Neupomax
Treatment with the drug should be carried out only under the supervision of an oncologist or hematologist with experience in the use of such drugs, if the necessary diagnostic capabilities are available. Cell mobilization and apheresis procedures should be performed in specialized centers with experience and the ability to adequately control progenitor cells.
During treatment, the number of leukocytes and the cellular composition of the bone marrow should be monitored.
The drug solution is prepared no earlier than 24 hours before administration and is stored at a temperature of 2-8 degrees C.
The effectiveness and safety of the drug for the mobilization of PSCC in healthy donors younger than 16 and older than 60 years for allogeneic transplantation have not been studied.
Human granulocyte colony-stimulating factor can stimulate the growth of myeloid cells in vitro and in relation to non-myeloid cells. The safety and effectiveness of use in myelodysplastic syndrome and chronic myeloid leukemia have not been established. Particular attention should be paid to the differential diagnosis between blast transformation of chronic myeloid leukemia and acute myeloid leukemia.
Patients receiving cytotoxic chemotherapy: in less than 5% of patients receiving treatment at a dose of more than 0.3 million units (3 mcg) / kg / day, the number of leukocytes increased to 100 thousand / μl or more. There were no reported side effects associated with this. However, given the possible risk associated with severe leukocytosis, the white blood cell count should be determined regularly during treatment. If, after passing the expected minimum, it exceeds 50 thousand/µl, the drug should be discontinued immediately. If the drug is used to mobilize PSCC, it is discontinued if the number of leukocytes exceeds 100 thousand/μl.
Particular caution should be exercised when treating patients receiving high-dose chemotherapy, since improvement in the outcome of malignant neoplasms has not been shown, while high doses of chemotherapy have more pronounced toxicities, including cardiovascular, pulmonary, neurological and dermatological reactions.
Monotherapy with the drug does not prevent the development of thrombocytopenia and anemia caused by myelosuppressive chemotherapy. Due to the possibility of using higher doses of chemotherapy drugs (eg, full doses according to regimens), the patient may be at greater risk of thrombocytopenia and anemia. It is recommended to regularly determine the platelet count and hematocrit. Particular caution should be exercised when using single-component or combination chemotherapy regimens that can cause severe thrombocytopenia.
The use of PSCC mobilized with the drug reduced the severity and duration of thrombocytopenia after myelosuppressive or myeloablative chemotherapy.
Particular care should be taken when diagnosing severe chronic neutropenia to differentiate it from other hematological diseases such as aplastic anemia, myelodysplasia and myeloid leukemia. Before starting treatment, a detailed blood test should be performed to determine the leukocyte formula and platelet count, as well as examine the morphological picture of the bone marrow and karyotype.
Myelodysplastic syndrome (MDS) and leukemia have been observed in a small number (3%) of patients with severe congenital neutropenia (Kostmann's syndrome) treated with the drug. MDS and leukemia are natural complications of this disease. Their relationship to drug treatment is unclear. In approximately 12% of patients with initially normal cytogenetics, anomalies were discovered during re-examination, incl. monosomy 7. If a patient with Kostmann's syndrome develops cytogenetic abnormalities, the benefits and risks of continuing therapy must be carefully assessed. If MDS or leukemia develops, the drug should be discontinued. It is not yet clear whether long-term treatment with the drug predisposes patients with severe congenital neutropenia (Kostmann syndrome) to the development of cytogenetic abnormalities, MDS and leukemia. Patients with Kostmann syndrome are recommended to undergo morphological and cytogenetic studies of the bone marrow at regular intervals (every 12 months).
During the treatment period, it is necessary to carefully monitor the platelet count, especially during the first few weeks of treatment with the drug. If thrombocytopenia develops (platelet count is consistently below 100 thousand/µl), temporary discontinuation of the drug or dose reduction should be considered. There are also other changes in the blood count that require careful monitoring, incl. anemia and a transient increase in the number of myeloid progenitor cells.
Causes of transient neutropenia such as viral infections should be excluded. An enlarged spleen is a direct consequence of treatment with the drug. During clinical studies, 31% of patients with severe chronic neutropenia had splenomegaly on palpation. X-ray examination revealed an enlarged spleen soon after the start of treatment and tended to stabilize. It was found that dose reduction slowed or stopped splenomegaly; 3% of patients required splenectomy. The size of the spleen should be monitored regularly. To detect splenomegaly, it is enough to palpate the abdomen.
Hematuria and proteinuria were observed in a small number of patients. Urinalysis should be monitored regularly.
The safety and effectiveness of the drug in newborns and patients with autoimmune neutropenia have not been established.
Mobilization: There are no prospective randomized trials comparing the two recommended mobilization methods (filgrastim alone or in combination with myelosuppressive chemotherapy) in the same patient population. The degree of discrepancy between individual patients and laboratory CD34+ cell count results indicates that direct comparisons between different studies are difficult. Therefore, it is difficult to recommend an optimal method. The choice of mobilization method should be made depending on the overall goals of treatment for a given patient.
Previous treatment with cytostatic drugs: in patients who have had a history of active myelosuppressive therapy, there may not be sufficient activation of PSCC to the recommended minimum value (more than 2 million CD34+ cells/kg) or acceleration of normalization of platelet counts.
Some cytostatics are particularly toxic to hematopoietic progenitor cells and may negatively affect their mobilization. Drugs such as melphalan, carmustine and carboplatin, if prescribed for a long time before attempting to mobilize progenitor cells, may reduce its effectiveness. However, their use simultaneously with the drug turned out to be effective in activating progenitor cells. If peripheral progenitor cell transplantation is planned, it is recommended that stem cell mobilization be planned early in the course of treatment. Particular attention should be paid to the number of progenitor cells activated in such patients before high-dose chemotherapy. If mobilization results according to the above criteria are insufficient, alternative treatments that do not require the use of progenitor cells should be considered.
When assessing the number of progenitor cells mobilized in patients using the drug, special attention should be paid to the quantification method. Results from flow cytometric analysis of CD34+ cell counts vary depending on the specific methodology; Caution should be exercised in making recommendations based on studies from other laboratories.
Statistical analysis of the relationship between the number of CD34+ cells administered and the rate of platelet count normalization after high-dose chemotherapy indicates a complex but stable relationship.
Currently, the minimum value for the increase in CD34+ cells has not yet been sufficiently determined.
Neipomax, 30 million units/ml, solution for intravenous and subcutaneous administration, 1 ml, 5 pcs.
Neupomax® can be administered by daily subcutaneous (SC) injection or daily short (30-minute) intravenous (IV) infusion. The drug can also be administered as a 24-hour intravenous or subcutaneous infusion.
The choice of route of administration should depend on the specific clinical situation, but in most cases the subcutaneous route of administration is preferred.
To avoid pain during injection, it is best to change the injection site daily.
Standard cytotoxic chemotherapy regimens
5 mcg/kg body weight 1 time per day daily subcutaneously or intravenously for 30 minutes until, after the expected maximum decrease in the level of neutrophils, their number is restored to normal, upon reaching which the drug can be discontinued .
The first dose of Neipomax® should be administered no earlier than 24 hours after the end of the course of cytotoxic chemotherapy. Duration of therapy is up to 14 days. After induction and consolidation therapy for acute myeloid leukemia, the duration of use of Neipomax® may increase to 38 days, depending on the type, dose and chemotherapy regimen used.
Typically, a transient increase in the number of neutrophils is observed 1-2 days after the start of treatment with filgrastim. To achieve a stable therapeutic effect, interrupting treatment until normal neutrophil values are achieved after the expected maximum decrease in their level is not recommended. When the absolute number of neutrophils exceeds 10,000/μl, treatment with Neypomax® is stopped.
Myeloablative therapy
by
autologous or allogeneic bone marrow transplantation.
Initial dose: 10 mcg/kg per day intravenously over 30 minutes or 24 hours, or as a 24-hour subcutaneous infusion.
The first dose of Neipomax® should be administered no earlier than 24 hours after cytotoxic chemotherapy, and in case of bone marrow transplantation - no later than 24 hours.
The duration of therapy is no more than 28 days. The daily dose of the drug is adjusted depending on the dynamics of neutrophil content. If the absolute neutrophil count is more than 1000 / μl for three consecutive days, the dose of Neipomax® is reduced to 5 μg / kg / day. If, when using this dose for another 3 days in a row, the absolute number of neutrophils exceeds 1000/μl, the administration of Neipomax® is stopped. If during treatment the absolute number of neutrophils decreases to a level of less than 1000/μl, the dose of Neipomax® is increased again in accordance with the above scheme.
Mobilization of peripheral blood stem cells in patients with tumor diseases
10 mcg/kg 1 time per day subcutaneously or by continuous 24-hour subcutaneous infusion for 6 consecutive days. In this case, 2 leukapheresis are usually performed in a row, on the 5th and 6th days. In case of additional leukapheresis, the administration of Neipomax should be continued until the last leukapheresis.
Mobilization of PSCC after myelosuppressive chemotherapy
5 mcg/kg per day by daily subcutaneous injection, starting from the first day after completion of chemotherapy until the number of neutrophils reaches normal values.
Leukapheresis should only be performed when the absolute neutrophil count exceeds normal values (>2000/µl).
Mobilization of PSCCs from healthy donors for allogeneic transplantation
10 mcg/kg/day subcutaneously for 4–5 days and 1 or 2 leukapheresis usually allows to obtain more than 4 × 106 CD34+ cells/kg body weight of the recipient. There are no data on the safety and effectiveness of filgrastim in healthy donors under 16 and over 60 years of age.
Severe chronic neutropenia (SCN)
Neipomax® is prescribed at an initial dose of 12 mcg/kg/day for congenital neutropenia and 5 mcg/kg/day for idiopathic or periodic neutropenia, subcutaneously once or by multiple injections daily until the neutrophil count consistently exceeds 1500/mcL. After achieving a therapeutic effect, the minimum effective dose is determined to maintain this level. After 1–2 weeks of treatment, the initial dose can be doubled or halved, depending on the patient's response to therapy. Thereafter, individual dose adjustments can be made every 1–2 weeks to maintain the mean neutrophil count in the range of 1500–10000/μL. In patients with severe infections, a more rapid dose escalation regimen may be used. The safety of filgrastim in long-term treatment of patients with SCN with doses greater than 24 mcg per day has not been established.
Neutropenia in HIV infection
The initial dose is 1–4 mcg (0.1–0.4 million IU)/kg subcutaneously once a day until the number of neutrophils normalizes. The maximum daily dose should not exceed 10 mcg/kg. After achieving a therapeutic effect, it is recommended to use Neipomax® in a maintenance dose: 300 mcg subcutaneously every other day. Subsequently, doses are adjusted on a case-by-case basis to maintain an average neutrophil count greater than 2000/µl.
Application in pediatric practice
Dosing recommendations for pediatric patients are the same as for adults.
Elderly patients, patients with impaired renal or hepatic function
No dose adjustment of Neypomax® is required.
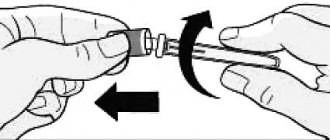
Breeding instructions
When administered subcutaneously, the drug should not be further diluted.
When preparing a solution for infusion, Neipomax® is diluted with only a 5% dextrose solution. Dilution with 0.9% sodium chloride solution is not allowed (pharmaceutical incompatibility).
Neipomax® in diluted form at a concentration of 2 to 15 μg/ml can be adsorbed by glass and plastics. In this case, to prevent absorption, it is necessary to add human serum albumin to the solution in the required amount to achieve its concentration in the final solution of 2 mg/ml. For a diluted solution of Neipomax® at a concentration of more than 15 mcg/ml, the addition of albumin is not required.
Neipomax® cannot be diluted to a concentration of less than 2 mcg/ml.