Pharmacodynamics and pharmacokinetics
This drug is able to reduce hyperglycemia without causing hypoglycemia . insulin secretion is not stimulated , and the hypoglycemic effect does not appear in healthy people.
An increase in the sensitivity of peripheral receptors to insulin and glucose utilization by cells was noted. The production of glucose by the liver is reduced by inhibiting glycogenolysis and gluconeogenesis. The drug inhibits the absorption of glucose in the gastrointestinal tract.
Metformin is characterized by stimulation of glycogen synthesis and an effect on glycogen synthetase. The transport capacity of various types of membrane glucose transporters increases. The medicine also has a beneficial effect on lipid metabolism: reducing the content of total cholesterol , TG and LDL. While using metformin, patients maintain a stable weight or moderately decrease.
As a result of oral administration, complete absorption of the active substance from the gastrointestinal tract is observed. Eating food can reduce and delay this process. At the same time, the absolute bioavailability of metformin is 50-60%. The maximum concentration of the component in the plasma is detected after 2.5 hours.
In the body, metformin is rapidly distributed in tissues, practically without binding to plasma proteins. The drug undergoes little metabolism. Excretion occurs through the kidneys.
Glucophage – present and future in pharmacotherapy of metabolic syndrome
For modern society, metabolic syndrome (MS) represents a serious global problem. According to the latest concepts, MS is a cluster of hormonal and metabolic disorders, interrelated risk factors for the development of cardiovascular diseases and diabetes mellitus, united by a common pathophysiological mechanism - insulin resistance.
Table 1. Direct and indirect cardioprotective effects of metformin
Particular attention paid to this syndrome is due to its high prevalence in the general population, reaching 14-24%, and the number of people at risk for IR syndrome is continuously growing (1, 3, 14). Moreover, in the age groups from 20 to 49 years, MS is more often observed in men. At the age of 50-69 years, the prevalence of MS is almost the same in men and women. On the other hand, MetS plays a significant role in accelerating the development and progression of cardiovascular diseases (CVD) associated with atherosclerosis, and also increases the risk of coronary complications and mortality (10, 15). It is known that the risk of developing coronary heart disease, cerebral stroke, general and coronary mortality increases as the number of components of the metabolic syndrome increases. The association between IR and cardiovascular risk begins in early childhood and persists throughout adolescence (1, 3). In addition, many modern researchers consider it as a prelude to type 2 diabetes mellitus (23). Thus, the risk of developing type 2 diabetes in people with MS is 5-9 times higher than in those without it. Along with this, various population studies have proven the unfavorable effect of MetS on the overall prognosis of life (3, 4, 13).
Currently, the exact causes of insulin resistance (IR) are unknown, in the development of which a complex interaction of hereditary and environmental factors plays an important role. IR is a decrease in the biological effects of insulin in peripheral tissues and organs. In this case, there is a need to increase the amount of insulin to compensate for the insulin-resistant state. Developing compensatory hyperinsulinemia increases the uptake of glucose by peripheral tissues and also reduces hepatic glucose production by the liver, which maintains normal glucose homeostasis for a certain time. Subsequently, the increased content of insulin in the circulation causes the development of a number of hormonal-metabolic, hemodynamic and systemic disorders.
IR can be either genetically determined or acquired. Currently, more than 40 different conditions and diseases are known in which IR develops. The reasons for its development may be stress, physical inactivity, alcohol abuse, trauma, and increased levels of counter-insular hormones. IR is usually detected in individuals with a family history of diabetes who lead a sedentary lifestyle. Along with this, physiological IR is characteristic of puberty, pregnancy and old age. In addition, IR is closely associated with the distribution of adipose tissue in the body. It is visceral adipose tissue, and not subcutaneous fat depots, that plays an important role in the development and progression of IR and associated metabolic disorders (3, 24).
According to criteria developed by the National Cholesterol Education Program Expert Committee (ATPIII, 2001), a diagnosis of MetS is made if a patient has three or more of the following features (20):
- abdominal obesity (waist circumference (WC) >102 cm in men, WC >88 in women);
- triglyceride level ≥ 1.7 mmol/L (≥ 150 mg/dL);
- HDL cholesterol
- arterial hypertension (BP ≥130/85 mm Hg);
- fasting glucose values ≥6.1 mmol/L (≥110 mg/dL).
A new edition of the definition of MetS was presented in 2005 at the 1st International Congress on Prediabetes and Metabolic Syndrome, as well as at the 75th Congress of the European Society of Atherosclerosis (21). A fundamentally new position was the approval of abdominal obesity as the main criterion for diagnosing MS with changes in the following parameters: waist circumference (5.6 mmol/l).
It is no coincidence that abdominal obesity is given an independent place in the proposed definitions of MS. There is a lot of clinical evidence demonstrating a close relationship between abdominal-visceral obesity and a complex of hormonal and metabolic risk factors that form the basis of the syndrome in question. However, it should be noted that a person can have MS even with slight excess body weight (or in its absence) if three other components of the syndrome are detected. The proposed diagnostic criteria are quite simple and convenient for use in clinical practice and are primarily aimed at the early identification of patients at high risk of developing atherosclerotic CVD and type 2 diabetes.
For some time, it was believed that MS was the lot of people predominantly of middle and old age. However, a number of studies indicate that over the past two decades, MetS has shown a steady increase among adolescents and young adults (1, 3, 14). Thus, in the period from 1994 to 2000, the incidence of MS among adolescents increased from 4.2 to 6.4%. In developed countries, about 15% of adolescents are obese and 25% are overweight. It should be noted that in such countries, type 2 diabetes in childhood and adolescence accounts for 10% or more of cases of all forms of diabetes.
Modern approaches to the treatment of MS involve the use of non-pharmacological methods of therapy, which, if necessary, are supplemented with pharmacotherapy. The main goal of therapy for patients with MS is to minimize the risk of developing cardiovascular diseases and their complications (4, 24). Recommendations for lifestyle modification should include individual diet calculations, changing eating patterns and giving up bad habits. Non-pharmacological methods include a low-calorie diet aimed at reducing body weight and optimizing it in combination with systematic physical training or household activities. Patients may be recommended regular dynamic physical activity (dosed walking, swimming, exercise bike) of moderate intensity (4-5 sessions per week for 30-45 minutes), since at the beginning of therapy, patients with MS are often unable to perform long and intense exercise.
Weight loss can be achieved by following a low-calorie diet containing no more than 25-30% fat from the daily calorie intake, including saturated fats - less than 7%, polyunsaturated fats - up to 10% and monounsaturated fats - less than 20%, cholesterol - less than 300- 200 mg, fiber content should be 20-25 g/day. It is also recommended to consume salt in moderation (up to 5 g per day).
According to modern recommendations, the initial weight loss in patients with MS should be at least 10% of the initial weight (4, 24). Losing body weight can reduce IR, as well as obtain a positive effect on blood pressure and blood lipid levels. A decrease in body weight in the range of 5.0-9.9 kg by 15%, and a decrease of 10.0 kg or more by 26% reduces the risk of developing arterial hypertension (7). In addition, for every 1 kg of body weight loss, the concentration of total cholesterol decreases by 0.05 mmol/l, high-density lipoprotein cholesterol (LDL-C) by 0.02 mmol/l, triglycerides by 0.015 mmol/l, and cholesterol levels high density lipoprotein (HDL cholesterol) increases by 0.009 mol/l. In addition, a decrease in body weight by 5.6 kg reduces by 58% the risk of further progression of carbohydrate metabolism disorders - the development of type 2 diabetes mellitus in patients with IGT.
Unfortunately, as practice shows, more than 90% of people who have lost weight gain weight again within one year (3, 23). And only about 4-5% of MS patients can achieve positive results without additional pharmacotherapy. The rapid increase in the prevalence of MS in various age groups, accompanied by an increased cardio-metabolic risk, necessitates the search for effective methods of pharmacotherapy. In this regard, the effectiveness of pharmacotherapy for MS should first of all be assessed from the perspective of preventing the development of diseases associated with atherosclerosis and their complications. Correction of IR, a key pathophysiological component of MS, is an important area of pharmacotherapy. Currently, one of the drugs of first choice for pharmacotherapy of MS is metformin (Glucophage), which not only directly affects IR, but also has a number of beneficial metabolic and cardiovascular effects.
The results of experimental and clinical studies have made it possible to reveal new aspects of the action of metformin, to better evaluate its practical significance, and to expand the indications for its use (3, 7, 23). Currently, metformin is effectively used not only for diabetes, but also in patients with MS, polycystic ovary syndrome (PCOS), and hepatosteatosis.
Glucophage, a drug belonging to the biguanide group, increases hepatic and peripheral sensitivity to endogenous insulin, and, most importantly, does not affect insulin secretion by β-cells. By reducing glucotoxicity and lipotoxicity, Glucophage indirectly improves insulin secretion. The primary antihyperglycemic effect of the drug is due to a decrease in the production of glucose by the liver (gluconeogenesis), as well as the secretion of free fatty acids, fat oxidation and, in part, an increase in peripheral glucose uptake (3, 15). Metformin has the ability to reduce FFA oxidation by 10-30%. By reducing the concentration of FFA (by 10-17%), it not only improves insulin sensitivity, but also helps correct impaired insulin secretion. In general, normalization of FFA concentrations leads to the elimination of lipotoxicity effects at all levels, including the liver, adipose and muscle tissue, and the islets of Langerhans. Treatment with metformin is associated with positive changes in the lipid spectrum: a decrease in the concentration of triglycerides by 10-20%, LDL cholesterol by 10% and an increase in the concentration of HDL cholesterol by 10-20%.
Increased sensitivity of peripheral tissues to the action of insulin under the influence of Glucophage is realized through several cellular mechanisms. Thus, on the part of insulin receptors, an increase in quantity and affinity is observed. In addition, there is stimulation of the tyrosine kinase activity of the receptor, the expression and activity of glucose transporters, as well as active translocation of transporters from the intracellular pool to the cell membrane (14).
Glucophage has an active effect on the adsorption of dietary carbohydrates in the gastrointestinal tract, slowing down its rate, and also reduces appetite. The intestinal effects of the drug make a significant contribution to the prevention of postprandial hyperglycemic peaks associated with the risk of premature mortality from CVD (3, 9). Another significant effect of Glucophage is the reduction or stabilization of the patient’s body weight, as well as a decrease in the deposition of visceral fat. It is believed that one of the mechanisms of the anorexigenic effect of metformin is associated with the effect of the drug on the metabolism of glucagon-like peptide-1 (GLP-1). Thus, in the work of Mannucci E. at al, the levels of GLP-1 (7-36)amide/(7-37) were determined initially and after 15 days of metformin therapy (2550 mg/day) in obese patients before and after GTT load ( 18). In order to eliminate the influence of insulinemia and glycemia on GLP-1 secretion, the study was conducted under conditions of an euglycemic hyperinsulinemic clamp. The authors found no changes in GLP-1 concentrations in the control group. At the same time, in obese patients, metformin caused a significant increase in the concentration of GLP-1 (7-36)amide/(7-37) at 30 and 60 minutes of the test with unchanged basal peptide levels. In mixed plasma (after 30 minutes of incubation at 37oC), as well as in a buffer solution containing dipeptidyl peptidase-4, metformin inhibited the degradation of GLP-1.
An important effect of metformin is the reduction or stabilization of body weight, as well as a decrease in the deposition of visceral fat. Various clinical studies have found that, depending on the duration of drug use, the reduction in body weight in patients with MS ranged from 0.5 to 4.5 kg (2, 3, 8). One of the mechanisms of the anorexigenic action of Glucophage appears to be due to its action at the level of the central nervous system. Thus, recently, in an experiment on animal models, it was shown that by inhibiting the activity of AMP kinase in hypothalamic neurons, the drug modulates the expression of orexigenic neuropeptide Y (6).
In recent years, a lot of interesting data have appeared on the hemodynamic effects of Glucophage, which indicate the significant role of the drug in the prevention and slowdown of the progression of cardiovascular diseases in patients with MS, type 2 diabetes (Table 1). Thus, the drug has a positive effect on the hemostatic system and blood rheology, has the ability not only to inhibit platelet aggregation, but also reduces the risk of blood clots (5, 11, 17). Metformin has been shown to reduce the levels of platelet factor 4 and β-thromboglobulin, which are known markers of platelet activation. Recent studies have shown an improvement in fibrinolysis under the influence of Glucophage therapy, which is due to a decrease in the level of PAI-1, which inactivates tissue plasminogen activator (2). In addition, the drug also has an indirect mechanism for reducing PAI-1 levels. Visceral adipose tissue adipocytes produce significantly more PAI-1 than subcutaneous adipose tissue adipocytes, and metformin therapy helps reduce visceral fat mass.
It should be noted that Glucophage has an anti-atherosclerotic effect, acting at the early stages of the development of atherosclerosis and disrupting the adhesion of monocytes to the vascular endothelium, lipoidosis, and the ability to take up lipids (17). In addition, the drug suppresses the processes of differentiation of monocytes into macrophages, which actively secrete proatherogenic factors. Recently, metformin has been shown in vitro to have an inhibitory effect on leukocyte-endothelial interactions as well as on the endothelial surface expression of adhesion molecules such as intracellular adhesion molecule 1, vascular cell adhesion molecule 1, and E-selectin (11, 15). A number of experimental studies indicate the active intervention of metformin in the metabolism of lipids in the vascular wall. Thus, the drug accelerates the catabolism of LDL, promoting their conversion to HDL, reduces the accumulation of cholesterol esters in the aorta, increases the content of phospholipids and reduces sphygnomyelin. In vivo and in vitro studies have shown that metformin attenuates atherosclerotic plaque formation in rabbits and rats fed a high-fat diet. Along with this, metformin reduces the proliferation of vascular smooth muscle cells (SMCs).
Consequently, by reducing the deposition of lipids in the vascular wall, reducing the proliferation of SMCs, disrupting adhesion, transformation of monocytes and the ability to take up lipids, metformin actively affects the early stages of the development of the atherosclerotic process.
The positive vascular effects of metformin include normalizing the contraction/relaxation cycle of arterioles, reducing the permeability of the vascular wall and inhibiting the processes of neoangiogenesis (3, 15). One of the first stages of the atherosclerotic process is endothelial dysfunction, which significantly worsens the prognosis and aggravates the course of MS and diabetes. It has been shown that during 12-week therapy with metformin in patients with type 2 diabetes with the introduction of acetylcholine, according to plethysmography, a significant increase in blood flow in the peripheral arteries was noted (19). In patients with MS treated with metformin (1000 mg/day, 12 weeks), along with a decrease in body weight and IR (by 26%), an improvement in endothelium-dependent vasodilation (EDVD) was observed (22). Thus, in the group of patients with MS, the average EDV value initially and after treatment with metformin was 7.4 ± 2.1% and 12.4 ± 1.9%, respectively, compared with the EDV values of the placebo group – 7.3 ± 2.5% and 6.9 ± 2.7%.
In a double-blind randomized study, the effect of metformin on vascular reactivity was studied in first-degree relatives of patients with type 2 diabetes with MS without impaired glucose tolerance (mean age 38.3 ± 7.6 years, BMI 36.3 5 ± 2 kg/m2 ) (8). It was noted that in conditions of reactive hyperemia, metformin therapy led to a significant improvement in endothelium-dependent vasodilation (infusion of acetylcholine 7.5, 15 and 30 mcg/min), without affecting endothelium-independent vasodilation (infusion of nitroprusside - sodium 2, 4 and 8 mcg/min.).
In recent years, special attention has been paid to the prevention of type 2 diabetes (1, 4, 23). According to Laaksonen DF at al. The risk of developing type 2 diabetes in patients with MS increases 7-9 times compared to individuals without MS (16). There are currently over 300 million people worldwide with impaired glucose tolerance (IGT) (23). According to epidemiological forecasts, by 2025 the number of patients with IGT will reach 500 million. It is known that annually approximately 1.5-7.3% of people with IGT develop type 2 diabetes.
The largest DPP trial (Diabetes Prevention Program, 2002) clearly showed that Glucophage therapy can effectively and safely prevent the development of type 2 diabetes in patients with IGT, especially in patients with a BMI of more than 25 kg/m2 (9). Thus, in patients with IGT and overweight who received Glucophage (1700 mg/day), there was a 31% reduction in the risk of developing type 2 diabetes compared to the group of patients who did not receive drug therapy.
Due to the absence of long hydrophobic side chains, both the ability of the drug to bind to the cell membrane and, indeed, active accumulation inside the cell are limited, which determines the low likelihood of developing lactic acidosis, as well as the high safety of metformin (3, 15). The drug is practically not metabolized in the body and is completely excreted unchanged by the kidneys (half-life 1.5-4.9 hours). With renal failure, a decrease in the excretory function of the kidneys, especially with age, the rate of metformin excretion decreases in proportion to the decrease in creatinine clearance and the risk of lactic acidosis increases. Treatment with the drug is initiated with 500-850 mg taken with dinner or at night. To avoid side effects of metformin (diarrhea, flatulence, abdominal discomfort, metallic taste in the mouth), gradual titration of the drug dose is necessary. Thus, the daily dose of the drug is gradually increased by 500-850 mg every 1-2 weeks, and in some cases there was a temporary reduction in the dose to the previous one. Side effects usually disappear when the dose of the drug is reduced. The maximum therapeutic dose in patients with MS is 1500-3000 mg/day in 2-3 doses. Contraindications to the use of metformin are impaired renal function (a decrease in creatinine clearance below 50 ml/min or an increase in creatinine in the blood above 1.5 mmol/l), alcohol abuse, pregnancy, lactation, as well as hypoxic conditions of any nature.
In conclusion, the use of metformin in combination with non-pharmacological methods is an effective and safe method in the management of metabolic syndrome, not only improving insulin sensitivity, but also having a positive effect on numerous risk factors for cardiovascular diseases. When choosing a drug for pharmacotherapy of patients with MS, you should always remember the proven benefits of metformin in this category of patients.
Contraindications for use
It is not recommended to take Glucophage if:
- diabetic ketoacidosis , precoma and coma ;
- impaired renal and liver function;
- various acute diseases;
- injuries and surgical operations;
- chronic alcoholism , severe alcohol poisoning;
- lactation, pregnancy;
- lactic acidosis;
- the period 2 days before and after radioisotope or x-ray studies involving the administration of iodine-containing contrast agent;
- following a hypocaloric diet ;
- sensitivity or intolerance to the drug.
You should also refrain from using the medicine in patients over the age of 60 years and those engaged in heavy physical work with a high risk of developing lactic acidosis .
Glucophage long
Use during pregnancy and breastfeeding
Decompensated diabetes mellitus during pregnancy is associated with an increased risk of birth defects and perinatal mortality.
Limited evidence suggests that the use of metformin in pregnant women does not increase the risk of birth defects in children.
When planning pregnancy, as well as in case of pregnancy while using metformin, the drug should be discontinued and insulin therapy should be prescribed. It is necessary to maintain blood glucose concentrations at a level as close to normal as possible to reduce the risk of fetal malformations.
Metformin is excreted in breast milk. No side effects were observed in breastfeeding newborns while taking metformin. However, due to limited data, the use of the drug during breastfeeding is not recommended. The decision to stop breastfeeding should be made taking into account the benefits of breastfeeding and the potential risk of side effects in the baby.
Use for liver dysfunction
Contraindication: liver failure, impaired liver function.
Use for renal impairment
Contraindicated in case of renal failure or impaired renal function (creatinine clearance less than 60 ml/min), in acute conditions with a risk of developing renal dysfunction, incl. dehydration (with chronic or severe diarrhea, repeated bouts of vomiting), severe infectious diseases (for example, respiratory and urinary tract infections), shock.
Use in children
Contraindicated in children and adolescents under 18 years of age due to the lack of data on use.
Use in elderly patients
The drug should be used with caution in patients over 60 years of age who perform heavy physical work, which is associated with an increased risk of developing lactic acidosis.
special instructions
Lactic acidosis
Lactic acidosis is an extremely rare but serious (high mortality rate unless promptly treated) complication that can occur due to accumulation of metformin. Cases of lactic acidosis in patients receiving metformin occurred mainly in diabetic patients with severe renal failure.
Other associated risk factors should be considered, such as poorly controlled diabetes, ketosis, prolonged fasting, excessive alcohol consumption, liver failure and any condition associated with severe hypoxia. This may help reduce the incidence of lactic acidosis.
The risk of developing lactic acidosis should be taken into account when nonspecific signs appear, such as muscle cramps accompanied by dyspepsia, abdominal pain, general weakness and severe malaise.
Lactic acidosis is characterized by acidotic shortness of breath, vomiting, abdominal pain, muscle cramps and hypothermia followed by coma. Diagnostic laboratory parameters are a decrease in blood pH (<7.25), plasma lactate content >5 mmol/l, increased anion gap and lactate/pyruvate ratio. If lactic acidosis is suspected, stop taking the drug and consult a doctor immediately.
Surgical operations
The use of metformin should be discontinued 48 hours before elective surgery and can be continued no earlier than 48 hours after, provided that renal function has been found to be normal during the examination.
Kidney function
Since metformin is excreted by the kidneys, before starting treatment, and regularly thereafter, it is necessary to determine CC: at least once a year in patients with normal renal function, and 2-4 times a year in elderly patients, as well as in patients with CC on lower limit of normal. In the case of CC less than 45 ml/min, the use of the drug is contraindicated.
Particular caution should be exercised in case of possible impairment of renal function in elderly patients, with simultaneous use of antihypertensive drugs, diuretics or NSAIDs.
Heart failure
Patients with heart failure have a higher risk of developing hypoxia and renal failure. Patients with chronic heart failure should have cardiac and renal function monitored regularly while taking metformin.
Taking metformin in acute heart failure and chronic heart failure with unstable hemodynamic parameters is contraindicated.
Other Precautions
Patients are advised to continue to follow a diet with even carbohydrate intake throughout the day.
Overweight patients are recommended to continue to follow a hypocaloric diet (but not less than 1000 kcal/day). Patients should also exercise regularly.
Patients should tell their doctor about any treatment they are undergoing and any infectious diseases such as respiratory or urinary tract infections.
Standard laboratory tests should be performed regularly to monitor diabetes mellitus.
Metformin does not cause hypoglycemia when used alone, but caution is recommended when used in combination with insulin or other oral hypoglycemic agents (for example, sulfonylureas or repaglinide). Symptoms of hypoglycemia include weakness, headache, dizziness, increased sweating, rapid heartbeat, blurred vision, or difficulty concentrating.
It is necessary to warn the patient that the inactive components of the drug Glucophage® Long can be excreted unchanged through the intestines, which does not affect the therapeutic activity of the drug.
Impact on the ability to drive vehicles and operate machinery
Monotherapy with Glucophage Long does not cause hypoglycemia and therefore does not affect the ability to drive a car or operate machinery.
However, patients should be warned about the risk of hypoglycemia when using metformin in combination with other hypoglycemic drugs (sulfonylureas, insulin, repaglinide).
Side effects
When treated with this drug, side effects may develop in the form of disturbances in the digestive system, for example: nausea, vomiting, metallic taste, loss of appetite, diarrhea, flatulence , and so on. Typically, these symptoms occur at the beginning of therapy and subsequently disappear on their own.
Metabolic abnormalities in the form of lactic acidosis , which requires discontinuation of treatment, are also possible. Long-term use of Glucophage can cause hypovitaminosis B12 . In addition, the possibility of developing megaloblastic anemia and skin rash .
Glucophage tablets, instructions for use (Method and dosage)
According to the instructions for Glucophage, the dosage of the drug is selected individually and depends on the glucose level in the blood.
In this case, the instructions for use of Glucophage 1000 mg, Glucophage 850 mg and Glucophage 500 mg at the beginning of treatment recommend taking a daily dose of 500-1000 mg. After 10-15 days of therapy, a gradual increase in dose is allowed, taking into account the level of glycemia. On average, the maintenance daily dose is 1.5-2 g, but not more than 3 g. In order to reduce side effects associated with the gastrointestinal tract, the daily dose is divided into 2-3 doses.
It is recommended to take these tablets simultaneously or immediately after meals as a whole. The duration of therapy is selected individually. When taking this drug for weight loss, specialist supervision is necessary.
GLUCOPHAGE (tablets)
has a progressive effect on the gastrointestinal tract.
I took glucophage after breakfast in the morning or sometimes with breakfast, that is, not on an empty stomach. Glucophage tablets are large in size. Well, let's just say that they are much larger than the usual standard tablet sizes. At first, swallowing a large tablet caused an unusual slight discomfort and I had to take it with an extra portion of water. But gradually I got used to it and somehow got used to it in my own way. The tablet is round and convex white on both sides, covered with a film. The tablet has a slightly bitter taste, but this is not critical for me. My feelings after taking the glucophage tablet. For a long time after taking the pill you don’t feel like eating at all, that is, your appetite has noticeably decreased. And I began to eat smaller portions, that is, satiation with food comes faster. And at times, after eating, I even felt an attack of mild nausea. The craving for sweets disappeared after taking the pill. My blood glucose level did not rise much after eating. That is, the drug coped with its purpose with a plus.
It perfectly keeps glucose levels within normal limits. I have never observed a sharp drop in glucose either, and that’s very good. Because an excessively rapid decrease in blood glucose is a very dangerous thing. I liked that while taking the drug there was no unpleasant aftertaste after waking up in the morning. But I must say that this taste happened quite often in the mornings when I was taking sulfonylurea-based hypoglycemic drugs.
Before glucophage, I took drugs based on sulfonylureas; anyone who took them, I think, knows the principle of action of such drugs. Such drugs promote the production of insulin in the human body. Glucophage, like all metformin-based drugs, does not promote insulin production. It acts on the intestinal walls, thereby delaying the absorption of glucose by the intestines. The principle of action of the drugs is radically different. And I would also like to mention that the drug has contraindications, all of which are described in detail in the long instructions for the drug. So far I have only encountered slight nausea (and even then not often, but occasionally) perhaps it was just an effect of getting used to the new drug.
About a month ago I bought “36.6” glucophage (30 tablets with a dosage of 500 mg) at a pharmacy near my house for 115 rubles. Among its counterparts (glucose-retaining drugs), the price of glucophage is still quite affordable. This drug is produced in France. And in connection with the crisis, I would really not like a sharp rise in the price of such a vital and necessary drug; I hope this will not happen.
Overdose
There were no cases of overdose while taking the drug Glucophage. However, the development of lactic acidosis .
Early symptoms of this disorder are characterized by:
- nausea;
- vomit;
- diarrhea;
- pain in the muscles and abdomen;
- increase in body temperature.
Complicated cases may be accompanied by:
- increased breathing;
- dizzy;
- disturbance of consciousness;
- development of a coma.
lactic acidosis occurs, you should immediately stop taking Glucophage and determine the lactate concentration in a hospital setting, which will help clarify the diagnosis. In the future, it is possible to use hemodialysis, which allows you to remove lactate and drug components from the body. Then symptomatic therapy is performed.
Interaction
The simultaneous use of this drug and danazol may lead to the development of hyperglycemic effects. If necessary, such a combination requires dosage adjustment and glycemic control.
Taking high doses of Chlorpromazine increases glycemia, reducing insulin release. Any hormonal drugs reduce glucose tolerance, increasing glycemia, and can cause ketosis.
Combination with loop diuretics maintains the risk of lactic acidosis due to functional renal failure .
β2-adrenergic receptor stimulants can increase blood glucose levels. In this case, glycemic control is necessary, and insulin may be prescribed. The combination of Glucophage and sulfonylurea , insulin , acarbose , and salicylates enhances the hypoglycemic effect.
Oral medications for type 2 diabetes
The list of hypoglycemic drugs is so impressive that even patients with diabetes sometimes have a very poor understanding of this variety of medications. Six pharmacological groups, which differ in their mechanism of action and have their own positive and negative sides, and dozens of drugs used for type 2 diabetes, create confusion in the minds of consumers. Let's try to put everything on the shelves.
Six groups
So, modern oral hypoglycemic agents belong to one of six groups:
- Biguanides are the main representative of metformin, which we have already written about.
- Sulfonylurea derivatives - glibenclamide, gliclazide, glimepiride, glipizide.
- Alpha-glucosidase inhibitors - acarbose, miglitol.
- Thiazolidinediones, or glitazones - pioglitazone, englitazone.
- DPP-4 inhibitors, or gliptins - sitagliptin, vildagliptin, saxagliptin.
- SGLT2 inhibitors - dapagliflozin, canagliflozin, empagliflozin.
Despite the names of pharmacological groups that are difficult for the inexperienced consumer to perceive, the mechanism of action of the drugs included in their composition is quite transparent, and the advantages and disadvantages are obvious. And, putting aside the fear of terms, let’s get to know them better.
Sulfonylurea derivatives
They “force” the body to produce (secrete) insulin, which is why they are sometimes called secretagogues.
How do they work?
Sulfonylurea derivatives bind to receptors located on the membranes of pancreatic beta cells. This triggers a sequence of events within the cells that results in an increase in the amount of insulin produced by the beta cells. Reduce the level of glycated hemoglobin (HbA1c - an indicator that reflects the level of glucose in the blood over a long period of time) by an average of 1-2%.
Who is it prescribed to?
Drugs in this group are prescribed for type 2 diabetes, when the level of glycated hemoglobin is above 6.5%. As a rule, they are approached in the absence or insufficient response to treatment with metformin.
Advantages:
- Affordable price.
- Fast onset of action.
- No effect on pressure levels.
- Convenient dosing.
- Reduction of microvascular complications (retinopathy, neuropathy).
Flaws:
- Risk of hypoglycemia.
- Gain in body weight.
- Low long-term effect.
Alpha-glucosidase inhibitors
Drugs in this group slow down the absorption of carbohydrates from food and the flow of glucose into the blood. Reduce HbA1c levels by 0.5–0.8%.
How do they work?
The mechanism of action is based on blocking intestinal enzymes - alpha-glucosidase - which are involved in the breakdown of saccharides.
Who is it prescribed to?
Drugs in this group are used when difficulties arise in controlling glucose levels after meals.
Advantages:
- The ability to reduce glucose levels after meals (postprandial), especially in combination with other glucose-lowering drugs.
- Low risk of hypoglycemia.
- No effect on body weight.
- Reduced triglyceride levels.
Flaws:
- Low hypoglycemic activity.
- Side effects from the gastrointestinal tract.
- Inconvenient dosing (need for frequent selection, dose titration).
- High price.
Thiazolidinediones
Drugs in this group increase the body's sensitivity to insulin, which is why they are sometimes called insulin sensitizers. HbA1c levels decrease by 0.5–1.4% when taking thiazolidinediones.
How do they work?
Thiazolidinediones bind to PPARg receptors, which are found in the liver, vascular endothelium, adipose and muscle tissues. This leads to an increase in the synthesis of proteins involved in glucose metabolism.
Who is it prescribed to?
Drugs in this group are used in cases where metformin or sulfonylurea derivatives are poorly tolerated or do not compensate for diabetes.
Advantages:
- Low risk of hypoglycemia.
- Long-term effect.
- Increasing the level of “good” cholesterol, decreasing the level of triglycerides (pioglitazone).
- Reducing the risk of coronary heart disease (pioglitazone).
Flaws:
- Gain in body weight.
- Fluid retention in the body.
- Contributes to the destruction of bone tissue and frequent bone fractures.
- Increased levels of “bad” cholesterol.
- High price.
DPP-4 inhibitors
This is a fairly new class of oral hypoglycemic drugs that can reduce HbA1c levels by 0.5–0.8%, as well as reduce body weight.
How do they work?
Drugs of this class block the action of the DPP-4 enzyme, which destroys a group of gastrointestinal hormones - incretins. Incretins help stimulate the production of insulin when it is needed (for example, after meals), and also reduce the liver's production of glucagon when it is not needed (during digestion). In addition, they slow down digestion and reduce appetite.
Who is it prescribed to?
DPP-4 inhibitors are considered second or third line drugs. They are used if treatment with metformin and sulfonylurea derivatives has not given the desired result. They often become an alternative to thiazolidinediones.
Advantages:
- Low risk of hypoglycemia.
- Good tolerance.
- Decreased appetite (used for increased body weight or obesity).
Flaws:
- Not as intense a decrease in HbA1c compared to drugs from other groups.
SGLT2 inhibitors
The newest class of glucose-lowering drugs. Their action is based on the ability to “help” the kidneys reduce blood glucose levels. Approved by one of the most authoritative health organizations in the world, the American Food and Drug Administration (FDA), for the treatment of diabetes in 2013.
How do they work?
The kidneys constantly filter glucose from the blood, after which it returns to the bloodstream again - glucose is reabsorbed. This process involves proteins called sodium-glucose glucose cotransporters - SGLT1 and SGLT2. SGLT2 inhibitors block type 2 proteins, causing less glucose to return to the blood and more to be excreted from the body in the urine.
Who is it prescribed to?
Drugs in this group are used in cases of insufficient response to treatment with metformin and insulin. They are not recommended for patients with impaired kidney function (nephropathy), since in such cases the effectiveness of SGLT2 inhibitors is reduced.
Advantages:
- High hypoglycemic activity.
- Loss of body weight.
Flaws:
- Risk of urinary tract infections.
- Risk of hypoglycemia.
- High price.
Marina Pozdeeva
Photo istockphoto.com
Products by topic: (metformin), (glibenclamide), (gliclazide), (glimepiride), (acarbose), [product strict="sitagliptin"](sitagliptin), (vildagliptin), (saxagliptin), (dapagliflozin), (canagliflozin ),(empagliflozin)
Analogs
Level 4 ATX code matches:
Bagomet
Diaformin
Metformin
Formetin
Gliformin
Glucophage Long
Siofor
The main analogues are represented by the following drugs:
- Siofor
- Glucophage Long
- Metformin
- Gliformin
- Merifatin
- Formetin
- Diasfor
- Metadiene
- Diaformin
- Rinformin
Glucophage for weight loss
It should be noted that this drug is very popular among people who are losing weight. However, reviews from doctors report that this method of combating excess weight is very dangerous and can cause serious complications. However, this particular method is discussed on various forums where users are interested in how to take Glucophage for weight loss?
At the same time, some people recommend taking Glucophage 500 mg, explaining that this dosage will be enough to “start metabolic processes.” Others, on the contrary, advise Glucophage 850 mg, since a higher dosage “will only speed up the process.”
It is interesting that reviews for losing weight with this drug do not describe specific results. But at the same time, there are reports of a deterioration in general health, the development of abdominal pain, nausea and even vomiting. Therefore, experts advise starting to monitor your diet, which should be nutritious. It is necessary to exclude sweets, flour and fatty foods from the diet and increase physical activity.
Reviews of Glucophage
In most cases, discussions of this drug are related to its use for weight loss. At the same time, some reviews of those losing weight about Glucophage report that their doctor recommended this method to them, since diets and physical activity did not help eliminate excess weight. Other users are interested in how to take this medicine to quickly lose extra pounds. In addition, you can find stories from patients who took these pills to restore reproductive function.
However, using the drug for such purposes is not always effective. Moreover, both reviews from doctors and patients contain information about the development of serious pathologies against the background of such experiments.
Reviews of Glucophage for weight loss also do not describe specific results. Although patients who take the medicine for diabetes note its effectiveness and gradual loss of body weight.
The effectiveness of Glucophage in the prevention of type 2 diabetes mellitus
WITH
Diabetes mellitus (DM) is one of the most common, high-cost chronic diseases and is a serious health problem in all countries of the world, both industrialized and developing.
The number of people with diabetes mellitus currently amounts to 177 million people
. Moreover, the majority of patients (90%) are patients with type 2 diabetes mellitus. In all countries, an increase in the incidence of diabetes mellitus is observed almost everywhere. In a little less than 20 years, the number of people with diabetes in the world has increased 6 times. According to forecasts, if such growth rates are maintained, by 2010 the number of people with diabetes mellitus on the planet will reach 221 million people, and by 2025, more than 300 million people will have diabetes mellitus [1]. This means that by 2025, the prevalence of diabetes in economically developed countries will be 7.6%, in developing countries - 4.9%.
Due to the fact that type 2 diabetes mellitus often goes undiagnosed for a long time, its actual prevalence is estimated to be 2–3 times higher than reported [2]. The Australian Diabetes, Obesity and Lifestyle Study ( AusDiab
) it is shown that for every diagnosed case of DM2 there is one undiagnosed [3].
The Third National Health and Nutrition Examination Survey ( NHANES lll
) conducted in the USA also revealed a high prevalence of undiagnosed T2DM among the population - on average it is 2.7%, and among men and women aged 50-59 years - 3.3% and 5.8%, respectively [4].
Type 2 diabetes is characterized by the development of severe disabling complications leading to complete disability and premature mortality. According to the study Cost of Diabetes in Europe – Type 2 ( CODE-2
), who studied the prevalence of various diabetic complications in patients with diabetes mellitus (the average age of those examined was 67 years), 59% of patients had various complications, with 23% of those examined having two and 3% having three complications of type 2 diabetes. Cardiovascular pathology was discovered in 43%, cerebrovascular – in 12% of patients [5]. It has been established that with existing T2DM, the risk of developing cardiovascular pathology is 3–4 times higher than in its absence. Patients with type 2 diabetes have the same risk of premature death as patients who have had a myocardial infarction without type 2 diabetes [6]. In most developed countries of the world, diabetes mellitus ranks 3–4 in the overall mortality structure and is the leading cause of blindness and visual impairment in the adult population.
In the United States and several European countries, the cost of treating T2DM and its complications already exceeds 15% of annual healthcare costs.
Insulin resistance (IR) and insufficient insulin secretion play a leading role in the development of T2DM. It is assumed that insulin resistance initially develops and progresses in genetically predisposed individuals. Under IR conditions, there is a decrease in the supply of glucose to insulin-dependent tissues (muscle, fat), and an increase in glucose production by the liver, which contribute to the development of hyperglycemia. With adequate ability of b-cells to compensate for increased glucose levels by excess insulin production, the state of normoglycemia is maintained. However, subsequently, as the severity of IR increases, the insulin secretory ability of b-cells is depleted and they cease to cope with the increasing load of glucose. Initially, this is manifested by the development of hyperglycemia in the postprandial period. An example of postprandial hyperglycemia is impaired glucose tolerance (IGT). IGT is diagnosed using an oral glucose tolerance test (OGT). The diagnostic criteria for IGT are: fasting glucose (capillary blood) < 6.1 mmol/l; glycemia 2 hours after a load of 75 g of glucose is 7.8 and 11.1 mmol/l.
With further progression of impaired insulin secretion by b-cells and persisting insulin resistance, the state of IGT turns into type 2 diabetes mellitus. It has been established that annually in 5-10% of patients IGT turns into diabetes mellitus
, over a five-year period in 20–35% of people, and with a combination of fasting glycemia (i 5 mmol/l) and IGT in 38–65%.
The prevalence of IGT in the world is quite high - about 314 million people have impaired glucose tolerance, and by 2025 it is predicted to increase to 472 million. According to P. Zimmet, about a quarter of the population of Western European countries have impaired glucose tolerance or metabolic syndrome [7 ]. It is known that insulin resistance also plays a leading role in the mechanisms of development of metabolic syndrome. The main clinical manifestations of metabolic syndrome are type 2 diabetes mellitus, coronary heart disease or other manifestations of atherosclerosis. Many people consider metabolic syndrome as a prelude to diabetes.
In the general population, the prevalence of metabolic syndrome is quite high and ranges from 14% to 24%. The United States of America leads in the prevalence of metabolic syndrome; metabolic syndrome is relatively common in northern European countries. According to the results of a study conducted in Finland and Sweden, 10% of women and 15% of men have metabolic syndrome in the absence of carbohydrate metabolism disorders, 42% and 64% have increased fasting glycemia and/or IGT, and 78% and 64% have diabetes mellitus, respectively. 84% [8].
As epidemiological studies have shown, even with IGT, the incidence of ischemic heart disease is 2 times, and mortality from cardiovascular diseases is 1.5 times higher than without disorders of carbohydrate metabolism [9]. Impaired glucose tolerance is an independent risk factor for premature mortality from cardiovascular diseases. With metabolic syndrome, the risk of developing coronary heart disease and stroke is 3 times higher than without it
.
By the time of clinical manifestation of T2DM, about 50% of patients already have various macrovascular complications. And retinopathy, peripheral neuropathy and proteinuria, as shown by the UKPDS
(UK prospective Diabetes Study), are respectively present in 35%, 12% and 2% of patients with newly diagnosed type 2 diabetes mellitus [10].
That is, individuals with elevated fasting glucose and/or IGT have a high risk of developing not only diabetes, but also cardiovascular diseases. Therefore, already in the early stages of carbohydrate metabolism disorders, it is extremely important to carry out active measures aimed at preventing the progression of carbohydrate metabolism disorders and reducing the risk of developing cardiovascular diseases.
It has been established that environmental factors - excess nutrition and a sedentary lifestyle lead to an increase in body weight and contribute to the development and aggravation of insulin resistance - the leading pathogenetic link in the development of type 2 diabetes mellitus.
The most important among the leading modifiable risk factors for the development of T2DM is obesity. Epidemiological studies indicate a higher prevalence of IGT and diabetes mellitus among individuals with obesity than without it, and a beneficial effect of weight loss on carbohydrate metabolism in individuals with diabetes and obesity. Therefore, it can be assumed that improving diet and increasing physical activity, leading to weight loss, will help delay or prevent the development of type 2 diabetes in people at high risk of developing the disease.
In this regard, several prospective studies have been conducted in America, Europe and China on the effectiveness of lifestyle changes in the prevention of type 2 diabetes, both without and in combination with drugs that reduce insulin resistance used to treat type 2 diabetes.
In the United States, a randomized clinical trial was initiated in 1998 by the Diabetes Prevention Program research group .
(DPP), the purpose of which was to study the effect of intensive lifestyle changes and the use of
metformin (Glucophage)
on preventing or delaying the manifestation of diabetes in individuals at high risk of developing it [11]. The study also compared the effectiveness of these interventions in people of different ages, gender, weight, race and ethnicity. The duration of the study was 2.8 years.
Glucophage, an antihyperglycemic drug from the biguanide group that does not have a hypoglycemic effect, has been used to treat type 2 diabetes mellitus for more than 40 years. The drug improves the sensitivity of peripheral tissues to insulin, reduces glucose production by the liver by influencing gluconeogenesis, and reduces glycogenolysis [12]. Numerous experimental and clinical studies have shown that Glucophage has a beneficial effect on blood lipid levels, the hemostasis system (reducing levels of plasminogen activator inhibitor-1 and von Willebrandt factor), inhibits the absorption of glucose in the intestine, and also has a weak anorexigenic effect. It is the only antidiabetic drug that has a proven effect on reducing the incidence of complications of type 2 diabetes mellitus. Thus, the UKPDS study showed a reduction in overall mortality - by 36%, mortality associated with diabetes, myocardial infarction and stroke - by 42%, 39%, respectively. and 41% in overweight patients with type 2 diabetes who received Glucophage, compared with patients on insulin or sulfonylurea therapy, with the same degree of compensation for carbohydrate metabolism [13]. A study conducted in Canada over 5 years and covering 12,000 patients with type 2 diabetes demonstrated a 40% reduction in overall and cardiovascular mortality among patients receiving Glucophage monotherapy or in combination with other antidiabetic drugs, compared with patients taking drugs sulfonylureas [14]. The positive effect of Glucophage on risk factors for cardiovascular diseases was revealed not only in patients with type 2 diabetes mellitus, but also in patients with metabolic syndrome and polycystic ovary syndrome. Randomized placebo-controlled trials BIGuanides and Prevention of the Risk of Obesity
(BIGPRO), which included 324 patients with abdominal obesity, showed that the use of Glucophage was accompanied by more pronounced reductions in body weight, plasma insulin, total cholesterol and fibrinolysis parameters (tissue-type plasminogen activator and von Willebrand factor) compared with placebo [15]. Published data on the use of Glucophage in obese patients and men with arterial hypertension showed that the use of Glucophage was accompanied by a decrease in body weight, blood pressure, insulin, improvement in the lipid profile and fibrinolytic activity of the blood [16]. A number of experimental and clinical studies have revealed a direct beneficial effect of Glucophage on microcirculation and endothelial function [17,18].
The above properties of Glucophage, especially the effect on insulin resistance and associated disorders, as well as the results of the use of the drug in clinical practice, suggested that the administration of Glucophage to individuals at high risk of developing diabetes will reduce this risk and thereby have a preventive effect regarding the development of diabetes mellitus .
All those included in the study had impaired glucose tolerance: fasting plasma glucose 5.3–6.9 mmol/l and from 7.8 to 11.0 mmol/l 2 hours after a load of 75 g of glucose. Inclusion criteria for the study were also: age 25 years, BMI 25 kg/m2 (for Asian Americans 22 kg/m2).
The study did not include persons taking drugs that affect carbohydrate metabolism or having severe somatic diseases.
The study included 3234 people (32.3% men and 67.7% women), average age 50.6±10.7 years, weight 94.2±20.3 kg, who had various risk factors for developing type 2 diabetes: hereditary predisposition to DM2 – 69.4%; history of gestational diabetes mellitus – 16.1% of women; BMI – 34.0±6.7 kg/m2 and specific ethnicity – African Americans (20%), Hispanic Americans (16%), Asian Americans (4%) and American Indians (5%).
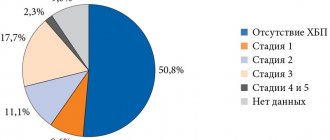
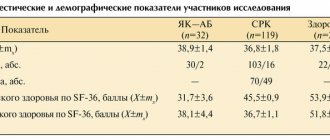
Clinical and laboratory characteristics of the study participants are presented in Table 1.
The 3,234 people included in the study were randomized into three groups: a group receiving Glucophage + standard lifestyle recommendations (1,073 people), a placebo group + standard lifestyle recommendations (1,082 people), and a group receiving intensive lifestyle changes. life (1079 people) (Fig. 1).
Rice. 1. Study design
Glucophage was prescribed for the first month at 850 mg once a day, and then at 850 mg twice a day. Standard recommendations for lifestyle changes included written information and annual 20–30 minute conversations on nutrition and increasing physical activity. In the intensive lifestyle change group, 16 individual sessions on changing diet and increasing physical activity were conducted during the first 6 months of the study, and then individual and group sessions were conducted monthly throughout the observation period. This group was given a goal of achieving 7% weight loss and weight maintenance during the study period by following a low-calorie, low-fat diet combined with 150 minutes of moderate-intensity walking per week. The average reduction in daily caloric intake was: in the placebo group – 249±27 kcal, in the Glucophage group – 296±23 kcal and in the intensive lifestyle group – 450±26 kcal (pЈ0.001). Diabetes mellitus was diagnosed according to the criteria of the American Diabetes Association (1997): plasma glucose on an empty stomach is 7 mmol/l and two hours after taking 75 g of glucose is 11.1 mmol/l.
Research results
Of the intensive lifestyle intervention group, 50% of study participants achieved target weight loss (7%) by week 24 of follow-up and 38% maintained this weight loss to the end of the study, 74% of participants were able to maintain the recommended exercise regimen during the first 6 months of the study and 58 % until the end of the study. In the Glucophage group, weight loss was 2.1 kg, in the placebo group - 0.1 kg and intensive lifestyle changes - 5.6 kg (p < 0.001). Initial fat intake averaged 34.1% of daily calories, in the Glucophage and placebo group it decreased by an average of 0.8 ± 0.2%, and in the intensive lifestyle change group by 6.6 ± 0.2% ( p<0.001).
Impact on the prevention of diabetes mellitus 2
The results of the study showed that the incidence of diabetes mellitus in the placebo group per year was 11%, while in the Glucophage group it was 7.8%, and in the intensive lifestyle change group it was 4.8% (Fig. 2).
Rice. 2. Annual incidence of diabetes mellitus
After 2.8 years, the use of Glucophage was accompanied by a reduction in the risk of developing type 2 diabetes by 31% (p<0.001), and intensive lifestyle changes by 58% (p<0.001) compared with placebo (Fig. 3).
Rice. 3. The effect of Glucophage and intensive lifestyle changes on the risk of developing T2DM
The cumulative incidence of diabetes mellitus in the intensive lifestyle intervention group and the metformin group was lower than in the placebo group and was 28.9%, 21.7% and 14.4% in the placebo, Glucophage and intensive lifestyle intervention groups, respectively.
The use of Glucophage was also more effective in preventing diabetes mellitus
in study subjects with metabolic syndrome compared to placebo.
The effectiveness of intensive lifestyle changes in reducing the incidence of type 2 diabetes did not depend on the gender, ethnicity and race of the individuals studied, and Glucophage did not depend on gender and ethnicity
However, in young patients (Ј 44 years old), the effectiveness of Glucophage in the prevention of diabetes mellitus was higher than in older age groups and was comparable to that of an intensive lifestyle - 44% and 48%, respectively (Fig. 4).
Rice. 4. Reducing the risk of developing type 2 diabetes depending on age
It was also noted that in case of massive obesity (BMI 35), the effectiveness of Glucophage did not differ from intensive lifestyle changes in reducing the incidence of diabetes mellitus. The administration of Glucophage to such patients was accompanied by a reduction in the incidence of type 2 diabetes by 53%, and intensive lifestyle changes by 51% compared to placebo (Fig. 5).
Rice. 5. Reduced risk of development depending on BMI
That is, the study showed the dependence of the effectiveness of Glucophage on the age and BMI of the subjects studied, indicators that determine the risk of developing type 2 diabetes and cardiovascular diseases. It should also be noted that there were no significant changes in lifestyle in the group of people receiving Glucophage.
Intensive lifestyle changes and the use of Glucophage contributed to the normalization of plasma glucose levels both on an empty stomach and after a glucose load. There was equal effectiveness of Glucophage and active lifestyle changes in normalizing fasting glucose levels, and higher effectiveness of lifestyle in reducing postprandial glycemia. This may be due to the mechanism of action of the drug (inhibition of glucose production by the liver). During the study, no serious side effects associated with taking Glucophage were recorded. However, in the Glucophage group, gastrointestinal disorders were observed more often than in other groups of subjects studied.
Thus, the results of the study confirmed the assumption that the development of T2DM can be prevented or delayed in individuals at high risk of developing the disease.
Taking Glucophage by persons with IGT for 2.8 years reduced the relative risk of developing type 2 diabetes mellitus by 31%, without significant changes in lifestyle. Intensive lifestyle changes, although more effective in reducing the incidence of type 2 diabetes (the risk of development decreased by 51%), but required significant efforts from specialists and participants in meeting the requirements for changes in diet and physical activity. The positive effect of intensive lifestyle changes on the risk of developing type 2 diabetes once again confirmed the importance of obesity and physical inactivity in the development of insulin resistance, IGT and type 2 diabetes. The study showed for the first time the effectiveness of drug prevention of the development of type 2 diabetes using the drug Glucophage. Undoubtedly, the results obtained will be an important step towards solving the problem of the epidemic of type 2 diabetes. References:
1. King H., Aubert R., Herman W. Global burden of diabetes 1995–2025. Diabetes Care, 1998; 21: 1414–31.
2. Dedov I. I., Suntsov Yu. I., Kudryakova S. V. Epidemiology of diabetes mellitus. Diabetes. Guide for doctors. auto Dedov I.I., Shestakova M.V. Universum Publishing. M., 2003; 75–93.
3. Dunstan D., Zimmet P., Welborn T. et al. The rising prevalence of diabetes and impaired glucose tolerance. The Australian diabetes, obesity and lifestyle study. Diabetes Care, 2002; 25:829–34.
4. Harris M., Goldstein D., Flegal K. et al. Prevalence of Diabetes, Impaired Fasting Glucose, and Impaired Glucose Tolerance in US Adults. The Third National Health and Nutrition Examination Survey, 1988–1994. Diabetes Care, 1998; 21:518–24.
5. Liebl A., Neiss A., Spannheimer A. et al. Complications, co-morbidity, and blood glucose control in type 2 diabetes mellitus patients in Germany – results from the CODE2 study. Exp Clin Endocrinol Diabetes 2002; 110:10–6.
6. Haffner S., Lehto S., Ronemma T., Pyorala K., Laakso M. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med 1998; 339:229–34.
7. Zimmet P. The burden of type 2 diabetes: are we doing enough? Diabetes Metabolism, 2003; 29: 6S9–6S18.
8. Isomaa B., Almgren P., Tuomi T., Forsen B. et al. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care, 2001; 24: 683–9.
9. Saydah S., Miret M., Sung J., Varas C. et al. Postchallenge hyperglycaemia and mortality in a national sample of US adults. Diabetes Care, 2001; 24: 1397–402.
10. UK Prospective Diabetes Study (UKPDS) Group. Intensive blood control with sulphonylurea or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet, 1998; 352:837–53.
11. Diabetes Prevention Program Research Group. Reduction in the Incidence of Type 2 Diabetes with Lifestyle Intervention or Metformin, The New England Journal of Medicine, 2002; 346:393–403.
12. Giannarelli R., Aragona M., Coppelli A., Del Prato S. Reducing insulin resistance with metformin: the evidence today. Diabetes Metabolism, 2003; 29: 6S28–6S35.
13. UK Prospective Diabetes Study (UKPDS) Group. Effect of intensive blood–glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet, 1998; 352:854–65.
14. Johnson J., Simpson S., Majumdar S., Toth E. Decreased mortality associated with the use of metformin compared with sulphonylurea monotherapy in type 2 diabetes. Diabetes Care, 2002; 25:2244–8.
15. Charles A., Vague P., Morange P. et al. Effect of weight change and metformin on fibrinolysis and the von Willebrand factor in obese nondiabetic subjects. The BIGPROl Study. Diabetes Care, 1998; 11: 1967–72.
16. Despres J. Potential contribution of metformin to the management of cardiovascular disease risk in patients with abdominal obesity, the metabolic syndrome and type 2 diabetes. Diabetes Metabolism, 2003; 29: 6S53–6S61.
17. Chan N. Improved endothelial function with metformin in type 2 diabetes mellitus. JAM Coll Cardiol 2001;38:2131–2
18. Bouskela E., Cyrino F., Wiernsperger N. Effect of insulin and the combination of insulin plus metformin (glucophage) on microvascular reactivity in control and diabetic hamsters. Angiology, 1997; 48:503–14.
Glucophage price, where to buy
Price Glucophage 850 mg 30 tablets - about 200 rubles.
The medicine Glucophage, intended specifically for weight loss, is not available.
- Online pharmacies in UkraineUkraine
- Online pharmacies in KazakhstanKazakhstan
Pharmacy24
- Glucophage 500 mg N30 tablets Merck Sante S.A.S., France/Merck, SL, Spain
67 UAH. order - Glucophage 500 mg N60 tablets Merck Sante S.A.S., France/Merck, SL, Spain
127 UAH order
- Glucophage 1000 mg N60 tablets Merck Sante S.A.S., France/Merck, SL, Spain
255 UAH order
- Glucophage 850 mg No. 30 tablets Merck Sante S.A.S., France/Merck, SL, Spain
96 UAH order
- Glucophage 850 mg No. 60 tablets Merck Sante S.A.S., France/Merck, SL, Spain
172 UAH order
PaniPharmacy
- Glucophage tab. p/o 1000 mg No. 30 France, Merck Sante
130 UAH order
- Glucophage tablets 500 mg No. 30 Australia, Nycomed
80 UAH order
- Glucophage XR tablet prol. valid 500 mg No. 60 France, Merck Sante
261 UAH. order
- Glucophage tablets, coated 850 mg No. 30 France, Merck Sante
90 UAH order
- Glucophage film-coated tablets 1000 mg No. 60 France, Merck Sante
255 UAH order
show more