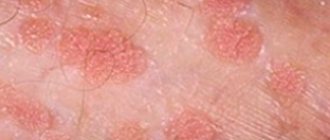
Signs of ichthyosis
Clinically, the disease is manifested by the formation of fish-like scales on the skin (which determined the name of the disease), white-yellow or gray-brown in color. The main problems faced by patients are dry, flaking and constant itching of the skin.
In severe cases, pathological dryness leads to the formation of bleeding cracks. The barrier function of the skin is impaired, which increases moisture loss. Accordingly, such patients have problems with thermoregulation and sweating. If damage to the epidermis occurs in the scalp, then, in addition to skin manifestations, there is excessive dryness and fragility of the hair, which subsequently leads to baldness.
In some forms of the disease, skin lesions are localized in the elbow and knee bends, on the face, which helps in diagnosis.
Clinical manifestations
The main symptom of ichthyosis - characteristic hard, scaly formations on dry skin - appears already in the first year of life, much less often - over the next few years. The child's skin becomes rough, and transparent, whitish or grayish scales appear on it, adjacent to each other. Only the elbow bends, the hollows under the knees and axillary areas, as well as the groin area remain clean. The palms and feet are peeling, and the skin pattern is clearly visible on them. In the mildest cases, the disease manifests itself only as slight peeling and dry skin.
Currently, there are more than fifty clinical and morphological forms of the disease, but in all cases the following manifestations are present:
- the stratum corneum of the epidermis is thickened, scaly formations and keratinization zones form on it;
- the skin is dry and flaky, the sebaceous glands practically do not work;
- the nail plates peel or break, in some cases they are deformed and resemble bird claws, peeling off from the soft tissues;
- the skin pattern becomes deeper and more expressive;
- There are rashes of different shapes and colors.
Skin ichthyosis usually worsens with the onset of cold weather. In warm weather, remission usually occurs. During puberty in adolescents, painful symptoms decrease, only to return in adulthood.
Causes of ichthyosis
It is worth noting that the disease is not infectious. It is not caused by viruses, bacteria, fungi, or parasites. It is not transmitted either through the air or through touch. Pathology is caused by mutations in genes. Moreover, it can be either congenital, inherited, or develop as a result of diseases of the blood, endocrine system (for example, hypofunction of the thyroid gland), or pathological deficiency of vitamins.
On the one hand, keratinization of the skin can be caused by a slowdown in the natural process of death of the outer layers, and on the other hand, by its increased growth.
Negative impact of the disease on the patient
Ichthyosis causes not only external harm, but also affects the processes and functions of the body:
- the functionality of the pancreas and adrenal glands is inhibited;
- the functioning of the gonads is disrupted;
- there is a lack of cellular immunity;
- vitamin A is not absorbed;
- spastic paralysis;
- oligophrenia;
- the functionality of the glands responsible for sweat production decreases;
- pain when trying to “clean” the skin;
- cardiac dysfunction in the body;
- mental retardation;
- Possible death.
Mortality among children with congenital ichthyosis is highest.
Classification of ichthyosis
Dermatologists identify 25 types of the disease, as well as a number of rare syndromes, where pathological changes in the skin are only one of the symptoms. The most common forms of ichthyosis:
- simple (vulgar);
- X-linked (linked to the X chromosome);
- lamellar.
Classification according to the nature of the scales:
- Simple (large scales, the disease affects large areas of the skin).
- Shiny or pearlescent (scales of the same color, lesions are very large).
- Serpentine (with thick, dense, rough scales, like the skin of a snake).
- Acicular (the scales look like needles or pins. This is the heaviest type).
- Black (scales with a dark color; mainly found in older people).
- Xeroderma (small scales, similar to bran - gray in color).
Ichthyosis vulgaris
The main clinical signs of the disease are peeling, increased folding of the palms and soles, and follicular hyperkeratosis.
Peeling is most pronounced on the extensor surfaces of the extremities; the skin of the back and abdomen and scalp are less affected. The scales are mostly small, thin, with wavy edges, their color varies from white and dark gray to brown. On the skin of the legs, the scales are the darkest and thickest, polygonal in shape, tightly attached. Follicular hyperkeratosis in the form of small dryish nodules at the mouths of hair follicles is observed on the skin of the thighs, shoulders, forearms and buttocks, and can also be localized on the skin of the torso and face. When palpating the affected areas, the “grater” syndrome is determined. The palms and soles have an accentuated pattern and increased folding, which gives them an aged appearance. In summer, painful cracks often appear on the soles. The nail plates are brittle, crumble from the free edge, and sometimes onycholysis develops. Hair thins and becomes sparse.
The expressiveness of vulgar ichthyosis is variable. There are abortive forms of the disease, which are characterized by dry skin with slight peeling and increased folding of the palms and soles.
The disease is characterized by the following symptoms:
- The presence of ichthyosis in the patient’s 1st and 2nd degree relatives.
- The appearance of clinical symptoms in the first year of life (3–7 months) or later (up to 5 years).
- Clear seasonality with improvement in summer and increased clinical manifestations in winter.
- Association with allergic diseases: patients with ichthyosis vulgaris are prone to allergic diseases and atopy. The frequency of combination with atopic dermatitis reaches 40–50%. Manifestations of bronchial asthma, vasomotor rhinitis, and urticaria may occur simultaneously. Characterized by intolerance to a number of foods and medications.
- Association with diseases of the gastrointestinal tract (gastritis, enterocolitis, biliary dyskinesia), cryptorchidism or hypogenitalism is less common (in 3% of patients). Patients are prone to pyococcal, viral and fungal infections.
X-linked ichthyosis
Immediately after birth or in the first weeks of life, dry skin is noted. Later, light and dark brown scales appear on the extensor surfaces of the limbs. The back surface of the neck takes on a “dirty” appearance due to the accumulation of scales. The armpits, elbow fossae and genital area are free of lesions. A distinctive feature from other forms of ichthyosis is the absence of “glove”-type lesions on the skin of the face and hands.
The disease is characterized by the following symptoms:
- The presence of ichthyosis in the patient’s 1st and 2nd degree relatives. Only males are affected. Women are heterozygous carriers of the defective gene and have no clinical manifestations of the disease.
- The appearance of clinical symptoms from birth or from the first weeks of life.
- Weak seasonality, but most patients note an improvement in their skin condition in the summer.
- Absence of associations with atopic dermatitis and respiratory atopy in most patients.
- Clouding of the cornea without visual impairment (in 50% of patients), cryptorchidism (in 20% of patients).
Lamellar ichthyosis
Generalized lamellar peeling is noted, simultaneously with which palmoplantar hyperkeratosis is necessarily observed, which is a constant clinical sign of the disease. The scales on smooth skin are usually small and light, but on the legs they are large and form lamellar peeling. Some patients experience deformation of the ears.
The disease is characterized by the following symptoms:
- The presence of ichthyosis in the patient’s 1st and 2nd degree relatives.
- The appearance of clinical symptoms from birth: the fetus is born in a colloidal film or a state of generalized erythroderma, then by 6–7 months after birth, generalized lamellar desquamation develops.
- Absence of physical and mental development disorders in patients.
- Lack of seasonality.
Congenital bullous ichthyosiform erythroderma
In the area of large natural folds (knee, elbow, wrist and ankle joints, on the cervical folds, in the area of the armpits) hyperkeratosis with large lamellar horny crumb-like formations is observed. Foci of hyperkeratosis are brown, brown-black or dirty gray in color. Against the background of hyperkeratosis, blisters with serous contents initially appear, followed by a secondary infection.
At the same time, there is an increase in body temperature and an increase in regional lymph nodes. When the horny layers are rejected, eroded lesions with noticeable papillary growths remain. An unpleasant odor is characteristic due to the frequent addition of a secondary infection.
The disease is characterized by the following symptoms:
- The presence of ichthyosis in the patient’s 1st and 2nd degree relatives.
- The appearance of clinical symptoms from birth: at birth, the child’s skin looks macerated, soon after birth the skin becomes dry, and in large natural folds it becomes rough and coarse.
- Seasonality of exacerbations of the disease: the appearance of blisters and the subsequent addition of infection is usually observed in autumn and spring.
Fetal ichthyosis
The lesion covers the entire skin in the form of a continuous, varying thickness of horny shell of whitish-yellow or grayish-brown color, which cracks and deep grooves form on the articular surfaces. There is a thick layer of horny layers on the patient’s head, the existing hair is short, sparse or completely absent. The face is deformed and covered with large horny plates. The mouth is wide open due to severe infiltration of soft tissues; deep cracks are visible in the corners of the mouth. The lips are thickened, their mucous membrane is everted, there is a pronounced ectropion and sparse eyelashes. The ears are deformed and pressed tightly against the skull or folded forward. In the nostrils and ear canals, horny layers in the form of plugs are detected.
The disease is characterized by the appearance of clinical symptoms from birth: at birth, the child’s skin resembles a rough, dry, horny shell of a grayish-whitish or lilac color, which begins to darken in the first hours after birth. Newborns are born premature in 80% of cases.
Ichthyosis in children
As a rule, the disease manifests itself at birth. In severe cases (for example, harlequin ichthyosis), the child is born prematurely and dies in the first days. However, the pathology can manifest itself in the second or third month of life, and sometimes the first manifestations occur at the age of 5 years. With moderate severity, this pathology is compatible with life.
If we talk about the gender of patients, it is worth noting that girls are carriers of the mutated gene, but mostly boys suffer from this pathology. Girls get sick in rare cases - for this to happen, two X chromosomes with the affected genes from both the mother and the father must match. In this case, the disease is very severe and can lead to the death of the child.
Against the background of the disease, pathological changes in other organs and systems are observed. These children are often diagnosed with:
- corneal clouding.
- epilepsy,
- disruption of the development of the skeleton and other organs,
- mental retardation.
Treatment of ichthyosis
Today the disease is incurable. The main goals are to alleviate the patient’s condition, eliminate symptoms and prevent exacerbations. The basic principles of therapy are reducing skin moisture loss, intensively moisturizing it with the help of anti-ichthyosis products, and controlling the thickness of the stratum corneum. Treatment is prescribed by a dermatologist and selected individually.
The enemies for patients are high temperature and dry air (including in winter). It is important to prevent overheating of such patients (in summer, use special sprays with water to moisturize the skin).
In addition, it is recommended to take baths for 10-20 minutes 1-7 times a week (depending on the degree of keratinization). Alternating baths with the addition of essential oils, soda (50-150 g per bath), rice, wheat or corn starch has worked well. After softening the skin using special mittens or silk rags, it is necessary to gently exfoliate. Before wiping, apply skin softening agents (emollients).
To improve exfoliation (desquamation) in hyperkeratosis, keratolytic agents are used: ichthyosis creams, ointments and lotions. Such products contain urea (Carboderm, Prednicarb), salicylic acid (Betasalik, Kerasal), propylene glycol. Once applied to the affected areas, they can be left uncovered or covered with a bandage. The use of the latter enhances the effectiveness of keratolytics, however, when large areas of skin are affected, occlusion is inappropriate, since it leads to an increase in body temperature, and in such patients thermoregulation is already impaired.
Prescribing keratolytics for the treatment of children with ichthyosis is possible only under the supervision of a physician. The concentration of the active substance is determined by the age range and severity of the disease.
If large areas of skin are affected, salicylic acid preparations should be used with caution, as this can lead to intoxication of the body (nausea, shortness of breath, tinnitus, etc.)
For preventive purposes, to improve skin condition, it is recommended to use products containing vitamins A and D3.
The use of antiseptics is indicated for treating cracks.
Frequently asked questions about ichthyosis
How is ichthyosis inherited from sick parents?
The disease ichthyosis is hereditary. Pathology is caused by mutation of genes on the X chromosome, so girls are carriers, and boys are most often affected.
Is ichthyosis transmitted during contact with a sick person?
No. Ichthyosis is not an infectious disease. They cannot be contracted through contact with sick people. The pathology is caused by gene mutation.
How do people with ichthyosis live?
The disease requires constant skin care. The main tasks are to reduce moisture loss, intensively moisturize the skin, and control the thickness of the stratum corneum. Due to impaired thermoregulation in such patients, it is important to avoid overheating and prolonged stay in rooms with dry air.