stage of pancreatic cancer. It all depends on the severity of the pathology, the extent of the damage, and the state of the patient’s body. Doctors at the Yusupov Hospital practice an integrated approach to diagnosing and treating pancreatic cancer in a hospital setting.
Make an appointment
Stages of pancreatic cancer
After a diagnosis of pancreatic cancer is made, doctors will try to find out the stage. It describes how serious cancer is and how best to treat it. Doctors also use cancer stage when talking about survival statistics.
The earliest stage of pancreatic cancer is stage 0 (carcinoma in situ), followed by stages I (1) to IV. Typically, the lower the number, the less the cancer has spread. A higher number, such as stage IV, means the cancer is in the most advanced stage.
The most commonly used system for pancreatic cancer is the TNM system, which is based on 3 key pieces of information:
Tumor size (T): How big the tumor is and whether it has grown outside the pancreas into nearby blood vessels.
Spread to nearby lymph nodes (N): Whether the cancer has spread to nearby lymph nodes. If yes, how many lymph nodes are affected by cancer.
Spread (metastasis) to distant sites (M): Whether the cancer has spread to distant lymph nodes or distant organs, such as the liver, peritoneum (the lining of the abdomen), lungs, or bones.
Tumor architecture describes how cancer cells look like normal tissue under a microscope.
Level 1 (G1) means the cancer is very similar to normal pancreatic tissue.
Grade 3 (G3) means the cancer appears very abnormal.
Level 2 (G2) is somewhere in the middle.
Low-grade (G1) cancers tend to grow and spread more slowly than high-grade (G3) cancers. In most cases, grade 3 pancreatic cancer has a poor prognosis compared to grade 1 or 2 pancreatic cancer.
Possibility of resection. For patients, an important factor is the size of the resection – whether the entire tumor will be removed:
R0 : The cancer is considered completely removed. (There are no visible or microscopic signs indicating that cancer remains)
R1 : All visible cancer was removed, but laboratory tests of the removed tissue indicate that some small areas of cancer likely remain.
R2 : Some visible tumors could not be removed.
Forecast
Survival rates for patients with this pathology are very low due to the lack of diagnostic capabilities to detect the disease in its early stages. Despite the treatment, the prognosis for life expectancy for pancreatic cancer remains unfavorable. It all depends on the stage of the disease and the presence of gene mutations. In 80-90% of patients, the tumor turns out to be inoperable at the time of diagnosis (metastasis or invasion of nearby organs), which has a poor prognosis in the future. Survival also depends on the genetic profile. Tumors harboring DAXX or ATRX mutations are associated with poor prognosis. By studying the genetic profile, it is possible to identify in advance patients who need early and aggressive therapy. Expression of the SerpinB2 gene in the body of the gland in adenocarcinoma is not associated with metastasis, therefore such patients have long survival.
Treatment methods are also important in prognosis. After radical surgical treatment, survival rate does not exceed 15%, and the remaining patients die within 5 years after treatment. Therefore, the surgical method is supported by chemotherapy treatment. Combinations of several drugs significantly improve the prognosis.
How long can you live with pancreatic cancer? After surgical treatment, the prognosis remains unfavorable, since the relapse rate is 80-90%. Five-year survival after surgery is achieved by 25-30% of patients without metastases and only 10% of patients with metastases. If combined chemotherapy is administered after surgery, 29% of patients live 5 years. The type of tumor also affects life expectancy.
How long do people live with stage 4 pancreatic cancer? Since this stage is characterized by a metastatic process, the lifespan for stage 4 pancreatic cancer is 3-6 months. How do patients die? Departure from life is individual. Typically, patients develop severe pain that requires the prescription of narcotic drugs; all patients develop cachexia , which leads to protein-energy malnutrition. Protein deficiency reduces immunity, and the enzymatic function of the gland is further impaired. Decreased immunity increases the risk of infections. The presence of cachexia limits the ability to fully administer chemotherapy . Patients spend more time sleeping, and there is detachment, lethargy and apathy. We must try to organize good care for the sick to give them the opportunity to die peacefully.
Diagnosis of pancreatic cancer
Often in the initial stages there are almost no symptoms Source: Difficulties in diagnosing pancreatic cancer.
Evdokimova S.Yu. E-Scio, 2019. This may make diagnosis difficult. In addition to the examination and standard tests, you will need: An ultrasound scan is a painless procedure that uses high-frequency sound waves to create images of the body's organs. However, this type of scan can often miss the early stages of pancreatic cancer because the ultrasound waves do not always penetrate deep into body tissue well.
Computed tomography (CT) scans provide detailed images of internal organs using a series of X-rays. The doctor can use the results of the CT scan to check for abnormalities and estimate the size of the tumor.
Magnetic resonance imaging (MRI) also provides images of the gland, but uses strong magnetic and radio waves instead of X-rays. An MRI allows the doctor to check for signs of metastases.
A positron emission tomography (PET) scan can help show where the cancer is and whether it has spread throughout the body.
Endoscopic retrograde cholangiopancreatography is a procedure used to insert a plastic tube or stent into the bile duct for jaundice.
Laparoscopy is a surgical procedure that allows the surgeon to gain access to the inside of the abdomen and pelvis. During the procedure, a small incision is made in the abdomen and a laparoscope (a thin, flexible microscope) is inserted. This will allow the surgeon to look into the abdomen and make sure that the tumor has not spread before recommending its removal.
A biopsy involves taking a sample from a suspected tumor, which can then be tested to determine whether it is cancerous.
OTHER ISLE CELL TUMORS
Lipomas can cause diarrhea, “pancreatic cholera”, WDHA syndrome (water diarrhea, hypokalemia, achlorhydria), 50% of them are malignant. Glkzagonoma is characterized by skin lesions (necrolytic erythema migrans), diabetes, glossitis, anemia, weight loss, depression and venous thrombosis; 75% of glucagon are classified as malignant tumors. The best treatment is resection. Clinical manifestations of somatostatin include diabetes, diarrhea, steatorrhea, achlorhydria, gallstones, malabsorption and abdominal pain. All of these symptoms are attributed to excess somatostatin levels. Streptozocin, dacarbazine, and doxorubicin are most often used in treatment.
Consultation on paid services
Show phone numbers
Pancreatic cancer: treatment
The treatment regimen is drawn up taking into account the stages, size of the lesion and age, general condition and personal preferences of the patients.
The first goal will be to completely remove the tumor and any other cancer cells in your body. If this is not possible, the focus will be on preventing tumor growth while improving overall condition Source: Diagnosis and Treatment of Pancreatic Cancer. Patyutko Yu. I., Sagaidak I. V. Bulletin of the Russian Cancer Research Center named after. N. N. Blokhin RAMS No. 2, 2006. p. 36-37. There are three main methods of treatment:
- operation;
- chemotherapy;
- radiation therapy.
Some types of cancer in this location require only one form of treatment, while others may require two or a combination of all three.
Typically, surgery is the only way to completely cure pancreatic cancer. However, because the condition usually progresses by the time it is diagnosed, surgery is only suitable for about 15-20% of people.
This is not a suitable option if the tumor is localized around important blood vessels or has spread to other parts of the body.
Although surgery may not be an appropriate way to remove the tumor, doctors may suggest it to relieve symptoms. This type of surgery will not cure the cancer, but it will delay complications Source: Pancreatic Cancer: Indications for Surgery. Keck T. Medical Council, 2010. p. 65-68.
Chemotherapy is a type of cancer treatment that uses anti-cancer drugs that either kill cancer cells or stop them from multiplying. Chemotherapy treatment is often used along with surgery and radiation therapy to ensure that as much of the cancer as possible is treated.
Chemotherapy may be prescribed:
- before surgery - try to shrink the cancer;
- after surgery - to reduce the risk of cancer recurrence;
- when surgery is not possible, try to shrink the cancer, slow its growth and relieve symptoms.
Some chemotherapy drugs can be taken by mouth, but some must be given intravenously.
Radiation therapy is a form of cancer treatment that uses high-energy beams of radiation to shrink tumors and relieve pain.
General information
The pancreas is an organ of the human digestive system that simultaneously performs an exocrine function (secretes digestive enzymes) and an intrasecretory function (synthesis of hormones - insulin , glucagon , somatostatin , pancreatic peptide ). Malignant tumors of this organ can be localized in the endocrine and exocrine sections, as well as in the epithelium of the ducts, lymphatic and connective tissue. The ICD-10 code for pancreatic cancer is C25. Anatomically, the gland consists of parts - head, body, tail. The subheadings of ICD-10 include processes localized in various departments and have codes from C25.0 to C25.8. If we consider the anatomical localization of the tumor process, then more than 70% of all malignant tumors of the gland occur in the head. This is a disease of the elderly - its greatest incidence is at the age of 60-80 years and very rarely at the age of 40 years. Men get sick 1.5 times more often. The disease is more common in people who eat high-carbohydrate and fatty foods. In patients with diabetes, the risk of developing this disease doubles.
Pancreatic cancer remains the most aggressive and is characterized by extremely low patient survival. This is due to the fact that the malignant tumor is asymptomatic, difficult to diagnose and early metastasizes to the lymph nodes, lungs and liver, and also quickly spreads through the perineural spaces and grows into the duodenum and colon, stomach and large vessels. In 52% of patients, it is detected in late stages - at the time of diagnosis there are already liver metastases. Early diagnosis is often an impossible task. Even with regular ultrasound, it is not always possible to detect cancer at an early stage.
Over the past 40 years, there have been few advances in diagnosis and treatment that would improve this situation. Despite the improvement of the surgical method and the performance of extended operations, they do not show benefits at those stages at which this disease is detected. Despite its rare occurrence (compared to malignant diseases of other locations - lung, stomach, prostate, colon and breast), mortality from pancreatic cancer ranks fourth in the world. In this regard, research is aimed at finding methods for early diagnosis and the most effective chemotherapy .
Pancreatic cancer: prognosis for life
To develop treatment, doctors use a simpler staging system that divides cancers into groups based on whether they can be removed by surgery:
- operable cancer;
- border operability;
- inoperable (locally advanced or metastatic).
Operable cancer . When the lesion is located only in the pancreas (or has spread not far beyond), the treating surgeon considers that the entire tumor can be removed, this is called resectable. (Usually includes most TNM stage IA, IB and II A cancers.)
Borderline . This term is used to describe certain types of cancer that may have just reached nearby blood vessels, but which doctors believe can be completely removed by surgery.
Inoperable . These cancers cannot be completely removed by surgery. If the cancer has spread to distant organs, it is called metastatic (stage IV). These cancers cannot be completely removed. Surgery is still an option, but the goal will be to prevent or relieve symptoms rather than try to cure the cancer.
Tumor markers are substances that can sometimes be found in the blood due to cancer. CA 19-9 is a tumor marker that may be useful in therapy. Decreased CA 19-9 levels after surgery (compared to preoperative levels) and low CA 19-9 levels after pancreatic surgery often predict a better prognosis.
Classification
The first symptoms of the disease are difficult to notice. The choice of treatment depends on the type of cancer classified by stage. The stages of the disease are determined in patients after examination.
According to the TNM classification, the following stages are distinguished:
- the disease is localized, there are no lesions of the lymph nodes and internal organs - stage zero;
- the tumor has increased in size, but there are no lesions of nearby lymph nodes and organs - 1A and 1B;
- the tumor has spread beyond the organ, internal organs and lymph nodes are not affected - stage 2A. If internal organs and lymph nodes are affected - stage 2B;
- internal organs and lymph nodes are affected, cancer cells are present in the vessels – 3;
- disease with metastases in the abdominal organs – 4.
Prevention
The basis of prevention is maintaining a healthy lifestyle and eliminating all possible risk factors.
Article sources:
- Pancreas cancer. Foltz E.E. Bulletin of medical Internet conferences No. 3, 2021. p. 146-151
- Diagnosis and treatment of pancreatic cancer. Patyutko Yu. I., Sagaidak I. V. Bulletin of the Russian Cancer Research Center named after. N. N. Blokhin RAMS No. 2, 2006. p. 36-37
- Difficulties in diagnosing pancreatic cancer. Evdokimova S.Yu. E-Scio, 2019
- Pancreatic cancer: indications for surgery. Keck T. Medical Council, 2010. p. 65-68
- Chronic pancreatitis and pancreatic cancer. Lazebnik L.B., Vinokurova L.V., Yashina N.I., Bystrovskaya E.V., Bordin D.S., Dubtsova E.A., Orlova Yu.N. Experimental and clinical gastroenterology, 2012. p. 3-9
- Genetic aspects of pancreatic cancer. Grigorieva I.N., Efimova O.V., Suvorova T.S., Tov N.L. Experimental and clinical gastroenterology, 2014. p. 70-76
- Diagnosis and surgical treatment of pancreatic cancer. Norbert Hüser, Volker Assfalg, Daniel Hartmann, Daniel Reim, Alexander Novotny, Edouard Matevossian, Helmut Friess. Experimental and clinical gastroenterology, 2011. p. 102-111
- Results of surgical treatment of pancreatic cancer. Mikhailov I.V., Bondarenko V.M., Kudryashov V.A., Prigozhaya T.I., Podgorny N.N., Shimanovsky G.M., Starinchik V.I., Novak S.V., Atamanenko A. .V., Dovidovich S.V., Kravchenko O.V., Nesterovich T.N., Achinovich S.L. Problems of health and ecology, 2014. p. 46-51
- The relationship between diabetes mellitus and pancreatic cancer. Kashintsev A.A., Kokhanenko N.Yu. Siberian Journal of Oncology, 2013. p. 36-39
The information in this article is provided for reference purposes and does not replace advice from a qualified professional. Don't self-medicate! At the first signs of illness, you should consult a doctor.
GASTRINOMA
Clinical manifestations. The disease is characterized by the original Zollinger-Ellison triad: peptic ulcers with atypical localization and a fulminant, aggressive course, extreme hypersecretion of gastric contents and the presence of a non-P islet cell tumor of the pancreas. It can begin as a simple disease and end with the appearance of severe complications (perforation, obstruction, bleeding, refractoriness to therapy). Standard medical and surgical treatment is ineffective. There are cases accompanied by significant diarrhea and steatorrhea.
Diagnostics. Manifestations typical of gastrinoma include high basal secretion rates of VAO/MAO (= or >0.6), hypertrophied gastric mucosal folds, fasting hypergastrinemia (>200 pg/ml) or paroxysmal increase in gastrin levels in response to secretin administration, imaging pancreatic tumor using CT.
Pathology and pathophysiology. Gastrinomas are non-β islet cell tumors of the pancreas that range in size from 2 to 10 mm. There is varying evidence in the literature regarding the malignant potential of gastrinomas, although rates equal to or greater than 90% have been reported. The presence of gastrinomas in the wall of the duodenum is observed. Neoplasms grow slowly and metastasize late; The cause of death is often peptic ulcer disease. Cases of gastrinomas have been described as manifestations of MEA-1 syndrome (Wermer's triad: pituitary gland, parathyroid glands, pancreas), in which the tumors are distinguished by the fact that they are multiple and benign.
Treatment. The original treatment method is gastrectomy. However, the use of histamine H2 receptor blockers and omeprazole with or without proximal selective vagotomy can control the condition of patients with disease that cannot be resected.
When is chemotherapy needed?
Almost always, if the patient’s condition allows it. So after removing the cancer within 6 weeks, it is necessary to begin six-month preventive chemotherapy. If it is not possible to start chemotherapy within three months after pancreaticoduodenectomy and other radical interventions, it is abstained from it until a relapse occurs.
If this is not possible, long-term neoadjuvant chemotherapy is performed at the first stage of the operation, the effectiveness of which determines the likelihood of the operation. After successful resection at the second stage, chemotherapy continues for a total of 6 months; if six months of treatment has been exhausted before resection, then drug prophylaxis is abstained.
Relapse and treatment tactics
The possibility of pancreatic cancer recurrence depends on the stage at which the disease was detected and the quality of treatment provided. It is impossible to accurately predict the possibility of tumor recurrence. Relapse is influenced by various provoking factors.
After completing treatment, it is important to follow your doctor's recommendations and attend regular preventive examinations. The tactics for managing a patient with a recurrent tumor depends on its location, size and stage of development of the tumor focus. For this, the same methods are used as for the primary disease.