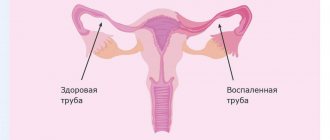
One of the most common diseases of the upper parts of the female reproductive system is adnexitis. It is an inflammatory process in which the uterine appendages are involved. If the disease has spread to both sides, then doctors diagnose bilateral adnexitis. If treated incorrectly or untimely, inflammation can lead to severe purulent-septic lesions or infertility. Therefore, it is very important to immediately undergo a comprehensive examination and begin treatment when the first symptoms occur.
Local symptoms of inflammation of the appendages:
- Aching, cutting pain of medium duration in the abdominal area;
- Painful periods, dull pain during intimacy;
- Mucous or purulent leucorrhoea, clear discharge, often accompanied by itching and irritation on the skin;
- Changes in the timing, duration of menstruation, cycle shift.
If you note at least one symptom, contact GMS Clinic specialists for diagnosis. It is much easier to cure the disease in the early stages, and the likelihood of avoiding complications and consequences is higher.
Signs of right-sided adnexitis
Signs that indicate damage to the fallopian tubes and ovaries:
- Severe pain in the abdominal area. As a rule, the right side hurts and women often confuse this with a manifestation of appendicitis.
- Temperature rises to 39 degrees.
- The appearance of purulent vaginal discharge.
- Problems with bowel movements.
- Pain when urinating.
A change in the amount of discharge during menstruation, an increase or decrease in the interval, the appearance of pain, indicates serious health problems. If such a symptom appears, it is best to contact the specialists of the Healthy Family clinic. Doctors will conduct a diagnosis and determine the exact cause of the problem. As a rule, with inflammatory diseases, especially if bilateral adnexitis is chronic, female sex hormones begin to be produced in minimal volumes, which affects menstruation. They can be either too scanty or abundant, and in some cases even the appearance of clots and fragments of the endometrium is observed.
The presence of an inflammatory process in the appendages provokes the appearance of purulent discharge. They appear during urination, as well as involuntarily. In some cases, it is greenish or yellow mucus. Due to the appearance of uncharacteristic discharge, the vaginal walls become irritated, which leads to severe itching and burning. Experienced specialists at the Healthy Family clinic can make a preliminary diagnosis and identify the pathogen based on the color of the discharge. Thus, under the influence of gonorrhea, clots of a yellowish tint appear, and with trichomoniasis, green-yellow clots appear.
Adnexitis is characterized by frequent bleeding, which can lead to the development of anemia. This makes a woman feel weak and depressed. The appearance of prolonged bleeding indicates that the disease is becoming chronic.
Additionally, women experience symptoms of general intoxication of the body:
- weakness;
- severe headaches;
- decreased appetite.
With a long course of the disease, health deteriorates significantly. Severe inflammation can cause problems with consciousness or disability. As a rule, this occurs due to the pain radiating to the spine.
If the disease progresses and peritonitis develops, the abdominal muscles become very tense, the pain spreads to the entire peritoneal area, and the woman’s condition worsens.
Subacute bilateral adnexitis is characterized by less striking clinical manifestations. The disease develops gradually. The pain is not so pronounced, and the temperature does not rise much. This progression of adnexitis leads to many women delaying treatment, and the disease becomes chronic.
Prolonged course without proper treatment leads to the fact that the inflammatory process spreads not only to the tubes, but also to the uterus. This form of the disease has its own name, salpingoophoritis. Its chronicity has a strong impact on the female body. The following functions are affected:
- menstrual;
- sexual;
- reproductive.
Often, problems with ovulation in combination with obstruction of the fallopian tubes lead to the development of infertility or the occurrence of an ectopic pregnancy. This is due to hormonal instability and the impossibility of normal functioning of internal organs. Even if fertilization proceeds normally and the egg is implanted into the wall of the uterus, then with adnexitis there is still a high probability of miscarriage or miscarriage.
A long-term inflammatory process in the body causes damage to the nervous and endocrine systems. A decrease in the body's protective functions, combined with constant mood swings caused by unstable hormonal levels, provokes the development of depression.
General symptoms of inflammation of the appendages:
- Pain in the lower abdomen, accompanied by general malaise, fever and weakness;
- Dry mouth, nausea, headaches;
- Changes in the blood picture: increased ESR, leukocytosis.
- Tachycardia is a strong heartbeat, accompanied by dizziness and ringing in the ears.
General symptoms of inflammation can relate not only to problems in the female genital area, but also to any other inflammatory processes occurring in the body. If any general symptom is detected in combination with local symptoms, you should immediately consult a doctor. We advise you to make an appointment with GMS Clinic specialists to receive qualified advice and assistance.
Classification of adnexitis
The inflammatory process can be acute or chronic5.
The chronic form often occurs after untreated acute adnexitis, in which the pathogen remains in the body, and when immunity decreases, the symptoms return. In chronic cases, symptoms may be less pronounced or completely absent. In this case, it is very important not to miss the infection and consult a doctor in a timely manner, because the disease can lead to the formation of adhesions in the pelvis, obstruction of the fallopian tubes, chronic pelvic pain, infertility and ectopic pregnancy1.
Up to contents
Forms of the disease. Symptoms characteristic of each form
Inflammation of the appendages can occur in several forms. To be fully prepared and know when to start sounding the alarm, we will tell you the most common symptoms of various forms of inflammation of the appendages.
- Contrary to expectations, the latent, or hidden, form of inflammation of the appendages is considered the most dangerous. Most often, women do not notice the symptoms of the inflammatory process occurring in the body, or attribute everything to stress and fatigue (headache, dizziness, abdominal pain). The latent form is dangerous because it is often detected already in the last stages, when adhesions have formed and the inflammatory process develops irreversibly. That is why we advise all women, even those who have no health complaints, to visit a gynecologist quarterly.
- The acute form is detected very easily, the characteristic symptoms are: cycle disruption, heavy discharge in the form of leucorrhoea, increased temperature, nagging pain in the lower abdomen, radiating to the lower back. If these symptoms are detected, you should immediately contact a specialist to prescribe treatment.
- The chronic form of inflammation of the appendages most often develops from an untreated acute or latent form. A typical symptom of the chronic form is a constant temperature of about 37 degrees, lethargy, dizziness, periodic pain in the lower abdomen, and discharge.
Symptoms and signs of adnexitis
It is important to distinguish the symptoms of adnexitis in women from signs of other diseases of the ovaries and uterus. In particular, salpingo-oophoritis is characterized by the following symptoms:
- Increase in body temperature to 39⁰.
- Spasmodic pain is felt in the abdomen, radiating to the sacrum and lumbar region of the back.
- A condition similar to an attack of appendicitis.
- Irregularities in the menstrual cycle - bleeding is irregular, heavy or too scanty, accompanied by severe pain.
- During urination, a woman feels pain and purulent discharge is noticeable.
- Sexual intercourse is accompanied by pain and severe discomfort; these sensations persist for several hours after the act.
Cost of treating adnexitis
The prices indicated in the price list may differ from the actual prices. Please check the current cost by calling +7 495 104 8605 (24 hours a day) or at the GMS Hospital clinic at the address: Moscow, st. Kalanchevskaya, 45.
| Name | Price |
| Initial consultation with a leading gynecologist | RUB 6,951 |
| Initial appointment with a gynecologist | RUB 4,865 |
| Repeated consultation with the leading gynecologist | RUB 5,908 |
| Repeated appointment with the gynecologist | RUB 4,137 |
Dear Clients! Each case is individual and the final cost of your treatment can only be found out after an in-person visit to a GMS Hospital doctor. Prices for the most popular services are indicated with a 30% discount, which is valid when paying in cash or by credit card. You can be served under a VHI policy, pay separately for each visit, sign an agreement for an annual medical program, or make a deposit and receive services at a discount. On weekends and holidays, the clinic reserves the right to charge additional payments according to the current price list. Services are provided on the basis of a concluded contract.
Plastic cards MasterCard, VISA, Maestro, MIR are accepted for payment. Contactless payment with Apple Pay, Google Pay and Android Pay cards is also available.
Western standards of treatment (evidence-based medicine)
Continuous staff development
Regular interaction with leading Russian and foreign medical institutions
Modern medical equipment and advanced diagnostic and treatment methods
Unified standard of service
We work around the clock 24/7/365
Make an appointment We will be happy to answer any questions Coordinator Oksana
The International Statistical Classification of Diseases and Problems, 10th revision (ICD-10), currently in use, is a normative document that ensures the formation of unified statistical control over the activities of medical institutions, assessment of the epidemiological situation in the country, and allows for the unity and comparability of incoming medical data [1] . ICD-10 is one of the important methodological tools for processing statistical data, which is extremely necessary for automating basic planning, regulatory and management work [2]. Unfortunately, this classification contains errors, both in the structural design of clinical sections and in the coding of a number of diseases. Some of the diagnoses that exist in it sound somewhat absurd; there is a confusion of placement of individual polyetiological diseases and syndromes in sections, which are often located in chapters that have a very indirect relationship to this nosology. In addition, many nosological forms, syndromes and symptoms that are currently common are not included in the accepted classification, which undoubtedly significantly limits the practical application of ICD-10.
The variety of different forms of diseases complicates the structure of the classification, so the latest revision has become much larger in volume and was accompanied by extensive guidelines, unfortunately, often without taking into account clinical practice. As a result, some of the clinical diagnoses ended up within the limits of unrefined conditions or conditions that were not sufficiently differentiated, and not in the headings or subheadings of the corresponding sections of the classification.
A number of difficulties arise with regard to the topographic classifications and terms used in ICD-10, many of which are imprecise, contradictory and do not correspond to clinical practice. Unfortunately, it should be noted that ICD-10 cannot currently be recommended as a model for terminology and recording of clinical diagnoses in medical records and other medical records.
To solve the problem of uniform standardization of medical diagnoses and statistical records, back in the late 70s of the last century, the idea arose of creating a “family” of classifications of diseases and health problems based on the ICD, adapted to a specific specialty, taking into account modern achievements of medical science.
Classification options for dentists, oncologists, dermatologists, rheumatologists and orthopedists, pediatricians, psychiatrists, and general practitioners have been published and recommended by WHO. Unfortunately, in the field of andrology there is still no unified classification [2].
Currently, the Research Institute of Urology is developing printed and electronic versions of a similar classification for urology and andrology, which is based on three-digit and four-digit ICD-10 codes. The coding system for urological and andrological diseases is presented in the form of a tree, where each subnode refines the information of the previous node. When forming a subnode, a number from zero to nine is added to the main code through a dot. The proposed system also provides for taking into account the localization of the pathological process, its stage and/or phase [3-5].
The creation of a printed and electronic version of a new unified clinical and statistical classification of andrological diseases will allow:
- facilitate data collection and improve the analysis of statistical material on andrology by increasing the reliability of statistical information and reducing the number of errors due to inconsistency of clinical diagnoses with ICD-10 diagnoses;
- provide a detailed assessment of the complexity of clinical cases and final treatment results when providing specialized (including high-tech) medical care;
- standardize the formulation of andrological diagnoses in medical documents and computer information systems of health authorities of the Russian Federation;
- improve the economic and statistical analysis of the provision of medical care in the field of andrology in the interests of healthcare of the Russian Federation, individual medical institutions and compulsory health insurance (CHI);
- optimize costs for diagnosis and treatment of andrological diseases.
It should be taken into account that andrological diseases, as a rule, are multi-etiological and many of them do not fit only into the framework of the block “Diseases of the male genital organs”. The modern concept of andrology is, of course, based on interdisciplinary interaction and is at the intersection of related medical disciplines (urology, endocrinology, psychiatry, genetics, neurology, therapy, etc.). Therefore, andrological diseases are heterogeneous in nature and are widely represented in different sections of ICD-10 (Table 1).
Table 1. General classification of andrological diseases according to ICD-10 and proposals for its correction
| ICD-10 code | Nosology | Correction and comments |
| 1 | 2 | 3 |
| A54.0 | Gonococcal infection of the lower genitourinary tract without abscessation of the periurethral or accessory glands | |
| A54.1 | Gonococcal infection of the lower genitourinary tract with abscess formation of the periurethral and accessory glands | |
| A56 | Other chlamydial sexually transmitted diseases | |
| A56.0 | Chlamydial infections of the lower genitourinary tract | |
| A56.1 | Chlamydial infections of the pelvic organs and other genitourinary organs | |
| A56.2 | Chlamydial infection of the genitourinary tract, unspecified | |
| A56.8 | Chlamydial infections, sexually transmitted infections, other localization | |
| A59 | Trichomoniasis | |
| A59.0 | Urogenital trichomoniasis | |
| A60 | Anogenital herpetic viral infection (herpes simplex) | |
| A60.0 | Herpetic infections of the genitals and genitourinary tract | |
| D17.6 | Benign neoplasm of adipose tissue of the spermatic cord | |
| E28.0 | Excess estrogen | Controversial diagnosis. It has no clinical use in men. |
| E28.1 | Excess androgens | Controversial diagnosis. Not all specialists accept the upper limits of normal. |
| E29 | Testicular dysfunction | Controversial diagnosis. Has no clinical use. |
| E29.0 | Testicular hyperfunction | Controversial diagnosis. Has no clinical use. |
| E29.1 | Testicular hypofunction | Controversial diagnosis. Has no clinical use. |
| E29.8 | Other types of testicular dysfunction | Controversial diagnosis. Has no clinical use. |
| E29.9 | Testicular dysfunction, unspecified | Controversial diagnosis. Has no clinical use. |
| E89.5 | Testicular hypofunction after medical procedures | Controversial diagnosis. Has no clinical use. |
| F52 | Sexual dysfunction not due to organic disorders or diseases | We propose to reduce this diagnosis due to its uncertainty, and refer all cases of erectile dysfunction to paragraph N48.4. |
| F52.0 | Lack or loss of sexual desire | |
| F52.1 | Aversion to sexual intercourse and lack of sexual pleasure | |
| F52.2 | Lack of genital response | Controversial diagnosis. It has no clinical use in men. |
| F52.3 | Orgasmic dysfunction | |
| F52.4 | Premature ejaculation | Correction: F52.4: Ejaculation disorders |
| Correction: F52.4.0 Premature ejaculation. | ||
| Correction: F52.4.1 Delayed ejaculation. | ||
| Correction: F52.4.2 Retrograde ejaculation. | ||
| Correction: F52.4.3 Anejaculation. | ||
| F64.0 | Transsexualism | |
| F64.2 | Gender identity disorder in childhood | |
| F64.8 | Other gender identity disorder | |
| F64.9 | Gender identity disorder, unspecified | |
| F65 | Sexual preference disorders | |
| F65.6 | Multiple disorders of sexual preference | |
| F65.8 | Other disorders of sexual preference | |
| F65.9 | Disorder of sexual preference, unspecified | |
| F66 | Psychological and behavioral disorders associated with sexual development and orientation | |
| F66.0 | Sexual maturation disorder | |
| F66.1 | Egodystonic sexual orientation | |
| F66.2 | Sexual relationship disorder | Controversial diagnosis. Correction: sexual disharmony. |
| F66.8 | Other psychosexual developmental disorders | |
| F66.9 | Psychosexual development disorder, unspecified | |
| F68.0 | Exaggeration of somatic symptoms for psychological reasons | |
| F83 | Mixed specific psychological development disorders | |
| F84 | General psychological disorders | |
| I86.1 | Varicose veins of the scrotum (varicocele) | |
| Correction: I86.1.0 Varicocele on the left. | ||
| Correction: I86.1.1 Varicocele on the right. | ||
| Correction: I86.1.2 Varicocele hemodynamic type 1 (renotesticular type of reflux). | ||
| Correction: I86.1.3 Varicocele hemodynamic type 2 (ileotesticular type of reflux). | ||
| Correction: I86.1.4 Varicocele hemodynamic type 3 (mixed type of reflux). | ||
| Correction: I86.1.5 Bilateral varicocele. | ||
| N34.0 | Urethral abscess | |
| N34.1 | Nonspecific urethritis | |
| N34.2 | Other urethritis | |
| N35 | Urethral stricture | |
| N35.0 | Post-traumatic urethral stricture | |
| N35.1 | Post-infectious urethral stricture, not elsewhere classified | |
| N35.8 | Other urethral stricture | |
| N35.9 | Urethral stricture, unspecified | |
| N36 | Other urethral diseases | |
| N36.0 | Urethral fistula | |
| N36.1 | Urethral diverticulum | |
| Correction: N36.2 Stenosis of the external urethral meatus. | ||
| Correction: N36.3 Obliteration of the urethra. | ||
| N36.8 | Other specified diseases of the urethra | |
| N36.9 | Urethral disease, unspecified | |
| N37* | Lesions of the urethra in diseases classified elsewhere | |
| N37.0* | Urethritis in diseases classified elsewhere | |
| N37.8* | Other lesions of the urethra in diseases classified elsewhere | |
| N39 | Other diseases of the urinary system | |
| N39.0 | Urinary tract infection without established localization | |
| N39.3 | Involuntary urination | |
| N39.4 | Other specified types of urinary incontinence | |
| N39.8 | Other specified diseases of the urinary system | |
| N39.9 | Urinary system disorder, unspecified | |
| N40 | Benign prostatic hyperplasia | |
| Correction: N40.0 With impaired quality of urination. | ||
| Correction: N40.1 Without affecting the quality of urination. | ||
| N41.0 | Acute prostatitis | |
| N41.1 | Chronic prostatitis | |
| Correction: N41.1.0 Chronic bacterial prostatitis. | ||
| Correction: N41.1.1 Chronic abacterial prostatitis. | ||
| Correction: N41.1.1.1 Abacterial CP with the presence of inflammation. | ||
| Correction: N41.1.1.2 Abacterial CP without signs of inflammation. | ||
| Correction: N41.1.2 Asymptomatic chronic prostatitis. | ||
| N41.2 | Prostate abscess | |
| N41.3 | Prostatocystitis | Controversial diagnosis. Has no clinical use. We propose to reduce this diagnosis. Correction: N41.3 Colliculitis. |
| Correction: N41.4 Sclerosis of the prostate gland. | ||
| N41.8 | Other inflammatory diseases of the prostate gland and seminal vesicles | |
| N41.9 | Inflammatory disease of the prostate, unspecified | |
| N42 | Other prostate diseases | |
| N42.0 | Prostate stones | Controversial diagnosis. Has no clinical use. We propose to reduce this diagnosis. Correction: Simple prostate cyst. |
| N42.1 | Congestion and hemorrhage in the prostate gland | Controversial diagnosis. Has no clinical use. We propose to reduce this diagnosis. |
| N42.2 | Prostate atrophy | |
| N42.8 | Other specified prostate diseases | |
| N42.9 | Prostate disease, unspecified | |
| N43 | Hydrocele and spermatocele | We propose in paragraph N43 to consider only hydrocele. |
| N43.0 | Hydrocele encyscum | Controversial diagnosis. Has no clinical use. We propose to reduce this diagnosis. Correction: Hydrocele on the left. |
| N43.1 | Infected hydrocele | Correction: Hydrocele on the right. |
| N43.2 | Other forms of hydrocele | Correction: Infected hydrocele. |
| N43.3 | Hydrocele, unspecified | Correction: Uninfected hydrocele. |
| N43.4 | Spermatocele | Correction: Hydrocele, unspecified. |
| Correction: N43.5 Spermatocele. | ||
| N44 | Testicular torsion | Correction: N44.0 Testicular torsion. |
| Correction: N44.1 Torsion of Morgagni's hydatid. | ||
| N45 | Orchitis and epididymitis | |
| N45.0 | Orchitis, epididymitis and epididymo-orchitis with abscess | Correction: Unilateral orchitis, epididymitis and epididymo-orchitis with abscess. |
| N45.9 | Orchitis, epididymitis and epididymo-orchitis without mention of abscess | Correction: N45.1 Unilateral orchitis, epididymitis and epididymo-orchitis without abscess. |
| Correction: N45.2 Bilateral orchitis, epididymitis and epididymo-orchitis with abscess. | ||
| Correction: N45.3 Bilateral orchitis, epididymitis and epididymo-orchitis without abscess. | ||
| N46 | Male infertility | Due to the polyetiological nature of the factors leading to male infertility, we propose to differentiate these forms depending on the causative factors. |
| Correction: N46.0 Male infertility caused by dysfunction at the level of the hypothalamus/pituitary gland. | ||
| Correction: N46.1 Male infertility caused by dysfunction at the testicular level. | ||
| Correction: N46.2 Male infertility caused by dysfunction of the efferent seminal tract and accessory sex glands. | ||
| Correction: N46.3 Male infertility caused by an ejaculation defect. | ||
| Correction: N46.4 Male infertility caused by an immunological factor. | ||
| Correction: N46.5 Male infertility caused by dysfunction of other androgen target organs. | ||
| Correction: N46.6 Male infertility, idiopathic form. | ||
| ALTERNATIVE CLASSIFICATION OF MALE INFERTILITY | ||
| Correction: N46.0 Male infertility is caused by a damaging external factor. | ||
| Correction: N46.1 Male infertility is caused by chromosomal pathology. | ||
| Correction: N46.2 Male infertility is caused by an anomaly in the structure or development of the male genital organs. | ||
| Correction: N46.3 Male infertility is caused by an endocrine factor. | ||
| Correction: N46.4 Male infertility is caused by infectious and inflammatory diseases of the male genital organs. | ||
| Correction: N46.5 Male infertility is caused by an immunological factor. | ||
| Correction: N46.6 Male infertility is caused by an iatrogenic factor. | ||
| Correction: N46.7 Male infertility is caused by an isolated pathology of seminal plasma. | ||
| Correction: N46.8 Idiopathic male infertility. | ||
| N47 | Excessive foreskin, phimosis and paraphimosis | Correction: N47.0 Excessive foreskin. |
| Correction: N47.1 Phimosis. | ||
| Correction: N47.2 Paraphimosis. | ||
| Correction: N47.3 Functional paraphimosis. | ||
| N48 | Other diseases of the penis | |
| N48.0 | Leukoplakia of the penis | |
| N48.1 | Balanoposthitis | |
| Correction: N48.1.0 Acute balanoposthitis. | ||
| Correction: N48.1.1 Chronic balanoposthitis. | ||
| N48.2 | Other inflammatory diseases of the penis | |
| Correction: N48.2.0 Cavernit. | ||
| Correction: N48.2.1 Serous cavernitis. | ||
| Correction: N48.2.2 Purulent cavernitis. | ||
| Correction: N48.2.3 Cavernous fibrosis. | ||
| N48.3 | Priapism | |
| Correction: N48.3.0 Arterial priapism. | ||
| Correction: N48.3.1 Ischemic priapism. | ||
| Correction: N48.3.2 Nocturnal intermittent priapism. | ||
| N48.4 | Impotence of organic origin | We suggest making a correction: Psychosomatic syndrome of erectile dysfunction. |
| Correction: N48.4.0 Erectile dysfunction with a predominance of the organic component. | ||
| Correction: N48.4.1 Erectile dysfunction with a predominance of the psychogenic component. | ||
| N48.5 | Penile ulcer | |
| N48.6 | Balanitis | |
| Correction: N48.6.0 Acute balanitis. | ||
| Correction: N48.6.1 Chronic balanitis. | ||
| Correction: N48.6.2 Xerotic balanitis obliterans. | ||
| N48.8 | Other specified diseases of the penis | |
| Correction: N48.8.0 Small penis. | ||
| Correction: N48.8.1 Ectopia of the penis. | ||
| Correction: N48.8.2 Double penis. | ||
| Correction: N48.8.3 Webbed penis. | ||
| Correction: N48.8.4 Retractile penis. | ||
| Correction: N48.8.5 Hidden penis. | ||
| Correction: N48.8.6 Peyronie's disease. | ||
| Correction: N48.8.6.0 Peyronie's disease in the active stage. | ||
| Correction: N48.8.6.1 Peyronie's disease in the functional stage. | ||
| N48.9 | Disease of the penis, unspecified | |
| N49 | Inflammatory diseases of the male genital organs, not elsewhere classified | |
| N49.0 | Inflammatory diseases of the seminal vesicle | Correction: Vesiculitis. |
| Correction: N49.0.0 Acute vesiculitis. | ||
| Correction: N49.0.1 Chronic vesiculitis. | ||
| N49.1 | Inflammatory diseases of the spermatic cord, tunica vaginalis and vas deferens | |
| N49.2 | Inflammatory diseases of the scrotum | |
| Correction: N49.3 Fournier's gangrene. | ||
| N49.8 | Inflammatory diseases of other specified male genital organs | |
| N49.9 | Inflammatory diseases of the unspecified male genital organ | |
| N50 | Other diseases of the male genital organs | |
| N50.0 | Testicular atrophy | |
| N50.1 | Vascular disorders of the male genital organs | Controversial diagnosis. Has no clinical significance. |
| Correction: N50.2 Contact dermatitis of the genitals. | ||
| N50.8 | Other specified diseases of the male genital organs | |
| N50.9 | Male genital disease, unspecified | |
| N51* | Lesions of the male genital organs in diseases classified elsewhere | |
| N51.0* | Lesions of the prostate gland in diseases classified elsewhere | |
| N51.1* | Lesions of the testicle and its appendages in diseases classified elsewhere | |
| N51.2* | Balanitis in diseases classified elsewhere | |
| N51.8* | Other lesions of the male genital organs in diseases classified elsewhere | |
| N51.8* | Other lesions of the male genital organs in diseases classified elsewhere | |
| N94.1 | Dyspareunia | |
| N99 | Disorders of the genitourinary system after medical procedures not classified elsewhere | |
| N99.1 | Postoperative urethral stricture | |
| N99.8 | Other disorders of the genitourinary system after medical procedures | |
| N99.9 | Disorders of the genitourinary system after medical procedures, unspecified | |
| Q53 | Undescended testicle | |
| Q53.0 | Ectopic testicle | |
| Q53.1 | Unilateral undescended testicle | |
| Q53.2 | Bilateral undescended testicle | |
| Correction: Q53.3 Pseudocryptorchidism. | ||
| Q53.9 | Undescended testicle, unspecified | |
| Q54 | Hypospadias | |
| Q54.0 | Hypospadias of the glans penis | |
| Q54.1 | Penile hypospadias | |
| Q54.2 | Hypospadias penis-scrotum | |
| Q54.3 | Perineal hypospadias | |
| Q54.4 | Congenital curvature of the penis | |
| Q54.8 | Other hypospadias | Correction: Hypospadias without hypospadias. |
| Q54.9 | Hypospadias, unspecified | |
| Q55 | Other congenital anomalies [malformations] of the male genital organs | |
| Q55.0 | Absence and aplasia of the testicle | |
| Q55.1 | Testicular and scrotal hypoplasia | |
| Q55.2 | Other congenital anomalies of the testicle and scrotum | |
| Correction: Q55.2.0 Monorchidism. | ||
| Correction: Q55.2.0.0 Monorchidism on the right. | ||
| Correction: Q55.2.0.1 Monorchidism on the left. | ||
| Correction: Q55.2.1 Polyorchidism. | ||
| Correction: Q55.2.2 Synorchidism. | ||
| Q55.3 | Atresia of the vas deferens | |
| Q55.4 | Other congenital anomalies of the vas deferens, epididymis, spermatic cord and prostate | |
| Q55.5 | Congenital absence and aplasia of the penis | |
| Q55.6 | Other congenital anomalies of the penis | |
| Q55.8 | Other specified congenital anomalies of the male genital organs | |
| Q55.9 | Congenital anomaly of the male genital organs, unspecified | |
| Q56 | Sex ambiguity and pseudohermaphroditism | |
| Q56.0 | Hermaphroditism, not elsewhere classified | |
| Q56.1 | Male pseudohermaphroditism, not elsewhere classified | |
| Q56.3 | Pseudohermaphroditism, unspecified | |
| Q56.4 | Gender ambiguity, unspecified | |
| Q64 | Other congenital anomalies [malformations] of the urinary system | |
| Q64.0 | Epispadias | |
| Correction: Q64.0.0 Epispadias of the head. | ||
| Correction: Q64.0.1 Penile epispadias. | ||
| Correction: Q64.0.2 Total epispadias. | ||
| Q64.1 | Bladder exstrophy | |
| Q64.2 | Congenital posterior urethral valves | |
| Q64.3 | Other types of atresia and stenosis of the urethra and bladder neck | |
| Q64.5 | Congenital absence of the bladder and urethra | |
| Q64.7 | Other congenital anomalies of the bladder and urethra | |
| Q64.8 | Other specified congenital anomalies of the urinary system | |
| Q64.9 | Congenital anomaly of the urinary system, unspecified | |
| Q89.7 | Multiple congenital anomalies not elsewhere classified | |
| Q89.8 | Other specified congenital anomalies | |
| Q89.9 | Congenital anomaly, unspecified | |
| Q92.7 | Triploidy and polyploidy | |
| Q95.3 | Balanced sexual/autosomal rearrangements in a normal individual | |
| Q98.0 | Klinefelter syndrome, karyotype 47,XXY | |
| Q98.1 | Klinefelter syndrome, male with more than two X chromosomes | |
| Q98.2 | Klinefelter syndrome, man with 46,XX karyotype | |
| Q98.3 | Another man with a 46,XX karyotype | |
| Q98.4 | Klinefelter's syndrome, unspecified | |
| Q98.5 | Karyotype 47,XYU | |
| Q98.6 | A man with structurally altered sex chromosomes | |
| Q98.7 | Male with mosaic sex chromosomes | |
| Q98.8 | Other specified sex chromosome abnormalities, male phenotype | |
| Q98.9 | Sex chromosome abnormality, male phenotype, unspecified | |
| Q99 | Other chromosomal abnormalities not elsewhere classified | |
| Q99.0 | Mosaic [chimera] 46,ХХ/46,ХY | |
| Q99.1 | 46.XX true hermaphrodite | |
| Q99.2 | Fragile X chromosome | |
| Q99.8 | Other specified chromosomal abnormalities | |
| Q99.9 | Chromosomal abnormality, unspecified | |
| R10.2 | Pain in the pelvis and perineum | |
| R30.9 | Painful urination, unspecified | |
| R32 | Urinary incontinence, unspecified | |
| R33 | Urinary retention | |
| R36 | Discharge from the urethra | |
| R39 | Other symptoms and signs related to the urinary system | |
| R39.1 | Other difficulties related to urination | |
| R39.8 | Other and unspecified symptoms and signs related to the urinary system | |
| R44.8 | Other and unspecified symptoms and signs relating to general sensations and perceptions | |
| R45 | Symptoms and signs related to emotional state | |
| R45.0 | Nervousness | |
| R45.1 | Anxiety and agitation | |
| R45.2 | State of anxiety due to failures and misfortunes | |
| R45.3 | Demoralization and apathy | |
| R45.4 | Irritability and anger | |
| R45.7 | State of emotional shock and stress, unspecified | |
| R45.8 | Other symptoms and signs related to emotional state | |
| R46 | Symptoms and signs related to appearance and behavior | |
| R52.1 | Constant, unrelieved pain | |
| R52.2 | Other constant pain | |
| R52.9 | Unspecified pain | |
| R53 | Malaise and fatigue | |
| R54 | Old age | Controversial diagnosis. |
| R62 | Lack of expected normal physiological development | |
| R62.0 | Delayed developmental milestones | |
| R62.8 | Other delays in expected normal physiological development | |
| R62.9 | Lack of expected normal physiological development, unspecified | |
| S30.2 | Bruise of the external genitalia | |
| S31.2 | Open wound of the penis | |
| S31.3 | Open wound of the scrotum and testicles | |
| S31.5 | Open wound of other and unspecified external genitalia | |
| S38.0 | Crushing of the external genitalia | |
| S38.2 | Traumatic amputation of the external genitalia | |
| T19 | Foreign body in the genitourinary tract | |
| T19.0 | Foreign body in the urethra | |
| T19.8 | Foreign body in another or several parts of the genitourinary tract | |
| T19.9 | Foreign body in an unspecified part of the genitourinary tract | |
| Z84.2 | Family history of other diseases of the genitourinary system | |
| Z87.4 | Personal history of diseases of the genitourinary system | |
| Z90.7 | Acquired absence of sexual organ(s) | |
| Z99.8 | Dependence on other auxiliary mechanisms and devices | |
This summary table shows those symptoms, syndromes and nosological forms according to ICD10 that a practicing specialist in the field of andrology encounters in real practice. At the same time, in our opinion, some of them no longer correspond to the modern understanding of pathophysiological processes and require terminological and classification clarification (right column).
Naturally, the above classification needs to be supplemented and refined, and fundamental amendments be made taking into account interdisciplinary interaction. With our publication, we would like to provoke a discussion among specialists in the field of andrology, the main goal of which would be to create a single, integral classification of andrological diseases. This is undoubtedly valuable and convenient for medical practitioners, health authorities, scientific research, and insurance companies. We will be grateful for your comments and remarks, which can be sent to the email address
Key words: ICD-10, andrological diseases, clinical and statistical classification.
Keywords : ICD-10, andrology diseases, clinical and statistical classification.
Literature
- International classification of diseases and related health problems. WHO, 1992
- Order of the Ministry of Health of the Russian Federation dated May 27, 1997 No. 170 (as amended on January 12, 1998) “On the transition of health authorities and institutions of the Russian Federation to the international statistical classification of diseases and health-related problems of the X revision.”
- Sivkov A.V., Kakorina E.P., Keshishev N.G. Unified clinical and statistical classification of urological diagnoses // Materials of the XI Congress of Urologists of Russia. M. 2007. pp. 598-599.
- Unified clinical and statistical classification of urolithiasis / Apolikhin O.I., Dzeranov N.K., Sivkov A.V., Kakorina E.P., Keshishev N.G. // Urology. 2008. No. 6. P. 3-6.
- On the creation of a unified clinical and statistical classification of oncological urological diseases using the example of kidney tumors / Apolikhin O.I., Sivkov A.V., Chernyshev Yu.V., Kakorina E.P., Keshishev N.G., Zhernov A.A. // Experimental and clinical urology. 2010. No. 1. pp. 23-28.
| Attached file | Size |
| Article in PDF format | 414.14 kb |
Causes of inflammation of the appendages
Normally, no bacteria live in the uterine appendages: neither beneficial nor harmful. However, with various diseases, their complications, and even if the rules of basic hygiene are violated, bacteria can get inside and lead to the development of inflammation.
Transmission of pathogens through sexual contact is also possible. Most often this happens with hidden infections, which cannot be noticed for a long time without testing. It is hidden infections that are the most dangerous. Once in the acidic environment of the vagina, microorganisms that carry diseases either die (with normal immunity) or move to the uterine appendages (with weakened immunity).
Causes
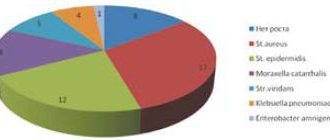
The main causes of salpingoophoritis are pathogenic microflora. This can be either a banal coccal flora (streptococci, staphylococci) or sexually transmitted infections - ureaplasma, mycoplasma, chlamydia, gonococci, trichomonas.
- Acute salpingoophoritis usually develops against the background of systemic pathology, due to a decrease in the immune function of the body. Provoking factors in this case may be severe stress, hypothermia, failure to comply with the rules of intimate hygiene, unprotected sexual intercourse and a number of other, at first glance, insignificant points.
- Chronic salpingoophoritis is, as a rule, a consequence of incomplete or improper treatment of the acute form of the disease or relapses if the above provoking factors are constantly repeated. This form of the disease is especially dangerous due to the sluggish nature of the course and the tendency to develop complications. From the perineum and vagina, pathogenic microorganisms enter the uterine cavity and fallopian tubes. By intensively multiplying, bacteria and their metabolic products damage the mucous membrane, provoking an inflammatory process. Toxins released into the blood cause intoxication syndrome (read more here).
If salpingoophoritis develops as a secondary process, the infection enters the appendages with blood. The further mechanism of development does not differ from that during the ascending process.
Risk factors for inflammation of the appendages:
- Promiscuous sexual intercourse without the use of protection
- Intrauterine interventions, operations performed without the proper level of antiseptics
- Diseases of the female genital organs of an inflammatory nature that have not been fully cured or have become chronic
- Hypothermia
It is important to understand that it is better to cure the disease completely once than to transform it into a chronic form by quitting treatment, or to deal with complications of the disease that can lead to infertility.
Literature
- A.U. Hamadyanova. Chronic recurrent salpingoophoritis: current state of the problem // Medical Bulletin of Bashkortostan - 2013 - Volume 8 - No. 3 - pp. 123-130. https://cyberleninka.ru/article/n/hronicheskiy-retsidiviruyuschiy-salpingooforit-sovremennoe-sostoyanie-problemy/viewer
- A.V.Shurshalina. Inflammatory diseases of the pelvic organs: modern treatment tactics // American Medical Center, Moscow - 2011 p. 28-31. https://www.akrikhin.ru/upload/iblock/4f4/4f4f7b9982433c19859b3f609fd499a5.pdf
- Tikhomirov A.L., Bataeva A.E., Sarsania S.I. Empirical antibiotic therapy for acute salpingo-oophoritis in outpatient practice // RMZh. Mother and Child No. 4 - 02.25.2010 - 196 S. https://www.rmj.ru/articles/pediatriya/Empiricheskaya_antibiotikoterapiya_ostryh__salypingooforitov_v_ambululatornoy_praktike/
- Instructions for medical use of the drug Motrin ®
- International Classification of Diseases 10th revision – 2021. https://mkb-10.com/index.php?pid=13321
- Gynecology. Guide to practical classes: textbook / Ed. V.E. Radzinsky. 3rd ed., revised. and additional 2020. - 552 pp.: ill. — ISBN 978-5-9704-5459-6.
- O.G. Putintseva, E.V. Verevkina Inflammatory diseases of the pelvic organs study guide – 2021.
- Diseases caused by exposure to thermal factors (heat and cold) on the body - Educational and methodological manual for practical classes in internal medicine (military therapy) - 2017.
- L.I. Maltseva, R.I. Sharipova, E.A. Gafarova - Treatment of inflammatory diseases of the pelvic organs in women - Training manual for doctors - 2021.
- Maksimov M.L. Topical issues of the effectiveness and safety of modern non-steroidal anti-inflammatory drugs // Regular issues of “RMZh” No. 28 - 09.12.2014 - 2015 pp. https://www.rmj.ru/articles/revmatologiya/Aktualynye_voprosy_effektivnosti_i_bezopasnosti_sovremennyh_nesteroidnyh_protivovospalitelynyh_preparatov /
- Buralkina N.A., Katkova A.S., Arutyunova E.E., Zhorova V.E., Batyrova Z.K., Vlasova G.A. Inflammatory diseases of the pelvic organs: pathogenetic aspects, diagnosis, clinic, treatment // Gynecology - 2021 - Volume 20 - No. 3. https://cyberleninka.ru/article/n/vospalitelnye-zabolevaniya-organov-malogo-taza-pathogeneticheskie-aspekty-diagnostika-klinika-lechenie-obzor-literatury/viewer
- Sekhin S.V. Antibacterial therapy for diseases of the pelvic organs: a rational choice in Russian conditions // Breast Cancer. Mother and Child No. 1 - 01/30/2014 - 83 C. https://www.rmj.ru/articles/antibiotiki/Antibakterialynaya_terapiya_vospalitelynyh_zabolevaniy_organov_malogo_taza_racionalynyy_vybor_v_rossiyskih_usloviyah
- Fricke JR, Halladay SC, Francisco CA. Efficacy and safety of naproxen sodium and ibuprofen for pain relief after oral surgery.Curr Ther Research. 1993;54(6):619-27.
Up to contents
Diagnosis of the disease
In order for you to be able to control the diagnostic process yourself and know what stages the study should consist of, we decided to tell you what stages the diagnosis of inflammation of the appendages consists of at GMS Clinic.
- Collection of blood for a general blood test. Based on the results, special attention, as noted above, is given to the level of leukocytes and ESR.
- The gynecologist first conducts a survey to identify possible symptoms of inflammation of the appendages, and then conducts an examination. The first thing a specialist pays attention to is pain in the ovaries and cervix during examination and in the medical history.
- During the examination, the specialist must take a smear to culture the flora and conduct further analysis to identify the exact causative agent of the disease, if it is detected.
- If necessary, the doctor may suggest ultrasound diagnostics. This is a completely painless procedure, which is carried out with a vaginal sensor. Ultrasound diagnostics will allow you to collect more information about the condition of the body and select the most optimal treatment regimen.
Correct diagnosis of inflammation of the appendages guarantees the choice of the most optimal treatment regimen. If, nevertheless, a specialist has diagnosed inflammation of the appendages, you should not think that the disease will go away on its own. The sooner you start treatment, the greater the chances of avoiding consequences and starting a healthy life without pain!
Therapy
Treatment of acute salpingoophoritis or during exacerbations is carried out in a specialized hospital. Therapy includes the prescription of antibacterial drugs, which is carried out taking into account the sensitivity of the flora to them and the type of causative agent of the disease. Simultaneously with antibacterial therapy, detoxification therapy is prescribed, during which special anti-inflammatory suppositories are used, which reduce temperature, relieve inflammation and have an analgesic effect on the affected pelvic organs.
After the inflammatory process is relieved, the patient is prescribed absorbable medications and physiotherapeutic procedures. They will prevent the appearance of adhesions in the fallopian tubes, reducing the risk of infertility and ectopic pregnancy in the future.
If conservative treatment does not produce results, then surgery is indicated, usually laparoscopy. The scope of the operation is determined individually. If an abscess forms, the fallopian tube is removed as a source of infection. To restore the patency of the appendages, adhesions are cut and rough scars are removed.
Chronic salpingoophoritis during periods of exacerbation is treated similarly to acute. During the remission phase, the use of physiotherapy is indicated. The appropriateness of prescribing a particular technique is determined by the attending physician, depending on the severity of menstrual irregularities, the presence of adhesions, and the symptoms of the disease. Treatment includes techniques such as ultrasound, magnetic fields, pulsed currents, reflexology, mineral waters, mud in the form of applications, irrigations, baths. These procedures have a beneficial effect on general and local immunity, improve blood supply to the pelvic organs, enhance regenerative processes, and restore hormonal balance.
Patients with inflammation of the appendages are not recommended to visit hot countries with a humid climate; it is better to give preference to balneological hospitals and local sanatoriums. If the pathology causes infertility, an IVF procedure is indicated. This technique allows you to give birth to a child even for those women who have a history of hormonal or tubal infertility. Pregnancy after IVF usually proceeds normally. Hormonal support is rarely necessary to prevent spontaneous miscarriage.
Options for surgical treatment of salpingoophoritis
Treatment of inflammation of the appendages (adnexitis)
Treatment of inflammation of the uterus and ovaries is carried out in several directions at once. The first direction is the fight against the inflammatory process itself, the second is antimicrobial therapy, and the third is restorative therapy measures.
After starting treatment, the symptoms of acute inflammation disappear after a few days, but this does not mean that the disease has receded.
Specialists at the GMS Clinic Center for Obstetrics and Gynecology select the most optimal treatment regimen for adnexitis in each individual case, because each organism is unique and requires a special approach.
You have questions? We will be happy to answer any questions Coordinator Tatyana
How to treat adnexitis?
Depending on the form and symptoms of adnexitis, treatment will be different:
- Acute adnexitis is treated in a clinical setting; hospitalization is necessary to provide the woman with complete rest. Drug therapy includes taking anti-inflammatory and painkillers, and antibiotics for adnexitis must have a long period of decay and elimination. It is important to adhere to a special diet that includes drinking plenty of fluids. To minimize the likelihood of developing adhesions in the acute form, physical therapy, including the use of biostimulants, can be prescribed.
- Purulent adnexitis may require laparoscopy, during which purulent contents are removed from the ovary, and an antibiotic and anti-inflammatory drug are injected in its place.
- Exacerbation of bilateral or unilateral adnexitis is primarily treated with local therapy. In this case, treatment of adnexitis includes douching with an antiseptic solution, paraffin therapy, and physiotherapy with ozokerite.
- Advanced cases of adnexitis, threatening peritonitis and sepsis, are treated with a complex of antibiotics - orally and intravenously. In order to remove toxins that have entered the body as a result of a long-term inflammatory process, the patient is prescribed infusion therapy. The most complex cases may require removal of the epididymis.
Prevention of inflammation of the appendages:
- Timely implementation of hygiene procedures to protect against infection entering internal cavities;
- If possible, avoid unprotected sexual intercourse;
- Protect yourself from surgical termination of pregnancy. The easiest way to do this is by using barrier methods of contraception;
- Regular visits to the gynecologist and a smear test for internal flora analysis.
Most often, a visit to a specialist helps to identify the disease and prevent its development in time. In addition, you can contact a herbalist who will create for you a personal collection of herbs that protect the body and help it fight infections.
Prevention of adnexitis
After a course of treatment, it is very important to draw conclusions and eliminate risk factors. In order not to encounter this problem again, you need to follow the rules of personal hygiene, use condoms during casual sexual contacts, and maintain immunity2.
Do not underestimate such a risk factor as hypothermia, because it can be encountered not only at extremely low, but also above-zero temperatures. Hypothermia occurs more quickly with high air humidity, especially in strong winds. Also, the body's resistance to cooling may decrease during physical fatigue, fasting, or after drinking alcohol8.
Avoid hypothermia, always dress appropriately for the weather and keep your feet warm. Shoes should be comfortable, not compressing the feet and toes - this way the blood flow in the tissues is not disturbed and they better withstand the effects of cold8.
If you find yourself with symptoms of adnexitis, even if they are not expressed, be sure to consult a doctor. He will determine the cause of the disease and help relieve symptoms.
Up to contents