Very often, patients come to the appointment who, due to pain in the upper abdomen, heaviness in the epigastric region after eating, and belching, have undergone gastroduodenoscopy and made a conclusion, based on which the doctor has diagnosed “atrophic gastritis.” A person is worried about what to do and whether this gastritis can turn into stomach cancer?
Today we will try to answer the question of what methods will help confirm the presence of atrophic gastritis and how to treat such patients.
Among stomach diseases, the most common diagnosis made by practitioners is “chronic gastritis.”
Chronic gastritis occupies a central place among stomach diseases and is the most common disease of the gastrointestinal tract. It is believed that a third of the adult population suffers from chronic gastritis, but only 10-15% consult a doctor. It is important that chronic gastritis precedes or accompanies diseases of the stomach that are serious in course and prognosis - peptic ulcers, stomach cancer, as well as nearby organs of the digestive system.
Atrophic gastritis - what is it?
What do we mean by atrophic gastritis? It is based on atrophic processes in the gastric mucosa, inflammatory and dystrophic processes that lead to functional failure of the mucosa. Atrophy of the glands of the gastric mucosa consists of a decrease in the number of cells that produce enzymes (pepsins) and parietal cells that secrete hydrochloric acid, and cells that produce Castle factor.
Anatomy of the stomach
Conventionally, there are several sections in the stomach:
- the cardiac section is the most initial one, where food comes from the esophagus,
- fundus - the uppermost dome-shaped part of the stomach, located at the very top of the stomach and where there is always some air,
- the body of the stomach (fundus), where enzymes and hydrochloric acid are produced and food is located during digestion,
- the outlet section or pyloric section of the stomach (antrum), which ends with the pyloric sphincter, which limits the cavity of the stomach and separates it from the duodenum.
Atrophy of stomach cells can affect all sections of the stomach, and then we are talking about total damage to the organ or affect specific sections - fundus (damage to the body of the stomach), antrum (outlet section of the stomach), or selectively affect part of the cells of the stomach. The clinical manifestations of atrophy in different parts of the stomach will be different.
It is known that the stomach is a hollow organ where food enters from the oral cavity and where gastric digestion of food occurs: food deposition, mechanical and chemical processing of food and its evacuation from the stomach into the intestinal tract.
Cytology of the stomach
In the mucosa of each section there are various cells responsible for the digestion of food and participation in hematopoiesis:
- parietal (or parietal) and main cells of the body of the stomach, which produce hydrochloric acid,
- pepsinogens, which under the influence of hydrochloric acid are converted into the active enzyme pepsin, which digests food proteins,
- chymosin and lipase, which digest milk,
- Castle factor (gastromucoprotein), which is responsible for the participation of the stomach in hematopoiesis and vitamin B12 metabolism. Castle factor binds to vitamin B12 in protein foods in the presence of calcium and transports vitamin B12 to the intestines, where it is absorbed into the body. With a lack of production of Castle factor, B12-deficiency anemia develops (decreased blood hemoglobin).
Additional flocculi of the gastric mucosa form mucus in almost all parts of the stomach. This mucus performs a protective function against bile, medications that the patient takes, and hydrochloric acid.
In the outlet section of the stomach there are endocrine cells - G cells, which produce a stimulator for the formation of pepsinogens, hydrochloric acid, and are responsible for the state of the motor function of the stomach.
Definition of the term
The stomach plays a huge role in the digestive process. Under the influence of peristalsis, the food bolus is mixed. It also produces a huge number of enzymes. Thanks to the acidic environment of the stomach, bacterial infection is neutralized. When low-quality food is ingested, the gag reflex is triggered, which prevents further distress.
Ninety-nine percent of digestive juice consists of water. It also contains enzymes and mineral components. A change in color to yellow indicates the presence of bile secretion in the gastric secretion. A red or brown tint may indicate blood. During active fermentation processes, the juice has an unpleasant putrefactive odor.
Important! Hydrochloric acid, which is part of the digestive juice, is the most powerful stimulator of pancreatic secretion.
In between meals, the stomach produces neutral mucus. After eating food, an acidic reaction appears in it. The composition of the secretion may vary depending on the amount of food consumed and its type. Thanks to the presence of mucus, the aggressive effect of the secreted acid is neutralized. This is why human gastric juice does not damage the inner walls of the stomach.
Moreover, viscous mucus envelops the food bolus, thereby improving digestive function. The chemical composition of gastric juice includes the following components:
- hydrochloric acid;
- mucoids;
- pepsin;
- lipase;
- mineral salts.
Experts also note that gastric juice contains bicarbonates. What role do these components perform? Interestingly, acid begins to be produced only after the corresponding reflex is triggered, which does not always appear when food enters.
What happens if the reflex works, but there is no food in the stomach? This is where bicarbonates help. The ions have a protective function and prevent acid from damaging the organ. Under their influence, carbon dioxide and water are formed, as a result of which the acidic environment is replaced by an alkaline one. If not for bicarbonates, reflux of stomach contents could result in burns to the larynx and throat.
Hydrochloric acid in the stomach plays a huge role in digestion.
Atrophic gastritis - causes of development
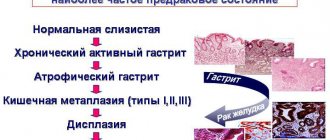
The most common cause of atrophic gastritis at present is considered to be Helicobacter pylori infection. Superficial gastritis develops in the stomach and, with prolonged infection, becomes atrophic.
Stomach infection is associated with damage to the antrum of the stomach in the form of limited or total damage to this department - atrophic gastritis of the antrum and body of the stomach. The development of atrophic processes in the stomach can be the result of age-related changes in the mucosa, genetic characteristics caused by hypo- or atrophy of the gastric mucosa, drug-induced damage to the stomach, or long-term use of antisecretory drugs (PPIs).
Autoimmune atrophic gastritis, when the body begins to produce antibodies against its cells in the gastric mucosa, is quite rare.
Drugs to get rid of reflux
H2 blockers and proton pump inhibitors
Treatments for reflux include H2 blockers (also known as H2 antagonists) and proton pump inhibitors (PPIs). These medications are available in tablet form. For the drug to take effect, it must be completely absorbed. Some types of medications can be obtained without a prescription, while others require a doctor's recommendation, especially if reflux symptoms become too frequent or cause increasing discomfort.
Antacids
Antacids can also be used to treat reflux, but are used for mild symptoms. Antacids contain acid neutralizing agents such as calcium carbonate, magnesium carbonate and aluminum bicarbonate.
alginates, e.g. Gaviscon® Double Action
Gaviscon® Double Action is involved in two processes to prevent reflux:
- Firstly, one of the elements contained in Gaviscon® Double Action is sodium alginate, which is a natural component obtained from brown seaweed. When it comes into contact with the acid of the gastric juice, a protective barrier begins to form between the esophagus and the stomach, preventing the acid of the gastric juice from entering the esophagus, thus the person ceases to experience discomfort and pain. In addition, the alginate gel, entering the esophagus, reduces irritation of the mucous membrane
- Secondly, Gaviscon® Double Action contains antacids - calcium carbonate and sodium bicarbonate - which quickly neutralize excess gastric acid. Thus, thanks to the above properties, a person ceases to feel a feeling of heaviness and discomfort.
"Gaviscon® Double Action" is available without a doctor's prescription. Expectant mothers can also take this drug because it is not absorbed into the blood.
Gaviscon® Double Action has a longer lasting effect1 than antacids.2,3
How to confirm the diagnosis of “atrophic gastritis”
The diagnosis of chronic atrophic gastritis is morphological . If an endoscopic examination is carried out, then if atrophic processes in the stomach are suspected, biopsies of the gastric mucosa should be taken and a histological interpretation of the changes in it given.
The morphological diagnosis should take into account: damage to the stomach, the condition of the glands, the severity and depth of inflammation and changes in the mucosa (metaplasia, dysplasia). The clinical diagnosis of “chronic atrophic gastritis” without morphological confirmation does not make sense.
The most accurate diagnostic method is endoscopic examination with biopsy . However, due to the uneven distribution of atrophic processes in the gastric mucosa, histological studies can give false negative results. In addition, biopsy is an expensive and time-consuming method and cannot be performed on every patient, and endoscopic examination itself is a seriously invasive method of examination.
Currently, there is an alternative to biopsy of the gastric mucosa - a screening method of research called “serum biopsy”, which can objectively reflect the functional state of the gastric mucosa and its morphological basis using blood serum samples.
Serum biopsy or Gastropanel (or test panel ) provides a simple and reliable way to obtain great information about the structure and function of the gastric mucosa, with great sensitivity and specificity to identify patients with atrophic gastritis and those who need further examination - endoscopic examination of the stomach. If the test panel reveals atrophic gastritis, then endoscopic examination is mandatory with oncological alertness.
Let's consider the role of individual components of gastric juice in digestion. The role of hydrochloric acid in digestion in the stomach
.
Hydrochloric acid is secreted by the parietal cells of the main glands of the stomach. It performs the following functions: - carries out acid denaturation of proteins, preceding their hydrolysis and facilitating it, - promotes the swelling of nutrients, promoting subsequent hydrolysis, - activates enzyme precursors and creates an environment of certain acidity for their action, - indirectly (through the activation of gastrin) participates in stimulation of the glands of the fundus of the stomach, - directly and indirectly affects the activity of subsequent parts of the digestive tract, - has a bactericidal and bacteriostatic effect on microbes entering the stomach with food. The role of enzymes in digestion in the stomach
.
The role of salivary enzymes in digestion in the stomach
.
The stomach receives food that has been previously processed in the oral cavity, that is, crushed and mixed with saliva containing the enzymes α-amylase (α - amylase) and maltase. In general, α-amylase hydrolyzes starch and glycogen to produce maltose (~20% of the final hydrolysis product), maltotriose, as well as a mixture of branched oligosaccharides (α-dextrins), straight oligosaccharides and some glucose (together ~80% of the final hydrolysis product). To activate α-amylase, chloride anions are required. The intensity and duration of hydrolysis depends on the alkalinity of the medium. Alkalinity level limits are optimal for maximum action of α-amylase pH
= 6.6 ÷ 6.8.
Salivary maltase acts on the carbohydrate maltose, breaking it down into glucose. Alkalinity level limits are optimal for maximum effect of maltase pH
= 5.8 ÷ 6.2.
When moving from the mouth to the stomach, the food bolus wedges into the thickness of previously consumed food located in the stomach. This may delay for some time the change in the environment of the food bolus from alkaline to acidic, due to the mixing of gastric juice with hydrochloric acid. Under such alkaline conditions, salivary enzymes continue to hydrolyze starch and glycogen. In the stomach cavity, ~30 ÷ 40% of all carbohydrates received with food are digested. Gradually, hydrochloric acid from the surface mixes with the contents of the stomach and its alkaline environment changes to acidic. Salivary amylase and maltase are inactivated. Subsequent breakdown of carbohydrates is carried out by enzymes of pancreatic juice during the passage of chyme into the small intestine. The role of gastric juice enzymes in digestion in the stomach
.
Pepsin
(pepsins) is a product of the main cells of the main glands of the fundus (dome) and body of the stomach.
Pepsin is secreted by these cells, stored and excreted in an inactive form in the form of the proenzyme pepsinogen, which is activated by hydrogen cations, the source of which is hydrochloric acid. Pepsinogen can be activated by pepsin (autocatalysis). During the process of activation of the pepsinogen protein, several peptides are separated from it, one of which plays the role of an inhibitor. Pepsin ensures the disaggregation of proteins, which precedes their hydrolysis and facilitates it. As a catalyst, it has protease and peptidase effects. The greatest catalytic activity of pepsin is observed at low acidity ( pH
= 1.5 ÷ 2.0).
Moreover, one gram of pepsin in two hours can break down ~50 kg
of egg albumin, curdle ~100,000
liters
of milk, and dissolve ~2000
liters
of gelatin.
Gastric juice has two limits of pH
for the manifestation of the greatest proteolytic activity:
pH
= 1.5 ÷ 2.0 and
pH
= 3.2 ÷ 3.5.
The first optimum corresponds to pepsin, and the second to the enzyme gastricsin. Gastricsin
(other names:
pepsin C
, pepsin C;
parapepsin II
, parapepsin II) is a product of the main cells of the main glands of the fundus (dome) and body of the stomach.
Like pepsin, this enzyme is secreted, reserved and excreted by the main cells of the main glands of the fundus (dome) of the stomach, the antrum of the stomach, and the glands of the proximal duodenum. Gastricsin is excreted in an inactive form as a proenzyme (progastricsin) and is activated by hydrochloric acid of gastric juice. Gastrixin hydrolyzes hemoglobin more actively than pepsin and is not inferior to pepsin in the rate of hydrolysis of egg white. Some differences were noted in the peptidase action of pepsin and gastricsin, clear differences in molecular weight, in the shape of the molecule, which indicates the difference between these enzymes. Both pepsin and gastrixin are obtained in pure form. Pepsin and gastrixin provide 95% of the proteolytic activity of gastric juice. The amount of gastricsin in gastric juice is ~20 ÷ 50% of the amount of pepsin. Pepsin-B
(other names
parapepsin
I, parapepsin I;
gelatinase
, gelatinase), like other proteolytic enzymes, is secreted, reserved and excreted by the main cells in an inactive form in the form of a proenzyme (pepsinogen-B) and is activated with the participation of calcium cations.
Pepsin-B differs from pepsin and gastricsin in having a more pronounced gelatinase effect and a less pronounced effect on hemoglobin. It breaks down the protein contained in connective tissue - gelatin. Chymosin
(another name is
rennin
) is a product of the main cells of the main glands of the fundus (dome) and body of the stomach.
This enzyme is also secreted, reserved and excreted by the main cells in an inactive form in the form of a proenzyme and is activated by hydrogen cations of gastric juice in the presence of calcium ions. Rennin curdles milk to a greater extent than pepsin, that is, in the presence of calcium ions, it breaks down the water-soluble caseinogen protein into insoluble casein protein. By this, rennin possibly prevents the rapid release of milk from the stomach. Subsequently, casein is digested by pepsin. Lipase
is an enzyme contained in small quantities in gastric juice and which carries out the initial hydrolysis of fats.
In this case, fats are broken down into glycerol and fatty acids. Like all enzymes, lipase is a surface-active catalyst. The larger the substrate surface, the better the hydrolysis results. Emulsified fats have the largest total surface area. An emulsion is a suspension of tiny particles of fat in water. Large particles of fat break down into small ones when surface tension forces are reduced by the action of surfactants and emulsifiers. Fats that enter the stomach are predominantly non-emulsified (with the exception of milk fats and meat broths). There are no fat emulsifiers in gastric juice. Therefore, there are no conditions in the stomach for maximum lipase action. In emulsified form, milk fats can enter the stomach in significant quantities. Therefore, it is believed that gastric lipase is more important for the digestion of fats in the stomach of milk-fed infants. Their gastric lipase breaks down up to 25% of milk fat. In addition to enzymes that catalyze the hydrolysis of food substances, that is, in addition to digestive enzymes, gastric juice contains enzymes that are not directly involved in the digestion of foods, but are important in digestion in general. These are lysozyme and mucolysin. Lysozyme
(lysozyme, another name for muramidase, discovered in 1921 by A. Fleming, Alexander Fleming, 1881-1955, Scottish bacteriologist, Nobel Prize laureate in 1945 for the discovery of penicillin) is an enzyme that is secreted, reserved and excreted by the cells of the surface epithelium of the mucosa stomach lining.
The enzyme lysozyme is found in many other body fluids (tear fluid, saliva, nasal mucus, etc.). This is a hydrolase that catalyzes the hydrolysis of certain bonds in the polysaccharides of the cytoplasmic membranes of bacterial cells, which leads to their destruction. Thus, lysozyme performs the function of nonspecific antibacterial protection. Mucolysin
(mucolysin; another name for mucolytic enzyme) is an enzyme that catalyzes the hydrolysis of mucopolysaccharides.
As a result, the viscosity of secretions containing mucin decreases. Mucolysin can be used to regulate the amount of mucus on the surface of the gastric mucosa and in the contents of the gastric cavity. Mucolysin has not been isolated in its pure form. The role of mucus in digestion in the stomach
.
Gastric mucus
(mucin) is a viscous aqueous solution of a complex mixture of mucoproteins.
Mucus is produced by mucous cells of the glands of the stomach and mucous membrane. Mucin is released at the apical surface of mucous cells from opening preformed vesicles. In addition, mucin is released when mucous cells are exfoliated. Mucin forms dense layers covering the gastric mucosa. Superficial layers of mucin may separate. Therefore, pieces of “soluble mucus” are found in the gastric contents. Mucin is formed mainly by mucoproteins (glycoproteins). These are complex proteins containing carbohydrates. The carbohydrate content of glycoproteins varies significantly (1 ÷ 85%) and depends on the composition (short, long, branched, unbranched chains). Important components of the chains are amino sugars. It is believed that they perform a certain protective function (protection from proteolysis inside the cell and in the extracellular environment). Functions of gastric mucus
: – protects the gastric mucosa from mechanical damaging effects, – protects the gastric mucosa from chemical damaging effects (part of the mucus does not dissolve in hydrochloric acid), – absorbs digestive enzymes and therefore is an active digestive agent, – protects vitamins from destruction, – stimulates the secretion of gastric glands, – neutralizes hydrochloric acid in the pyloric section of the stomach on the surface of the food mass before it exits into the duodenum.
Neurogenic and humoral mechanisms take part in controlling the secretion of gastric juice. A component of gastric juice that is absolutely necessary for the functioning of the body is the internal factor
(Castle). The name of this substance was coined by the American doctor V.B. in the late 20s of the last century. Castle (William Bosworth Castle, 1897-1990). This substance, which is a glycoprotein, is produced by the parietal cells of the gastric glands. Intrinsic factor allows vitamin B12 (cyanocobalamin) to be absorbed in the small intestine. The absence of intrinsic Castle factor in the body leads to a disease known as pernicious anemia. The juice secreted by the glands of different parts of the stomach has unequal digestive power and acidity. Thus, the juice secreted by the glands of the lesser curvature of the stomach is characterized by a high content of pepsin and high acidity. The glands of this part of the stomach begin to secrete juice first and stop secreting earlier than the glands of other parts of the stomach.
See: Gastroenterology: dictionary, Gastroenterology: Literature. Illustrations,
Literature. Illustrations. References. Illustrations
Click here to access the site's library! Click here and receive access to the reference library!
- King MW Enzyme Kinetics. In: Michael W. King, Ph.D. Medical Biochemistry. Terre Haute Center for Medical Education. Enzyme kinetics. Directed by: Michael W. King. "Medical biochemistry". A carefully designed and well illustrated study guide.
Access to this source = Access to the reference. URL: https://www.tryfonov.ru/tryfonov/serv_r.htm#0 quotation - McPherson RA, Pincus MR Eds. Gastric Fluid = Gastric fluid readings. Norm. Probability limits. APPENDIX 3, Table A5-8. In: Henry's Clinical Diagnosis and Management by Laboratory Methods = Laboratory methods in clinical diagnosis. 21st ed., Saunders, 2006, 1472 p. Illustrated reference book.
.CHM format . Access to this source = Access to the reference. URL: https://www.tryfonov.ru/tryfonov/serv_r.htm#0 quotation - Nomenclature Committee of the International Union of Biochemistry and Molecular Biology. Enzyme Nomenclature. Enzymes and Related Biochemicals. Nomenclature of enzymes. Reference materials.
Access to this source = Access to the reference. URL: https://www.chem.qmul.ac.uk/iubmb/enzyme/quotation - Von Worthington. Worthington Enzyme Manual. Enzymes and Related Biochemicals. Enzymes and other issues of biochemistry. Carefully designed and well illustrated reference materials.
Literature. Access to this source = Access to the reference. URL: https://www.worthington-biochem.com/index/manual.html quotation
| LIBRARY = LIBRARY Human Physiology = Human Physiology, Human Anatomy = Human Anatomy, Human Biochemistry = Human Biochemistry, Human Psychology = Human Psychology, Medicine = Medicine, Mathematics = Mathematics, Chemistry = Chemistry, Physics = Physics, General Scientific Literature = General Science Lexis. Click here to access any source in the site's library! Click here and receive access to the any reference of the library! “I AM LEARNED. . . N E D O U C H A ?” T E S T V A S H E G O I N T E L L E C T A Premise : The effectiveness of the development of any branch of knowledge is determined by the degree of compliance with the methodology of knowledge - the knowable entity. |
Error? Click here and fix it! Search on the site E-mail of the author (author)
How is Gastropanel performed?
Blood sampling to determine markers of atrophic gastritis is carried out in the morning on an empty stomach and 20 minutes after a protein breakfast. Blood is collected into serum tubes, which are centrifuged for analysis.
Blood serum analysis determines markers of chronic atrophic gastritis. Markers of atrophy of the mucous membrane of the fundic and antral parts of the stomach are:
- Pepsinogen I, Pepsinogen II and their ratio,
- Gastrin-17 and Gastrin-17 stimulated after a protein breakfast,
- determination of antibodies to Helicobacter pylori Ig G.
The tests are based on enzyme immunoassay technology.
Besides,
- Antibodies to parietal cells of the body of the stomach are determined in autoimmune atrophic gastritis with a high risk of disorders associated with vitamin B12 deficiency, for which the level of vitamin B12 is determined.
- Homocysteine is identified as a risk factor for vascular and thromboembolic diseases.
- To clarify Helicobacter pylori infection, an additional test of the acute phase of infection is performed, Ig A and IgM antibodies are determined.
A few words about serum markers
We have a diagnostic algorithm for identifying stomach diseases, which is recommended for all patients who have pain or discomfort in the upper abdomen.
Pepsinogens
There are seven isoforms of pepsin precursors, five of which are designated as group Pepsinogen I of the main cells of the stomach body and Pepsinogen II, uniformly secreted by the glands of the entire stomach and duodenum. Pepsinogens formed in the stomach are absorbed into the blood and determination of their serum level is a generally accepted marker of atrophic gastritis “serological biopsy”.
A decrease in the level of Pepsinogen I indicates the severity of atrophic gastritis of the body of the stomach, and since the activation of Pepsinogen I into active pepsin occurs with the participation of hydrochloric acid, then the level of Pepsinogen I can roughly represent the level of stomach acidity. Pepsinogen II is produced in all parts of the stomach and in the duodenum. As the severity of atrophy increases, the ratio of serum levels of Pepsinogen I and Pepsinogen II decreases, which indicates the severity of atrophy and the spread of the process.
Gastrin
Gastrin-17, produced in the outlet section of the stomach after stimulation of cells by various factors (stomach distension, protein foods). In case of atrophy of the gastric antral mucosa, the secretion of Gastrin-17 decreases. To assess the presence and severity of the atrophic process in the stomach, it is necessary to conduct a protein stimulation test, the decrease of which shows the severity of atrophy; in the case of atrophy of the mucous membrane of the antrum of the stomach, the secretion of Gastrin-17 is proportionally reduced. In patients with severe atrophic gastritis in the antrum of the stomach, the risk of developing stomach cancer is 90 times higher than in people with normal gastric mucosa.
Homocysteine
Homocysteine is an early marker of cellular functional deficiency of B12, B6, folic acid due to the development of atrophic gastritis and other reasons - age, smoking, Helicobacter pylori infection, etc. With atrophic gastritis, the level of homocysteine increases in the blood and becomes toxic to the body. When donating blood for homocysteine, you should avoid protein foods, vitamins, and hormonal contraceptives 1 day before the test. This test can be an addition to the Gastropanel or an independent test for other diseases.
Preventing Reflux
There are two main ways you can help prevent reflux symptoms:
Review your daily habits
- Try to quit smoking or at least reduce the number of cigarettes you consume. The chemical composition of tobacco contains elements that help relax the sphincter muscles. This, in turn, can cause free flow of gastric juice into the esophagus.
- Stop being a hostage to stressful situations. Although there is no conclusive evidence that stress plays a role in reflux symptoms, it is known that stress can be a potential trigger. Therefore, by understanding what makes you worry and trying to stop such situations as much as possible, you can improve your health.
- Try not to wear clothes that are too tight. Avoid compression belts as they will only increase pressure on your stomach and abdomen, which can cause reflux.
- Watch your weight - even a little excess weight can put additional stress on your stomach and cause reflux.
Watch your diet
Certain foods are known to cause reflux, so try to avoid these foods. If you're unsure about foods that trigger reflux in your particular case, try keeping a food diary. Typically, these products include:
- Spicy foods, such as curry dishes
Spicy vegetables: onions, garlic, tomatoes, peppers
- Citrus fruit
- Fatty food
Reflux can also be a result of overeating. If your stomach is full, the pressure on the sphincter will be too much, causing it to relax and allow the contents of the stomach to flow into the esophagus. Having several small meals throughout the day can help reduce your risk of reflux.
Advantages of Gastropanel for diagnosing “atrophic gastritis”
Thus, Gastropanel allows you to answer the following questions:
- does the patient have atrophic gastritis, in which part of the stomach are the changes localized,
- assess the risk of developing stomach cancer and peptic ulcers,
- does the patient suffer from gastritis caused by Helicobacter pylori,
- identify autoimmune gastritis or atrophic gastritis with damage to the body of the stomach, which may determine the risk of developing vitamin B12 deficiency, which can be associated with many diseases (atherosclerosis, vascular damage to the brain and heart, depression, polyneuropathy, dementia, etc.)
What advantages of Gastropanel can be noted: it is a simple non-invasive serological test, high sensitivity, specificity, safety and convenience for the patient, quick results, and meets the principles of evidence-based medicine.
What to do if you are diagnosed with atrophic gastritis
A few words about the principles of treatment of chronic atrophic gastritis. Treatment approaches are individual, it all depends on the severity of atrophic processes, the presence of Helicobacter, and vitamin B12 deficiency.
The problem will be dealt with by a doctor who will prescribe:
- treatment,
- repeated studies to monitor treatment,
- repeated consultations to assess the clinical manifestations of the disease and adjust treatment.
It is most difficult to eliminate autoimmune mechanisms of damage to the gastric mucosa; the question of prescribing hormonal drugs arises only when gastritis is accompanied by anemia. Helicobacter pylori eradication therapy has its own characteristics. First of all, the question arises about the acidity of gastric juice, and more often treatment is carried out without antisecretory drugs. The study of the acidity of gastric juice using the pH-metric method is now rarely carried out (usually daily monitoring in a hospital setting), but it is possible to orient the acidity according to the level of Pepsinogen I.
A high level of Pepsinogen and periodic heartburn in a patient may indicate preserved gastric secretion. In case of atrophic gastritis in a hypo or anacid state with damage to the body and outlet of the stomach, antisecretory drugs are excluded and Helicobacter pylori eradication is carried out with antibiotics. Effective eradication of infection improves processes in the gastric mucosa, and can be considered as a prevention of the development of gastric cancer.
Nutrition for chronic atrophic gastritis
There are no strict dietary restrictions, but you need to know that some foods alkalize the stomach (mainly protein foods) and further reduce the acidity of gastric juice, and there are foods that stimulate it (vegetable and fruit juices, vegetables, fruits).
Most often, doctors prescribe diet 2, the purpose of which is to mechanically spare the gastric mucosa and preserve chemical irritants.
But medical experience shows that strict restrictions are not required. The necessary diet - eating in small portions with replacement therapy drugs allows for good gastric digestion, in which protein foods are also digested in the stomach.
Natural gastric juice
The composition of the drug includes digestive juice, as well as an alcohol solution of salicylic acid. The drug is used to normalize the level of acidity in the stomach and improve digestion processes. Natural gastric juice improves appetite and eliminates dyspeptic disorders. Experts prescribe the remedy for achylia, hypoacid and anacid gastritis.
Natural gastric has some limitations; it cannot be used in the following cases:
- gastroesophageal reflux;
- hyperacid gastritis;
- stomach and duodenal ulcers;
- erosive gastritis and duodenitis;
- allergy to active ingredients.
Proper storage of the drug plays an important role. If you leave the product in a warm place, it will lose its activity.
Atrophic gastritis - treatment
Replacement therapy
Replacement therapy includes the use of hydrochloric acid preparations and gastric juice enzymes:
- Natural gastric juice is a preparation of animal origin, the composition corresponding to human gastric juice, contains hydrochloric acid and enzymes. Use 1-2 tablespoons (15 - 30 ml) during meals or after meals 2-3 times a day.
- Acidin-pepsin , containing betaine hydrochloride, which is hydrolyzed in the stomach to release free hydrochloric acid and the enzyme pepsin. Before use, tablets (500 mg) are dissolved in 50-100 ml of water and taken with meals. These medications are administered through a straw.
- Abomin - the drug contains the sum of proteolytic enzymes of the stomach and is obtained from the gastric mucosa of calves and lambs. Use 1 tablet (0.2 g each containing 50,000 units in 1 tablet) 2 - 3 times a day with meals for 1 - 3 months.
Stimulant therapy
Some drugs that stimulate the secretion of gastric juice:
- Mineral water (Essentuki N17, Narzan) is used warm 15-20 minutes before meals, the course is 2-3 weeks, twice a year.
- Rosehip decoction , cabbage, tomato, carrot, lemon juice, 50 ml each, diluted with boiled water 1:1 before meals, alternate.
- Medicinal mixtures: plantain, St. John's wort, wormwood, thyme in equal proportions.
- Plantaglucide is widely used - granules of plantain leaves to prepare a suspension, for which take 1/1 -1 teaspoon (½-1 g) per ¼ glass of warm water and apply 30 minutes before meals 2-3 times a day, course of treatment 3- 4 weeks, for preventive treatment 1-2 months. Plantaglucide activates gastric secretion, has an enveloping, regenerative, anti-inflammatory and antispasmodic effect.
- Collection of herbalist Mikhalchenko S.I.:
Ingredients: angelica, yarrow, dandelion, birch, trifoliate, plantain, caraway, burnet, licorice, fumifera, calendula, chamomile. Application: pour 1 dessert spoon of the mixture into 500 ml of boiling water, leave in a thermos by volume overnight, strain. Take 150 ml 3 times a day an hour before meals. Before use, warm up by diluting with hot water. Keep refrigerated. Reception: 10 days admission - 2 days break, 3-4 months.
During the period of relative remission of atrophic gastritis, the main drugs are replacement and stimulating therapy, which affect the secretory insufficiency of the stomach.
Foods that affect acidity
To normalize the condition associated with changes in the secretion of gastric juice, it is first necessary to normalize nutrition. Next, let's talk about foods that increase and, conversely, decrease acidity levels.
Raising pH
Alcoholic drinks provoke an increase in acidity. Alcohol irritates the mucous membranes of the digestive organs, which is why nutrients cannot be properly absorbed. The more often a person drinks alcohol, the more intense the digestive juice will be released. This can manifest itself in the form of severe heartburn, nausea and attacks of pain in the stomach area.
Important! The pH level increases after drinking champagne, beer, wine and low-alcohol cocktails.
The basis of the diet for people on a healthy diet is fruit. Many people do not even suspect that they can significantly increase the level of acidity in the stomach. This reaction can be caused by:
- grape;
- melon;
- pomegranate;
- peach;
- kiwi;
- citrus.
Citrus fruits raise pH levels
Oddly enough, some vegetables can also increase the secretion of gastric juice. The functionality of the secret glands increases the consumption of such products:
Hungry stomach pain
- cabbage;
- pickles;
- zucchini;
- tomatoes.
Increased acidity can also be a reaction to fatty and sweet foods. If we talk about fatty foods, they often include spread, margarine, and vegetable fat. Eating such food leads to disruption of digestive processes and an increase in the functional activity of the secret glands.
If we talk about sweets, it is worth noting that not all of them affect the amount of gastric juice produced. Honey, halva and marshmallows do not give such a reaction. Chocolate, cakes, pastries, alcoholic desserts, etc. can increase acidity. Spices give dishes an exquisite taste, but some of them can cause pathological changes in the functioning of the secret glands.
The following foods can enhance the secretion of digestive juice: nutmeg, chili, cloves, ground red and black pepper. Herbs are also used in treatment to neutralize acid. Decoctions of chamomile flowers, licorice root, calamus rhizome, wormwood, and fireweed will help normalize the level of gastric juice.
Lower pH
To reduce acidity, patients are recommended to eat food with a homogenized consistency, namely boiled porridge, pureed soup, pureed vegetable puree from carrots, pumpkin, potatoes. Products containing simple compounds reduce acidity and at the same time do not require a large amount of energy to break down. For example, if you choose between meat and fish, then preference is given to the latter product, since it contains fewer fatty compounds.
Boiled porridge reduces stomach acidity
Let's highlight a list of foods that should be consumed to lower pH:
- cereals: rice, semolina, corn, pearl barley, barley, buckwheat, oatmeal;
- peaches, apples, bananas;
- potatoes, beets, olives;
- raspberries, lingonberries, dogwoods, quinces, currants, tangerines, blueberries, strawberries, wild strawberries.