Introduction of volume-forming preparations (gels) into the submucosal layer of the urethra
The essence of this technique comes down to the formation of peculiar “pillows” under the urethral mucosa (as with the Mantoux test on the skin of the forearm). As a result of the introduction of the gel at several points, the lumen of the urethra narrows, and the prerequisites are created for better urinary retention. This method of treating stress urinary incontinence, especially in older women, is captivating with its “simplicity” - it is performed under local anesthesia, the operation lasts only 5-10 minutes. The operation is usually performed using a cystoscope through the lumen of the urethra. There are techniques that do not even require a cystoscope.
Unfortunately, despite the considerable cost, the effectiveness of this operation is significantly inferior to surgical treatment.
Repeated injections of the drug are often required. It is also not entirely clear how “harmless” the gels used are for the urethra and paraurethral tissues, especially with repeated administrations. However, there are a number of clinical situations where the introduction of gels is indeed preferable.
Anterior colporrhaphy or anterior vaginalplasty
Currently, it is the most common operation performed in gynecological hospitals for stress urinary incontinence in women (in its pure form or in combination with cystocele-prolapse of the bladder). “Colporrhaphy” literally means “suturing the vagina.” When performing this operation, a midline incision is made in the vagina, tissue dissection is carried out in lateral directions. Then the isolated tissues surrounding the urethra and bladder are bunched up (pulled together) along the midline using special absorbable sutures. As a result, “support” of the urethra is created for some time, allowing urine to be retained.
After a year, the effectiveness of this operation is no more than 50-60 percent, and after 3 years - 25 percent.
At the same time, this manipulation can greatly complicate the performance of modern operations to eliminate urinary incontinence (after childbirth), since after it pronounced fibrosis (scarring) of the tissue develops. In modern conditions, the indications for anterior colporrhaphy are extremely narrow! Anterior colporrhaphy as an “anti-stress” operation for urinary incontinence should generally be considered archaic. Unfortunately, this archaism continues to be widespread.
Uro-Vaxom®
Activation of the immune response after oral administration of the drug Uro-Vaxom® begins in the area of Peyer's patches of the small intestine. Strengthening the immune response in the genitourinary tract under the influence of the drug Uro-Vaxom® occurs in two directions:
1. Activation of the humoral immune response (activation of T- and B-lymphocytes, synthesis of various anti-E. coli antibodies, synthesis of class A immunoglobulin).
2. Activation of a nonspecific immune response (macrophages and NK cell phagocytosis).
Thanks to this activation, Uro-Vaxom® is effective against not only E. coli, but also against other uropathogens, including various serotypes of E. coli and/or pathogens belonging to other bacterial genera.
In vitro studies have shown that Uro-Vaxom® stimulates the activity of macrophages and neutrophils, activates the maturation of dendritic cells and increases the expression of adhesion molecules by neutrophils. The activation and maturation of dendritic cells are central to the cellular response to trigger an appropriate immune response in the intestine.
Due to the activation of B lymphocytes, the synthesis of immunoglobulin A increases, incl. in urine. In addition, studies on mice have shown that Uro-Vaxom® increases the activity of leukocytes in the blood and the secretion of tumor necrosis factor alpha (TNF-alpha), interleukin-6 (IL-6), interleukin-12 (IL-12), interferon -alpha (IFN-alpha) by peritoneal cells, as well as immunoglobulin G (IgG) in spleen cell culture. The molecular mechanism by which Uro-Vaxom® stimulates innate immune cells is likely related to its ability to activate pattern recognition receptors (PRRs). In vitro studies using HEK.293 cell lines with the expression of membrane and cytoplasmic pattern recognition receptors (Toll-like receptors (TLRs) or Nod-like receptors (Nod)) and the presence of reporter genes, it was found that the components contained in the drug Uro-Vaxom® are recognized by receptors TLR2 and TLR4 and to a lesser extent Nod2, but are not recognized by receptors such as TLR3, TLR5, TLR7, TLR8 or TLR9. Activation of these receptors, associated with pathogen-associated molecular patterns (PAMPs), including small molecules of the bacterial wall from the drug Uro-Vaxom®, triggers a cascade of immune reactions.
The drug Uro-Vaxom® promotes the following effects:
— stimulates T and B lymphocytes;
— stimulates the activity of dendritic cells, macrophages, NK cells and neutrophils;
- induces the formation of endogenous interferon (IFN), tumor necrosis factor alpha (TNF-alpha), interleukin-6 (IL-6), interleukin-12 (IL-12);
— increases the content of immunoglobulin A (IgA), including in the urine.
The drug Uro-Vaxom® has an immunostimulating effect and activates B lymphocytes (production of polyclonal antibodies), macrophages (impact on the function of phagocytosis) and dendritic cells (activation of maturation markers).
When taking the drug Uro-Vaxom®, the frequency of relapses of urinary tract infections, especially cystitis, decreases.
Colposuspension according to Birch
It consists of suspending the tissues surrounding the urethra to the strong structures of the anterior abdominal wall - the inguinal ligaments (Cooper). The operation is performed via abdominal access (through the abdomen). Surgical approach: either open or laparoscopic. For a long time, this operation was considered! "gold standard" in the treatment of stress urinary incontinence in women.
With the advent of operations to install a synthetic midurethral sling, Birch colposuspension lost its position.
Its long-term effectiveness “in capable hands” is up to 70-80 percent. The main disadvantages of this technique are: the need for anesthesia with artificial ventilation and the strong dependence of the results on the qualifications of the surgeon.
Implantation of a synthetic midurethral sling (sling operation, TVT-O, TOT, etc.)
The midurethral sling is the most studied and, at the same time, the most effective treatment method for stress urinary incontinence (SUI). It would seem, what else can be said about the technique, which over 20 years, even in the era of “mesh wars,” has become the gold standard for the treatment of SUI, confidently positioned in all clinical recommendations?
We invite you to think about the very essence of this operation.
It is performed to restore urinary continence while maintaining normal urination (!).
The placement of a midurethral sling is a classic example of functional surgery. Unfortunately, many experts think in terms of “cut and sew” and firmly believe that the very fact of “correct” installation of the sling is quite enough for its correct operation. This is wrong. And practice eloquently demonstrates this. We are not surprised when a watchmaker, after replacing a part, asks for a few more days to adjust the correct movement of the mechanism. What can we say about the patient - we are introducing an artificial part into an already debugged system that has existed for years. Ideally, the implant should adapt as much as possible to the anatomy and physiology of the recipient, and not vice versa.
A few years ago, we also sincerely believed that sling implantation was a very simple and effective operation. At that time, the clinic performed no more than 100 operations per year. But a multiple increase in the number of patients and a more thorough postoperative examination showed that not everything was so good - in some patients the tension of the prosthesis was insufficient, in others it was excessive. In the first case, this was manifested by insufficient effectiveness, and in the second (much more unfavorable) - by symptoms of obvious and hidden bladder outlet obstruction (presence of residual urine, symptoms of hyperactivity, etc.). The solution to this problem suggested itself - the possibility of adjusting the prosthesis after surgery.
“Why after surgery and not intraoperatively?” - the reader will ask. The fact is that up to 20% of patients lose urine only while standing. And patients urinate while sitting. In the operating room, the patient lies in the lithotomy position under anesthesia. And for an adequate “test drive” of the installed sling, a woman must be in the most natural state for her usual lifestyle: be able to walk, get up from a chair, cough and sneeze while standing, urinate on the toilet, etc. Our clinic has developed a clear algorithm for managing patients before and after surgery, including various modifications of the cough test, uroflowmetry, determination of residual urine, questionnaires, cystometry, etc.
A serious argument not in favor of the standard (i.e. unregulated sling) are the real results (without “tricks”, such as “improvement”, “good answer”, etc.) published recently (Maggiore LR et al ., 2017). If you look at the truth, the statistics are quite sad: the “honest” effectiveness of the operation does not exceed 70%, and the frequency of obstructive urination is 5-20%... In the group of complicated patients (relapses, sphincter insufficiency, hypomobile urethra, mixed urinary incontinence) the indicators even more inconclusive... It is important to note that the so-called “de novo hyperactivity”, which often occurs after sling operations, can also be a consequence of subclinical urethral obstruction. This condition is insidious in that patients have no residual urine. That is, there is no formal reason to cut the implant, but if you cut it, most patients experience obvious improvement!
This problem can only be avoided by carefully analyzing the change in uroflowmetry indicators before and the next day after surgery and having the opportunity to loosen the tension of the loop. At the end of 2015, our clinic developed the concept of an adjustable sling. It includes two main provisions:
A -
The usual endoprosthesis has become adjustable. In the central part of the well-proven Urosling (transobturator sling) and Urosling 1 (retropubic sling) implants, adjustment threads were installed, which are removed through a vaginal incision. These threads are used to loosen the tension in the loop. The ends of the implants are not cut off after surgery and serve to increase tension. After the adjustment is completed and the effectiveness of the operation is confirmed, the adjusting threads and ends of the prosthesis are removed.
IN -
The adjustment became clear and absolutely controllable. An algorithm was developed to evaluate the effectiveness of the operation and adjust the tension. The stress test is carried out both in a lying and standing position. All patients undergo uroflowmetry to determine the volume of residual urine. If insufficient tension or obstructive symptoms are detected, adjustment is performed under local anesthesia. After each adjustment, the diagnostics are repeated at least twice.
In 2021, we published the first article on the results of treating patients with primary and complicated SUI using an adjustable sling: Adjustable transobturator sling as a first-line method for surgical treatment of stress urinary incontinence
The relevance of the problem is confirmed by the interest of foreign and domestic colleagues. Our experience with the use of an adjustable sling was presented at the American Urological Association Congress in Boston (AUA 2017): The effectiveness of transobturator adjustable midurethral sling in women with complicated SUI
The use of an adjustable sling in a complicated group of patients was reported at the congress of the International Society for Continence in Florence (ICS 2017): Poster - The effectiveness of transobturator adjustable midurethral sling in women with complicated SUI.
In November 2021, the concept of an adjustable sling was highlighted at the plenary session of the Congress of the Russian Society of Urology in Moscow (ROU 2017).
An article on the use of an adjustable sling for the treatment of SUI has been accepted for publication in the International Urogynecology Journal: Adjustable transobturator sling for the treatment of primary stress urinary incontinence.
Chronic cystitis. Immunoprophylaxis of relapses. Gadzhieva Z.K.
Oksana Mikhailovna Drapkina , professor, doctor of medical sciences:
– We move on to the next message from Professor Gadzhieva Zaida Kamaludinovna “Chronic cystitis and immunoprevention of relapses.” Please.
Zaida Kamaludinovna Gadzhieva , professor, doctor of medical sciences:
– In fact, on the one hand, my task was made easier, since I knew that Grigory Georgievich would speak, so fully and comprehensively he would present the problem of both acute and recurrent cystitis, and on the other hand, let’s say, I need to present as thoroughly as possible that small part, that seemingly small part of prevention, and specifically the immunoprophylaxis of cystitis, which we will talk about today.
In my speech, perhaps I will allow myself to repeat some points, because this is very important, and we must emphasize this, and we must remember this, because without such basic things, unfortunately, cystitis was the most important thing and the first among urological diseases in women, so, unfortunately, it will probably remain so. This is a kind of scourge. There are many such sufferers. They were, are and will be. But, in fact, I love such patients, because it is interesting to invest your knowledge, your experience in them, when you really see the effect of your work, but, unfortunately, as Grigory Georgievich said, there are a lot of recurrent cystitis, and these women do not - no they return.
The slide, which probably should have been the first, was for me to emphasize how common cystitis is - it accounts for 30% of all urological diseases. If we are talking today about chronic recurrent cystitis, we mean, of course, two or more exacerbations in six months and three or more exacerbations in a year. And, as Grigory Georgievich already said, it is believed that on average 20-30% of women have a relapse attack within 3-4 months after the first exacerbation, and about 20% of women face chronic urinary tract infections in their lives.
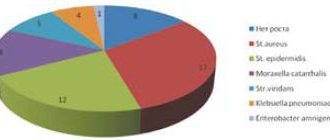
But I presented slightly earlier information than what Grigory Georgievich spoke about; he mentioned Aresk’s research. Here is a fairly large study that was carried out in Canada and several European countries. You see that almost 5,000 women took part in this study. And, despite the grandeur of this study, the result is, in principle, identical to what was presented by Professor Krivoborodov, that is, Escherichia coli as the main uropathogen accounts for the same 78-79%. A little less for other uropathogens. But we must pay attention to the fact that recently we are faced with the fact that the frequency of occurrence of the same Proteus, Klebsiella, Staphilococcus is growing. In recent years there have been more of them.
If we are talking about bacteriuria in general, then, of course, we must understand that the detection of the main uropathogens in the urine, just detection, does not give us the opportunity to make a final diagnosis. That is, in order for us to talk about true bacteriuria, we must prove that the number of these bacteria is really large. And according to all possible Guidelines, you see that clinically significant bacteriuria with a titer of monocultures of Escherichia coli and staphylococcus of 103 or more CFU/ml; monocultures of other bacteria are 104 CFU/ml and mixed cultures of two bacteria are 105 CFU/ml of urine.
A very important issue before the issue of prevention is the issue of urinary tract infections and bacteriuria in pregnant women. It is believed that about 6% of pregnant women have asymptomatic bacteriuria, despite the fact that it does not clinically cause any symptoms, which is why it is called asymptomatic bacteriuria, but what can it lead to? Look at the terrible complications: premature birth; to anemia of a pregnant woman; to preeclampsia; to malnutrition of the newborn; intrauterine fetal death. And it is believed that the risk of having children with low body weight in pregnant women who have asymptomatic bacteriuria and who have not received appropriate therapy is 1.5-2 times higher than in women without it.
As Grigory Georgievich said, what are the main goals we pursue when we talk about the treatment of uncomplicated urinary tract infection? This, of course, is the rapid elimination of clinical symptoms, eradication of the pathogen, and this is the very prevention of reinfections that we will talk about today.
Speaking about recurrent infection, as has already been emphasized, this is very important; it is a serious medical, socio-economic problem. There are different approaches to the problem of preventing this condition. Not all antibiotics are suitable for us to prevent infection. Moreover, if we are talking about antibiotics, then the questions regarding bacterial resistance, compliance, and adverse reactions are completely different. Therefore, we need to search and develop some other alternative approaches to this problem.
I found interesting data and I always try to show it, especially when I meet with other specialists, doctors of other specialties, because, fortunately or unfortunately, cystitis is, one might even say, in some way an interdisciplinary problem. Look what's happening? Who treats cystitis here? In first place, oddly enough, are not health workers at all (neighbors, friends). What was the advice? What dose was recommended? This is a big question. In second place, unfortunately, is self-medication. Patients do not reach specialists because even our elderly women have learned to use the Internet. What are they buying for themselves? This is also a big question. Today Grigory Georgievich spoke about the cost, it is desirable that the drug be of low cost. But in my practice there was a patient who found Ciprofloxacin for 28 rubles. What can you expect from this "Ciprofloxacin"? She really wanted to save money, apparently, but ended up saving on her treatment. In third place are our fellow gynecologists, because, as I already said, not at the dawn, but at the height of the 21st century, our women think that urologists are only male doctors, and do not reach a specialist in the appropriate field. Well, perhaps it is believed that it is easier for a woman to tell a gynecologist, combining all possible other problems. Well, in fourth place, finally, we are urologists, the matter has come to us. But then there are therapists, pharmacists, nephrologists - all those specialists who, willy-nilly, meet with these patients, so I believe that doctors of various specialties are probably obligated to know about what is happening in this section of medicine, because that they sometimes take the first blow. But at least you just need to send to a urologist, knowing, for example, what primary examination methods are needed to be carried out, so that the same urologist can quickly and easily make the correct diagnosis and prescribe the correct therapy.
I will periodically refer to the recommendations of the European Association of Urology, which we try to follow. There are some features that are presented in our Russian recommendations, which came out in 2012. But, for example, everything related to the prevention of recurrent urinary tract infections is here, both in our recommendations and in European ones, in principle, we follow the same rules.
As Grigory Georgievich said in his previous speech, in the first place is, of course, long-term prophylaxis using low doses of antibiotics. But, for example, if we are talking about women with postcoital cystitis, then we prescribe antibacterial drugs only when all possible behavioral methods of prevention have been exhausted. We always recommend that such women immediately after sexual intercourse urinate, after an hour it is possible to urinate again, be sure to wash themselves in order to wash away all those microorganisms that entered the external opening of the urethra during sexual intercourse with a current of urine, a stream of urine.
For women in menopause, since the main pathogenesis of the development of urinary tract infections in this category of patients is estrogen deficiency and urogenital atrophy, then the basis of pathogenetic therapy for such patients is hormone replacement therapy, be it systemic, but more often local; these are probiotics; this is nonspecific prevention in the form of acidifying urine with cranberry preparations or, as we have always used cranberry juice since ancient times, and immunoactive prevention, which we will talk about today.
But if you notice, on this slide, after each statement, let's say, after each recommendation, there is a level of recommendation. Everything that concerns antibacterial drugs, then the level of recommendation is A, and as for probiotics and nonspecific prophylaxis, then, accordingly, the level of recommendation is C, and if we are talking about immunoactive prophylaxis, then we mean the level of recommendation B. What is this?
When we mean level A recommendation, we have the right to use these recommendations based on the results obtained from all kinds of large clinical trials, at least one of which must be randomized. If we talk about level B recommendation, then, of course, we use the knowledge that has been obtained as a result of studies, well-designed clinical trials, not necessarily randomized. If we are talking about level C, then clinical studies of the required quality have not been conducted on these drugs or in this area.
As for immunoprophylaxis, from this slide I can clearly say that this is how the song says, if we say immunoprophylaxis, we mean “Uro-Vaxom”; if we say “Uro-Vaxom”, then we mean form of immunoprophylaxis. Because today this is the only drug that is recommended, accordingly, indicated in the recommendations of the European Association of Urology. And you see the translation, accordingly, from the Guidelines, from these recommendations: “...Immunoactive prophylaxis and the effectiveness of Uro-Vaxom compared to placebo have been proven even in several randomized studies. And it can be recommended for immunoprophylaxis in women with uncomplicated recurrent urinary tract infections.”
The same thing, I specifically gave a link to our Russian national Recommendations for antimicrobial therapy and prevention. Treatment of recurrent infections with low doses of antibiotics. If we are talking about alternative methods of treatment and recurrent infections, then the schemes, accordingly, include the same “Uro-Vaxom”.
What is Uro-Vaxom? What he really is? Today these are capsules that contain lyophilized strains of Escherichia Coli, 18 strains. More than 2000 patients have undergone various studies. More than 1 million, respectively, have been treated over the past 5 years.
How does Uro-Vaxom work? Its action literally begins from the gastrointestinal tract. Once in the gastrointestinal tract, the cells of the immune system are stimulated, namely Peyer's patches, which make up 25% of the surface of the entire gastrointestinal tract. Previously, it was believed that such drugs could not act in the human body; let’s say, they were not absorbed. But it was realized that the action occurs precisely through Peyer’s patches. Activation of T- and B-lymphocytes occurs, that is, our T-lymphocyte is responsible for cellular immunity, and our B-lymphocytes, respectively, are responsible for humoral immunity. Circulation of protective cells - their entry into the bloodstream and lymphatic channel, respectively, integration of T- and B-lymphocytes into the urinary tract. And already the production of protective and specific antibodies in the mucous membrane of the bladder itself. In principle, probably 20 years ago, it was believed that through the mucous membrane we could not achieve such an effect of these drugs until it was discovered that immunoglobulin A can be produced through Peyer's patches - the same immunoglobulin A that works well in the mucous membrane. For example, in other organs or in the circulatory system, immunoglobulin G mainly acts, which in the mucous membrane, accordingly, works worse than immunoglobulin A.
If we are talking about strengthening antimicrobial protection in the genitourinary tract under the influence of "Uro-Vaxom", then it goes in two directions - this is the implementation, respectively, of a specific immune response and an increase in nonspecific resistance, that is, through macrophages, NK-phagocytosis, synthesis immunoglobulins A, as I already said.
It is believed that the amount of immunoglobulins A and immunoglobulins G in those patients who take Uro-Vaxom is almost 2-2.5 times higher than in those patients who do not take this immunoactive drug, Uro-Vaxom.
Moreover, it was previously believed that if this drug contains only lyophilisates of Escherichia Coli, then it should act accordingly in patients whose urine cultures revealed Escherichia Coli. No, in fact, studies have been performed on the basis of which we can say that Uro-Vaxom provides protection against a wider range of pathogens that cause urinary tract infections, and not just against those used in its , let's say, composition.
How can we use Uro-Vaxom? Starting with treatment together with an antibiotic, for 10 days together with an antibiotic, 1 capsule per day, and then continue, respectively, one capsule per day for 3 months. That is, we use the drug, starting from the treatment stage, and then for 3 months in order to carry out, accordingly, immunoactive prophylaxis.
What do we expect from this immunoactive prophylaxis? Of course, a decrease in the level of bacteriuria. Of course, a decrease in symptoms. Reducing the need to use antibacterial drugs. And, of course, either an increase in the intervals between exacerbations, that is, an increase in the interval of relapse-free course, or a decrease, complete disappearance of relapses of the disease.
Look, if the drug is used together with an antibiotic, then after 3 months of treatment the level of bacteriuria is 3 times lower than, for example, among those patients who took only an antibiotic. Moreover, if we want and pursue the goal of reducing the need to use antibiotics, look, if we use Uro-Vaxom, that is, a drug for active immunotherapy, it reduces the duration of antibiotic use by 36%. In total, after 6 months of using it, the need to use antibiotics is reduced by even 67%. Moreover, the drug reduces the number of relapses by 36% in those patients in whom the level of bacteriuria was quite high and reached, respectively, 104 CFU/ml/
A very large number of patients get rid of urinary tract infections when using Uro-Vaxom. You see that 65% is quite high for such a disease. The difference in the number of patients with relapses was about 21% in favor of this drug. We have one for the use of active immunoprophylaxis. Therefore, in general, there is no advertising of the drug here. In this case, we are advertising the same immunoactive prophylaxis.
Moreover, since we are pursuing the most long-term need and the possibility of a long relapse-free period, then, you see, even after 12 months, that is, 1 year after stopping the drug, 55% of patients get rid of relapses of this disease.
A lot of research has been done on this matter. But Kurt Nabert, for urologists this is a fairly well-known name, in matters relating to urinary tract infections, he conducted a fairly large meta-analysis, collecting the results of many studies on this issue, and it was revealed that against the background of such active immunoprophylaxis, a decrease in the number recurrence of urinary tract infections is about 40%.
Moreover, using active immunoprophylaxis, we improve laboratory parameters. Leukocyturia decreases, as you can see, by almost 2 times, bacteriuria by 33%. The incidence of dysuria after 6 months decreases by more than 50%, that is, almost 2.5 times.
Moreover, the drug is quite well tolerated. So I collected data from various studies specifically. And you see that despite the fact that a lot is used there, all kinds of side effects are presented, the percentage of their occurrence is so low that, in general, we can safely recommend to patients, saying that this immunoprophylaxis is practically without side effects. In my practice, patients mostly complain about this feeling of nausea, some kind of slight nausea, and even then not always.
If we are talking, accordingly, about the clinical effectiveness of immunoactive prophylaxis using Uro-Vaxom, then, as a summary, the number of relapses is reduced; the frequency of bacteriuria, dysuria, leukocyturia decreases; and, accordingly, the need to use antibiotics is reduced; reliable protection from 3 to 12 months; and, as I already said, the drug is very well tolerated.
At the beginning of my speech, I said that asymptomatic bacteriuria occurs quite often in pregnant women. This is a very complex group of patients, to whom the approach can sometimes even be difficult, let’s say. We always consult with gynecologists on this issue. Despite the fact that the annotation for this drug, Uro-Vaxom, states that no clinical studies have been conducted on pregnant women, at the same time, animal studies have not revealed any negative effects during pregnancy, including including the development of the embryo, fetus, respectively, and postnatal development. If we talk about the lactation period, then such studies have not been conducted; accordingly, there is no data on this condition.
But we still have a question. Is it possible to use Uro-Vaxom in pregnant women? To date, several such studies have been carried out, and I will try to present the data. It is quite possible that, given such indicators, the annotation for this drug may someday include the possibility of using it in pregnant women.
Against the background of immunoactive prophylaxis, there is a significant decrease in urinary tract relapses, you see, a significant decrease in the frequency of dysuria - 87% at the starting point and 22.8%, which is almost 3.5 times. Moreover, there is a significant reduction in the need for antibiotic use. For pregnant women, this is a very important issue, because for a pregnant woman, antibiotics, even though some antibiotics can be used in certain trimesters of pregnancy, it is better to bypass them. And, naturally, the duration of the required course of antibiotic therapy is reduced by almost 40%.
Last slide. I always voice it and show it when I talk about lower urinary tract infections. Their treatment must be comprehensive. Today we spoke with Grigory Georgievich that no, no, these women are still coming back. Why? Because in addition to antibiotics, in addition to anti-inflammatory drugs, in my practice I always try to use drugs to improve the functions of the lower urinary tract. At one time, our clinic carried out work to study the functions of the lower urinary tract in patients suffering from chronic recurrent cystitis. Almost 50% of them have dysfunction of the urethra, the so-called instability of the urethra, causing this functional obstruction, which in itself is a provocateur of the development, casting, let’s say, of those bacteria that are located in the distal part of the urethra, maximum casting, which in should not be the norm. This is the same overactive bladder. We must identify and treat any dysfunctions using appropriate medications along with antibiotics and uroseptics. And, of course, the drug for systemic immunoprophylaxis, what we talked about today, the drug “Uro-Vakson”, is the only one we have today. Protection of the urothelium from recurrent infection. This may also be local therapy. Now there are drugs that improve the condition of the bladder mucosa. But perhaps this is the topic of some of our other meetings and speeches.
I thank you for your attention. And like Grigory Georgievich, I always try to tell you that in our clinic of the First Moscow Medical University. THEM. Sechenov, at the Research Institute of Uronephrology and Human Reproductive Health on Bolshaya Pirogovskaya we are always ready to meet you and help you. Welcome. Thank you.
Treatment at the VMT MI Clinic. N.I. Pirogov St. Petersburg State University
North-West Center for Pelviperineology (NWTCPP), founded in 2011 on the basis of the Department of Urology of the Clinic of High Medical Technologies named after. N.I. Pirogov St. Petersburg State University, specializes in modern low-traumatic methods of treating stress urinary incontinence (SUI), painful bladder syndrome (interstitial cystitis), overactive bladder (OAB), its leader is Doctor of Medical Sciences, urologist Dmitry Dmitrievich Shkarupa.
Today we have no doubt that the ability to adjust the sling is the cornerstone that was missing to build a clear and effective system for performing sling operations.
Every year, our Center performs more than 600 implantations of an adjustable sling, which has become the standard of care for SUI. The use of this approach made it possible to almost completely eliminate obstructive complications and increase the real (!) effectiveness of the operation to 90%, even in complicated patients.
We consider tracking long-term treatment results to be the most important element of our work. More than 80% of our patients are regularly examined by the Center’s specialists in the late postoperative period. This allows you to see a real picture of the effectiveness and safety of the treatment.
COST OF TREATMENT FOR URINARY INCONTINENCE:
Most patients receive care free of charge as part of compulsory health insurance (compulsory medical insurance).
It is also possible to pay for treatment in cash. The price depends on the volume and complexity of the operation. On average: from 60,000 to 80,000 rubles
(The price includes: surgery, anesthesia, hospital stay, mesh implant and other expenses).
Bibliography
- AskMayoExpert. Female urinary incontinence and voiding dysfunction (adult). Rochester, Minn.: Mayo Foundation for Medical Education and Research. 2021.
- What is urinary incontinence? Urology Care Foundation. https://www.urologyhealth.org/urologic-conditions/urinary-incontinence. Accessed March 18, 2021.
- McAninch JW, et al., eds. Urinary incontinence. In: Smith and Tanagho's General Urology. 18th ed. New York, NY: McGraw-Hill; 2013. https://accessmedicine.mhmedical.com/content.aspx?bookid=508§ionid=41088107. Accessed March 18, 2021.
- South-Paul JE, et al. Urinary incontinence. In: Current Diagnosis & Treatment in Family Medicine. 4th ed. New York, NY: The McGraw-Hill Companies; 2015. https://accessmedicine.mhmedical.com. Accessed March 18, 2021.
- Lukacz ES. Evaluation of women with urinary incontinence https://www.uptodate.com/home. Accessed March 18, 2017.
- Bladder control problems in women (urinary incontinence). National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/urologic-diseases/bladder-control-problems-women. Accessed March 18, 2021.
- AskMayoExpert. Male urinary incontinence. Rochester, Minn.: Mayo Foundation for Medical Education and Research. 2021.
- Bladder control problems in men (urinary incontinence). National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/urologic-diseases/bladder-control-problems-men. Accessed March 18, 2021.
- Gameiro SF, et al. Electrical stimulation with non-implanted electrodes for overactive bladder in adults. Cochrane Database of Systematic Reviews. https://onlinelibrary.wiley.com/doi/10.1002/14651858.CD010098.pub4/full. Accessed March 18, 2021.
- Jelovsek JE. Surgical management of stress urinary incontinence in women: Choosing a primary surgical procedure. https://www.uptodate.com/home. Accessed March 18, 2021.
- Frawley J, et al. Complementary and conventional health-care utilization among young Australian women with urinary incontinence. Urology. 2017;99:92.
- Mo Q, et al. Acupuncture for adults with overactive bladder: A systematic review protocol. BMJ Open. 2015;5:1.
- Solberg M. A pilot study on the use of acupuncture or pelvic floor muscle training for mixed urinary incontinence. Acupuncture Medicine. 2016;34:7.
- Vinchurkar AS, et al. Integrating yoga therapy in the management of urinary incontinence: A case report. Journal of Evidence-Based Complementary & Alternative Medicine. 2015;20:154.
- Brown A.Y. Allscripts EPSi. Mayo Clinic, Rochester, Minn. Jan. 24, 2021.
- Ziegelmann MJ, et al. The impact of prior urethral sling on artificial urinary sphincter outcomes. Canadian Urological Association Journal. 2016;10:405.
- Linder BJ, et al. Autologous transobturator urethral sling placement for female stress urinary incontinence: Short-term outcomes. Urology. 2016;93:55.
- Lukacz ES. Treatment of urinary incontinence in women. https://www.uptodate.com/home. Accessed May 9, 2021.
- American College of Obstetricians and Gynecologists (ACOG) Committee on Practice Bulletins - Gynecology and the American Urogynecologic Society. ACOG Practice Bulletin No. 155: Urinary Incontinence in Women. Obstetrics & Gynecology. 2015;126:e66.
The role of Uro-vaxom in the complex treatment of patients with chronic pyelonephritis and cystitis
AND
Infectious and inflammatory diseases of the genitourinary system occupy an important place in the structure of urological pathology, especially among women.
80–90% of all patients with chronic pyelonephritis and cystitis are women; 10–20% of women experience an episode of urinary tract infection at least once during adulthood [8,14]. Despite the huge number of powerful antibiotics, the problem of treating patients with urinary infections is far from being resolved. First of all, we see the reason for this as the lack of an integrated approach. The doctor discovered bacteriuria and leukocyturia in the patient; coupled with complaints of pain in the kidney area, frequent painful urination, rise in body temperature, etc. this is certainly an indication for treatment. What goal does the doctor set for himself in such a situation? Achieve eradication of the pathogen and, indirectly, stop inflammation. And the achievement of this goal, judging by domestic and foreign publications, is expected by prescribing antimicrobial drugs. Is it possible to destroy a microbial agent with antibacterial therapy in the case of uncomplicated acute or exacerbation of chronic nonspecific pyelonephritis or cystitis? Yes, in the vast majority of cases. Can we talk about the patient’s recovery? Not always. Of course, in a situation of acute cystitis, provoked by some obvious single action, taking fosfomycin can stop dysuria and sanitize the urine within 24 hours. It is likely that in the absence of repeated provocation the patient will never develop cystitis again. In this case, recovery occurred as a result of taking an antibiotic. Unfortunately, circumstances usually turn out differently. Much more often, a patient comes to the appointment who has received many courses of antibacterial therapy, both for genitourinary tract infections and for concomitant diseases. What decision will the average doctor make? Prescribe a stronger antibiotic at the maximum dosage. Will he achieve the destruction of the pathogen? Very likely, yes. Will he cure the patient with this? Most likely not. The patient we talked about above was treated with antibiotics for a long time. It can be said with 100% certainty that she has intestinal and vaginal dysbiosis and a disturbed immune response. There is a high probability of presence in the urine, in addition to microbial flora, also of fungi. The long course of the infectious-inflammatory process in such unfavorable conditions actually transforms an uncomplicated urinary tract infection into a complicated one
, as it promotes the selection of resistant pathogens and disrupts the natural passage of urine.
Thus, the use of antibacterial therapy alone is not enough; a complex pathogenetic effect
.
Pathogenetic measures should include laser therapy (with strict consideration of contraindications), infusion, antioxidant, and anti-inflammatory therapy. In addition, you should use the drug Uro-vaxom
, which is actually a means of etiopathogenetic treatment of urinary infections.
Uro-vaxom is a 6 mg lyophilized bacterial lysate of 18 different strains of E. Coli
, enclosed in a gelatin capsule for daily administration on an empty stomach once a day.
Since E. Coli
is the main causative agent of both complicated and uncomplicated urinary infections [2,3], the targeting of Uro-Vaxom can be regarded as an etiotropic effect.
However, the inhibitory effect of Uro-vaxom on both S. aureus
and
C. albicans
[7].
According to the mechanism of action, Uro-vaxom is an immunomodulator; Experimental studies have established its activating effect on lymphocytes and macrophages. Uro-vaxom increases both humoral and cellular immune responses, thereby enhancing natural defenses against microbial agents. Uro-vaxom is initially prescribed in combination with antimicrobial therapy; the main goal is to reduce the frequency and severity of relapses and exacerbations. In the future, it is possible to carry out preventive courses of Uro-Vaxom. Unusually important results were obtained by Bottex et al. [5], who found that Uro-vaxom significantly reduces immunosuppression caused by antibiotics
.
Foreign experience shows the feasibility of using Uro-vaxom in clinical practice. Schulman et al. [13] assessed the effectiveness of Uro-Vaxom on the example of 160 patients with urinary tract infections. 82 of them received Uro-Vaxom (mean age 45.3±2.0 years, 84% women) and 78 received placebo (age 45.0±1.8 years, 83% women). Patients received Uro-vaxom 6 mg or placebo once a day for 3 months; Then they were monitored for another 3 months. Bacteriuria was recorded significantly less frequently in the Uro-Vaxoma group than in the control: 31 versus 59 during treatment (p<0.001) and 27 versus 55 during the observation period (p<0.001). In the Uro-Vaxom group, 0.7 cases of relapse were noted over 6 months, while in the control this occurred 2 times more often. Accordingly, patients in the Uro-Vaxom group took antibiotics significantly less. The authors emphasize the long-term aftereffect in the main group. Side effects in the form of minor skin manifestations were noted in 2 patients receiving Uro-Vaxom and in 11 patients receiving placebo. Magasi et al. [10], who conducted a study using the same design with 112 patients, obtained similar data: in patients treated with Uro-Vaxom, exacerbation was observed in 13.8% of cases within six months, while among those taking placebo - in 79.6 %. These authors did not record any adverse reactions at all. The effectiveness of Uro-Vaxom was studied on the example of 64 patients with spinal trauma (67% of them were men). All of them underwent regular or continuous bladder catheterization; All of them had an increased number of leukocytes in their urine. In most patients, growth of E. Coli
;
in isolated cases – growth of Proteus spp., Klebsiella spp;
S. aureus .
Patients were given a three-month course of antibacterial therapy followed by Uro-Vaxom or placebo (also for 3 months). In both groups, while taking antibiotics, a significant improvement was obtained, which persisted in patients receiving Uro-Vaxom, but returned to the original level in the placebo group. Minor side effects were noted by 6 and 5 patients, respectively [6]. The long-term aftereffect of Uro-Vaxom was noted by Tammen et al. [15]. In addition to the standard regimen (3 months of Uro-Vaxom, 3 months of observation), the authors continued to monitor the patients’ condition for another 5 months. The main group included 61 patients (85% women), and the control group receiving placebo included 59 patients (86% of them women). Over the course of six months, patients in the control group had an average of 1.8 exacerbations of urinary tract infections, while in the main group this figure was only 0.82 (p <0.05). Although antibiotic therapy in the first 3 weeks of the study was similar in both groups, subsequently the need for repeated courses of antibiotics in the main group was significantly lower. Clinical manifestations of urinary infections
(pyuria, bacteriuria, dysuria)
stopped faster when taking Uro-Vaxom
.
Overall, the effectiveness of complex treatment in the main group was 95.1%, while in the control group it was only 72.9%. The positive effect persisted throughout the observation period in 95.1% of patients receiving Uro-Vaxom and in 60.3% of patients in the placebo group. A method of fractional therapy is also described (the first 10 days of each month for three months in a row). Thus, Schneider [12] prescribed Uro-Vax to 116 women (average age 35.6 years) suffering from uncomplicated cystitis. About a quarter of the patients were included in the study during the period of remission. Treatment was carried out for 10 days every month for six months. Previously, these patients annually noted an average of 3.4 exacerbations of cystitis; against the background of intermittent use of Uro-Vaxom, their number decreased to 1.2. This treatment regimen was also well tolerated by patients, the severity and frequency of side effects were insignificant. The feasibility of maintenance therapy with a booster dose of Uro-Vaxom in postmenopausal women has been proven. Uro-vax was prescribed to 58 women (average age 66.3 years), who had an average of 3.4 exacerbations of chronic cystitis annually. The treatment regimen was as follows: for 3 months, patients took Uro-Vaxom, 1 capsule daily, followed by a three-month break, then for another 3 months, patients received Uro-Vaxom 10 days a month. In just 9 months of observation, the relapse rate decreased by 64.7%, averaging 1.8. A slight heaviness in the stomach after taking the drug was noted in one patient; no other complications of treatment were recorded [11]. There is another aspect to the problem of treating urinary infections. In the Ural, Siberian and Far Eastern federal districts (74% of the territory of Russia), a tuberculosis epidemic persists, that is, the incidence of the population exceeds 100 per 100,000 [4]. In these conditions, recommendations for the treatment of infections of the genitourinary system, created for safe conditions, cannot be fully applied, since there is a risk of reducing the inoculation of Mycobacterium tuberculosis (MBT) and, consequently, late diagnosis of urotuberculosis, and the frequency of drug resistance of MTB increases. In a tuberculosis epidemic zone, treatment of supposedly nonspecific infections should begin with drugs that obviously do not have an inhibitory effect on Mycobacterium tuberculosis: Amoxicillin/clavulonic acid
is a broad-spectrum antibiotic that has a bactericidal effect, including against strains resistant to amoxicillin.
Gentamicin
is a broad-spectrum aminoglycoside.
Bactericidal, penetrates the cell membrane. Fosfomycin trometamol
is a broad-spectrum antibiotic that is active against most gram-u1086 negative and gram-positive bacteria.
After a single oral dose of fosfomycin trometamol, a concentration is created in the urine after 3 hours that is significantly higher than the minimum inhibitory concentration for the main uropathogenic strains of bacteria, and persists for 72–80 hours. Currently, the lowest microflora resistance has been registered to fosfomycin trometamol [9]. Ceftriaxone
is a third generation cephalosporin antibiotic that has a bactericidal effect.
Highly resistant to action? –lactamase. Effective against aerobic gram-positive and gram-negative microorganisms, including those resistant to penicillins and other cephalosporins. Excreted by the kidneys (60%) and through the intestines. Bactericidal concentrations persist for 24 hours. Nitrofurantoin
is an antimicrobial drug from the group of nitrofuran derivatives;
Available in the form of enteric-coated tablets. It has a bacteriostatic and bactericidal effect on gram-positive and gram-negative microorganisms, including those resistant to antibiotics and sulfonamides. Pyobacteriophage (sextaphage)
is a sterile mixture of purified filtrates of phagolysates of bacteria staphylococci, streptococci, Proteus, Pseudomonas aeruginosa, Klebsiella pneumoniae, Escherichia coli;
is available ready-to-drink in the form of a transparent yellow liquid of varying degrees of intensity with a greenish tint. Uro-vaxom
should be considered as a drug that enhances the effectiveness of antibacterial therapy, and in some cases replaces it .
The therapeutic effect of Uro-Vaxom is due to stimulation of T-cell immunity, increased production of endogenous interferon and the creation of high levels of IgA in the urine [15]. Prescribed on an empty stomach, 1 capsule per day for 10 days for acute cystitis and up to 3 months for chronic urinary tract infections. Considering that the main causative agent of infectious and inflammatory diseases of the urinary tract is E. Coli
, the use of a specifically targeted drug that is not an antibiotic is very promising.
It is obvious that treatment with Uro-Vaxom will in no way affect the frequency of detection of MBT and will not cause the development of its resistance, therefore Uro-Vaxom is absolutely indicated for patients receiving ex juvantibus type 1 therapy [1]. The drugs listed above have a bactericidal effect on the main types of nonspecific microorganisms, without at the same time inhibiting the growth of Mycobacterium tuberculosis and, therefore, do not have a negative effect on bacteriological diagnostics. After performing 2-3 urine cultures for MBT, if there is no effect, fluoroquinolones (for example, norfloxacin or ciprofloxacin) can be prescribed. We used Uro-Vaxom in the complex treatment of 18 patients with recurrent infections of the genitourinary system. 15 had chronic nonspecific pyelonephritis, 2 had chronic cystitis and 1 had chronic urethritis supported by capitate urethral hypospadias. In 16 cases the causative agent was E. Coli
, in 1 –
Enterobacter
, in another patient –
S. aureus
.
Uro-vaxom was prescribed for a course of 3 months immediately after completion of antibacterial therapy. In no case were any adverse reactions to Uro-Vaxom noted. Patients came for a follow-up appointment, which included a general urine test, 2 times a month. The total observation period is 6 months. All patients achieved a stable effect, expressed in the absence of clinical manifestations of urinary tract infections, urine sanitization, and cessation of bacteriuria. None of the patients experienced an exacerbation of the disease. Thus, Uro-vaxom
should be considered as
a promising drug with etiopathogenetic action
for the treatment of urinary tract infections, which should be included in a complex therapy regimen. It is necessary to conduct a series of studies to determine the possibility of using Uro-Vaxom in the treatment of various categories of patients, including children, and, probably, expanding the indications.
Literature 1. Kulchavenya E.V. Difficulties in diagnosing tuberculosis of the genitourinary system. – Novosibirsk, 2004. 2. Rafalsky V.V., Strachunsky L.S., Krechikova O.I. et al. Resistance of pathogens of outpatient urinary tract infections according to multicenter microbiological studies UTIAP-I and UTIAP-II.//Urology.–2004.–No. 2.– P. 14–17. 3. Rafalsky V.V., Strachunsky L.S., Kogan M.I. et al. Antibacterial therapy of complicated urinary tract infections in outpatients.//Urology. – 2004. – No. 5. – P. 25–29. 4. The state of anti-tuberculosis care to the population of the Siberian and Far Eastern federal districts based on the results of work in 2003 / ed. Krasnova V.A. – Novosibirsk, 2004. 5. Bottex C., Martin A., Fontangens R. Action of a mycotoxin on the immune response of the mouse – interaction with an immunomodulator. Immunopharm Immunotoxic 1990; 12: 311–325. 6. Hachen HJ Oral immunotherapy in paraplegic patients with chronic urinary tract infections: a double-blind, placebo-controlled trial. // J. Urol., 1990; 143:759–763. 7. Hockertz St. Immunomodulatory effects of immunoactive fractions of selected E.Coli strains on the macrophage. Arzneim Forsch Drug Res. 1990; 40: 1068–1072/ 8. Johnson JR, Stamm WE. Urinary tract infections in women: diagnosis and treatment. Ann Intern Med 1989; 111:906–917. 9. Kahlmeter G., Journal of Antimicrobial Chemotherapy (2000) 46 Suppl., S1 – 15 –22 (cited from the journal “Medical Estate”, 2004. – No. 3. – pp. 32–36. 10. Magasi P, Panovics J, Illes A, Nagy M. Uro–Vaxom and the management of recurrent urinary tract infection in adults: a randomizes multicenter double–blind trial. Europ Urol 1994;26:137–140. 11. Popa G, Lauber K–D , Rothe H, Rugendorff E. Rezidivierende Harnwegsinfektionen in der Postmenopause. Wirksamkeit einer oralen Immuntherapie mit E. Coli-fraktionen. Munch med Wschr 1996; 138: 713–716. 12. Schneider H–J. New therapeutic approach for recurrent urinary tract infections Marked reduction in recurrence rate in women with uncomplicated cystitis – few side effects, high compliance. Der Allgemeinarzt 1990;12:626–633. 13. Schulman CC, Corbusier A, Michiels H, Taenzer HJ. Oral immunotherapy of recurrent urinary tract infections : a double-blind placebo-controlled multicenter study J Urol 1993;150:917–921 14. Schultz HJ, McCaffrey LA, Keys TF, Nobrega FT. Acute cystitis: a prospective study of laboratory tests and duration of therapy. Mayo Clin Proc 1984; 59: 391–397. 15. Tammen H. and the German urinary tract infection study group. Immunobiotherapy with Uro-Vaxom in recurrent urinary tract infection. //Br J Urol 1990; 65:6–9.