Home » Services for women » Gynecology » Treatment of vulvitis in women
Vulvitis is an inflammatory process that affects the external genitalia of girls and women. The symptoms of the disease are unpleasant - pain during sexual intercourse or urination, burning, heavy vaginal discharge, swelling and itching. Often this pathology is caused by improper hygiene and hormonal imbalances.
Vulvitis in women with timely started therapy practically does not cause complications. If the disease occurs in a girl at an early age, it often provokes the development of a pathology such as fusion of the labia minora.
Symptoms of inflammation of the labia
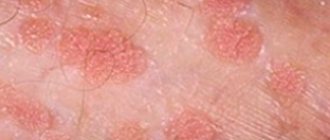
The inflammatory process in the area of a woman’s external genitalia (vulva) is referred to in gynecology as “vulvitis.” This condition has characteristic symptoms, such as redness, itching, swelling of the labia, painful symptoms when urinating, and copious natural female discharge. A woman may also experience a number of additional symptoms:
- the appearance of roughness of the labia minora, which is nodules of enlarged sebaceous glands;
- the appearance of a whitish coating, plaques reminiscent of psoriasis rashes;
- feeling of general malaise and fever.
Like any other inflammatory process, vaginitis is divided into acute and chronic. The acute form is characterized by pronounced symptoms, while the chronic process is more sluggish and unnoticeable.
Expert opinion
You should be especially careful about the development of vulvitis in little girls, since children tend to hush up problems associated with discomfort in the intimate area. For this reason, it is necessary to make it clear to the child that if he experiences any unpleasant sensations, he must inform his elders about their occurrence.
Obstetrician-gynecologist of the highest category Oksana Anatolyevna Gartleb
Gynecologist appointment
Causes of vulvitis
In order to clearly understand the causes of vulvitis, it is worth dividing this disease into 2 types: primary and secondary. Primary vulvitis develops in the case of:
- Failure to comply with the rules of intimate hygiene (irregular washing, rarely changing tampons and pads during menstruation, rarely changing underwear, wearing tight and synthetic underwear).
- Sudden hypothermia or overheating of the body.
- Mechanical damage to the vulvar mucosa during sexual intercourse, constant use of tight clothing made of coarse fabrics, removal of hair, and combing.
- Chemical exposure to various drugs.
- Hormonal imbalance and metabolic disorders (obesity, diabetes, insufficient ovarian function, lack of vitamins and minerals in the body);
- Allergic reactions.
Secondary vulvitis, vulvovaginitis (Vulvovaginitis) occurs due to infection of the external genitalia by pathogenic microorganisms contained in vaginal discharge.
Vulvitis - causes
Irritation of the labia can be caused by thrush, colpitis (Vaginitis), endometritis (Endometritis) and other diseases of various organs, not necessarily directly related to the mucous membranes and skin of the genitals. It is worth noting that long-term or frequent use of antibiotics can cause disruption of the vaginal microflora and subsequent vulvitis.
Inflammation of the labia - vulvitis
As medical statistics show, secondary vulvitis most often occurs in women of reproductive age, while primary inflammation is more often diagnosed in childhood. This is facilitated by the tendency of children to diathesis, helminthiasis (Helminthosis) (pinworms with improper hygiene can get into the labia area, causing an inflammatory process).
In this case, vulvitis in girls can be complicated by the appearance of synechiae, which are adhesions connecting the labia minora.
Vulvitis can occur during pregnancy, especially if a woman does not follow the rules of intimate hygiene or wears inappropriate underwear. Vulvitis can occur after childbirth. As the fetus passes, the vagina and labia are injured, which can cause subsequent inflammation.
Vulvovaginitis
Vulvovaginitis is a disease of the female genital organs.
Inflammation may be of bacterial origin or be the result of mechanical irritation of the vulvar and vaginal mucosa. The natural structure of the female body allows us to protect the genitals from microorganisms from the external environment. The vaginal microflora of a healthy woman easily inhibits the growth of opportunistic bacteria that live on the mucous membranes. A decrease in immunity due to stress, intoxication or a viral disease can provoke a surge in the activity of pathogens, resulting in the development of acute vulvovaginitis.
Diagnosis of vulvitis
To diagnose vulvitis, in most cases, a simple manual examination by a doctor is sufficient, as well as taking a smear for bacteriological, bacterioscopic and cytological examination. The results obtained allow us not only to determine the presence of inflammation, but also to exclude malignant tumors and identify the causative agent of the infection. Additionally, the doctor may prescribe a stool test to detect helminthiasis.
Appointment with a doctor for the treatment of vulvitis
A detailed description of the symptoms and the initial stage of the disease will also have diagnostic value for the doctor. This will simplify the diagnosis and make it possible to exclude any concomitant infections. After all, the itching that vulvitis causes leads (especially often in girls) to the appearance of scratching in the area of the external genitalia, which may also indicate the presence of diseases such as pediculosis, dermatitis or lichen. Also, the cause of itching in the labia area can be any sexually transmitted disease, which sometimes may require consultation with a dermatovenerologist or additional diagnostics.
What complications can there be?
Untreated vulvovaginitis can lead to serious consequences. In girls, the formation of dense adhesions of the labia minora is possible. Such a deformation will make sexual life difficult. In addition, this pathology is one of the factors that provoke cystitis.
The disease is especially dangerous during pregnancy. The expectant mother is at risk of spontaneous abortion, endometritis, or the birth of an infected baby.
Chronic vulvovaginitis leads to hardening of the mucous membranes. With this course, cracks and erosions occur more often, and prerequisites for the appearance of oncology appear.
Treatment of vulvitis
If you notice any alarming symptoms, you should immediately consult a doctor. Only a specialist can diagnose the cause and prescribe correct and quick treatment, including a set of measures: relieving inflammation, eliminating factors that are catalysts for the process.
The basis of treatment for vulvitis is the elimination of the causes of the inflammatory process and treatment of concomitant diseases, which may include diabetes mellitus (Diabetes mellītus), gonorrhea (Gonorrhoea), diphtheria (Diphtheria), helminthiasis. After receiving smear test data and checking the sensitivity of the infectious agent, the doctor can prescribe medication, most often antibacterial drugs. Vulvitis responds well to treatment with local remedies, which include all kinds of ointments, gels and suppositories.
In parallel, in the course of treatment of vaginitis, vitamin complexes can be prescribed, including vitamin A to effectively protect the epithelial layer, as well as vitamins E and C, known for their antioxidant properties.
To combat severe symptoms, other drugs may be prescribed:
- Antihistamines that help relieve itching.
- Hormonal, occurring in atrophic vulvitis in the postmenopausal period.
- Anesthetics that relieve pain.
In addition to the medications prescribed by your doctor, you can use Gynocomfort Restoring Gel. This product was created by specialists from the pharmaceutical company VERTEX and underwent clinical trials at the Department of Dermatovenerology with the clinic of the St. Petersburg State Medical University. During testing of the gel, it was proven that it is a very effective additional agent as part of the complex therapy of inflammatory processes of the female genital tract.
As additional therapeutic measures that can be used at home, it is worth mentioning warm baths with herbal infusion.
Chamomile, calendula, string, and comfrey have excellent anti-inflammatory properties.
Baths will help not only reduce inflammation, but also relieve symptoms such as itching, burning and pain.
Prevention of inflammation of the labia
To prevent vulvitis, it is necessary, first of all, to maintain intimate hygiene. It is recommended to use products designed specifically for caring for intimate areas. Ginocomfort washing gels for intimate hygiene, which were developed by specialists of the pharmaceutical company VERTEX, taking into account the characteristics of the microflora of the genital organs, are well suited for this purpose. They do not dry out the mucous membrane and do not disturb the acid-base balance. These products have a package of necessary documents and quality certificates.
Other measures to prevent inflammatory processes in the labia area include the following:
- Proper drying of the genitals after hygiene procedures. It should be carried out with a clean towel or napkin in the direction from front to back or with gentle blotting movements.
- Careful selection of underwear. It is optimal if it is underwear made of natural and soft material that will not squeeze or rub the perineum.
- General maintenance of immunity, which will allow the body to independently fight infection and suppress the proliferation of pathogens.
Preventive measures
It is easier to prevent any disease than to treat it. To prevent vulvovaginitis, the following measures are recommended:
- proper toilet of the vulva. You need to wash from front to back. Do not use products with an aggressive pH environment;
- wearing tailored underwear made from natural materials;
- use of barrier contraception;
- excluding douching without indications - this way you can wash healthy flora;
- visit a gynecologist for consultation 1-2 times a year.
Inflammation of the labia in women, video
Gynecologist Irina Vladimirovna Garyaeva about vulvitis in women.
Source - KVD - dermatovenerological dispensary Sources:
- ROLE OF INFECTIONS IN THE GENESIS OF VULVA DISEASES. Reutskaya M.A., Kulinich S.I. // Siberian Medical Journal (Irkutsk). – 2010. – No. 6. – pp. 239-242.
- CLINICAL AND MORPHOLOGICAL PRINCIPLES OF TREATMENT OF CHRONIC VULVITIS. Kulinich S.I., Reutskaya M.A., Pokinchereda T.V., Ezhova I.V. // Acta Biomedica Scientifica. – 2013. – No. 5 (93). – P.42-48.
- Diseases of the cervix, vagina and vulva: Clinical lectures. Ed. V.N. Prilepskaya. // M.: MEDpress. - 1999. - P. 432.
- Recurrent vulvovaginal candidiasis: etiology, pathogenesis, treatment. Levonchuk E.A. // Med. news. - 2001. - No. 4. — P. 40-43.
- Dystrophic diseases of the vulva. Diseases of the cervix, vagina and vulva. Ed. V.N. Prilepskaya. // M.: MEDpress. - 1999. - pp. 326-336.
- https://simptom-lechenie.ru/en/vulvit-u-zhenshhin-i-devochek-simptomy-i-lechenie.html
- https://www.thenakedscientists.com/science-articles
- https://woman-centre.com/vlagalische-i-vulva/vulvit/vulvit-u-zhenshhin.html
- https://simptomer.ru/bolezni/zhenskie-zabolevaniya/864-vulvit-simptomy
Popular questions
I suspect inflammation and cysts.
The doctor prescribed IV thiosulfate, IM ceftriaxone, and Diclovit suppositories. I just didn’t explain, is it necessary to apply everything at the same time or what? Hello! Most often, this complex of treatment is carried out simultaneously, but it is better to check with your doctor.
Hello. My labia and clitoris are swollen, there is a burning sensation and a cheesy discharge with something in it, the color is unclear. What could it be and how to treat it? Before that I had inflammation and treatment, and after that it all started. Hello! This is how vulvovaginitis manifests itself. I recommend that you contact an obstetrician-gynecologist and conduct an examination to find out the cause of the inflammation. This will allow you to correctly prescribe therapy. At this stage, you can use Gynocomfort gel with tea tree oil, 1 dose once a day, which will limit the spread of inflammation and improve your well-being.
Hello! Severe itching on the labia, irritation. There is nothing to worry about in the vagina itself. What could it be?
Hello! This may result in an allergic reaction or inflammation. I recommend using Ginocomfort gel with mallow extract, applying it once a day to the discomfort zone for 7 days. If you do not notice relief, consult a doctor.
Good morning, I have vulvitis on my labia minora, I don’t know what to do or how to treat it.
Hello!
If inflammation occurs in the labia minora area, you can use Gynocomfort gel with tea tree oil. The gel is applied in a thin layer once a day for 1 week. If complaints persist, you should consult a specialist. For an accurate diagnosis, contact a specialist
Reviews
Author, 06/24/2016
Hello! The story is like this. Candidiasis, that is, thrush, has been tormenting me for a long time. Flucostat is effective for two days for a maximum of a week. I contacted doctors. The last doctor prescribed a diet and a long course of treatment. Apply clotrimazole externally for 21 days, Viferon suppositories, then a one-time application, five Revita tablets taken internally for a month (so that ascorbic acid restores the microflora). And in the end, two weeks after the end of treatment, the finish is complete again. Everyone stupidly advises using soda the old fashioned way, but I’m afraid of experiments. Who was in such a situation and won this byaku? Please share your experience.
Irina, 08/15/2016
Oh, how familiar this problem is to me, nothing helps. There are probably no medications that I haven’t tried. I took smears and culture tests 100 times. I did everything as prescribed by the doctor. After treatment with antifungal drugs, I took probiotics and put on suppositories. I also tried folk remedies. I donated blood. It seemed like the norm was the last time (albeit a year ago). I’ve been suffering from this infection for about 15 years. At first there were relapses once every six months, then after a month or two, now a week after the end of treatment. I don’t know what to do. I’ll go to the doctor again. But I don’t believe it anymore. All this time I did what they told me. How much money I spent, I’m generally silent. And I tried expensive medications and their analogues. They brought it to me from abroad. I constantly deal with this garbage. I don’t believe that anything will help. More like a cry from the heart. I finished another course of treatment a week ago. Here we go again...
Alena, 35 years old, September 20, 2016
I had thrush for about 9 years. I read medical articles about this, itraconazole helped me, but I took it for about a week at the same time as Terzhinan suppositories for 10 days, after that Vaginorm for 6 days along with ecofemin in tablets, and don’t expect to be cured in one month, further 3 months, fluconazole once a week, and do not stop repeating Vaginorm and Ecofemin after menstruation, and then depending on the situation, as soon as I feel that something is starting again, terzhinan suppositories and Ecofemin lactobacilli, constant monitoring, but for almost a year there have been no fungus in tests)!