Pharmacological properties of the drug Lantus
Pharmacodynamics . Insulin glargine is an analogue of insulin, obtained using recombinant DNA technology using the K12 strain of E scherichia coli , has a structure identical to human insulin. Reduces blood glucose levels. It has low solubility at neutral pH and is completely soluble in acidic media. The pH value of the injection solution is 4. After subcutaneous administration, the acidic solution is neutralized in the tissue, which leads to the formation of microsediment/microprecipitates, from which insulin glargine is gradually released, which ensures a smooth, peak-free drug concentration profile in the blood. These properties of insulin glargine ensure a long-lasting effect of the drug. Like human insulin, insulin glargine binds to insulin receptors, causing the same physiological effects, primarily affecting glucose metabolism. Insulin and its analogues reduce blood glucose levels by increasing its utilization in peripheral tissues, particularly in skeletal muscle and adipose tissue, and inhibiting glucose production in the liver. Insulin inhibits lipolysis and proteolysis and enhances protein biosynthesis. Pharmacokinetics. With intravenous administration of insulin glargine and human insulin in equal doses, their effects are equivalent. The onset of action of insulin glargine after subcutaneous administration is more gradual, the concentration in the blood is stable (there are no peaks in blood concentration), and the duration of action is prolonged compared to human insulin. Such effects of insulin glargine are directly due to slow absorption and allow the drug to be used once a day. In patients with type I diabetes mellitus, the time of optimal effectiveness between injection and the end of pharmacotherapeutic action is 14.5 hours (from 9.5 to 19.3 hours) for human insulins and 24 hours (from 10.8 to 24 hours or more ) for insulin glargine. Stable insulin levels are achieved 2–4 days after the start of administration. In humans, insulin glargine is partially broken down in subcutaneous fat by carboxylation of the beta chain to form the active metabolites 21A-Gly insulin and des-30B insulin. Both unchanged insulin glargine and its metabolic products are detected in blood plasma. In clinical studies, when analyzing subgroups formed by age and gender, no differences were noted regarding the safety and effectiveness of insulin glargine.
Lantus® SoloStar® (Lantus® SoloStar®)
Insulin glargine is an analogue of human insulin, obtained by recombination of DNA from bacteria of the species Escherichia coli
(
strains K12), and is characterized by low solubility in a neutral medium.
In the composition of Lantus® SoloStar®, insulin glargine is completely soluble, which is ensured by the acidic reaction of the injection solution (pH 4). After injection into the subcutaneous fat, the acidity of the solution is neutralized, resulting in the formation of microprecipitates from which small amounts of insulin glargine are continuously released, providing a predictable, smooth (no peaks) profile of the con-Pharmacokinetics curve).
Connection with insulin receptors:
The kinetics of binding to specific insulin receptors of insulin glargine and its metabolites M1 and M2 are very close to those of human insulin, and therefore insulin glargine is capable of exerting biological effects similar to those of endogenous insulin.
The most important action of insulin and its analogues, including insulin glargine, is the regulation of glucose metabolism. Insulin and its analogues reduce blood glucose concentrations by stimulating glucose uptake into peripheral tissues (especially skeletal muscle and adipose tissue) and inhibiting glucose production in the liver. Insulin suppresses lipolysis in adipocytes and inhibits proteolysis, while simultaneously increasing protein synthesis. The prolonged action of insulin glargine is directly related to the reduced rate of its absorption, which allows the drug to be used once a day. After subcutaneous administration, the onset of action occurs after an average of 1 hour. The average duration of action is 24 hours, the maximum is 29 hours. The duration of action of insulin and its analogues, such as insulin glargine, can vary significantly between different patients or within the same patient .
The effectiveness of the use of the drug Lantus® SoloStar® in children over 2 years of age with type 1 diabetes mellitus has been shown. In children in the age group 2-6 years, the incidence of hypoglycemia with clinical manifestations when using insulin glargine was numerically lower, both during the day and at night, compared with the use of isophane insulin (correspondingly, an average of 25.5 episodes vs. 33.0 episodes per patient over one year).
During a five-year follow-up of patients with type 2 diabetes, there were no significant differences in the progression of diabetic retinopathy when treated with insulin glargine compared with isophane insulin.
Binding to insulin-like growth factor 1 (IGF-1) receptors: The affinity of insulin glargine for the IGF-1 receptor is approximately 5-8 times higher than that of human insulin (but approximately 70-80 times lower than that of IGF-1), at the same time, compared to human insulin, the insulin glargine metabolites M1 and M2 have slightly less affinity for the IGF-1 receptor.
The total therapeutic concentration of insulin (insulin glargine and its metabolites) determined in patients with type 1 diabetes mellitus was markedly lower than the concentration required for half-maximal binding to IGF-1 receptors and subsequent activation of the mitogenic-proliferative pathway triggered through IGF-1 receptors.
Physiological concentrations of endogenous IGF-1 can activate the mitogenic-proliferative pathway, however, therapeutic concentrations of insulin determined during insulin therapy, including treatment with Lantus® SoloStar®, are significantly lower than the pharmacological concentrations required to activate the mitogenic-proliferative pathway.
The ORIGIN (Outcome Reduction with Initial Glargine INtervention) study was an international, multicenter, randomized trial conducted in 12,537 patients at high risk for cardiovascular disease and with impaired fasting glucose (IFG), impaired glucose tolerance (IGT), or early stage diabetes. type 2 diabetes. Study participants were randomized (1:1) to receive insulin glargine (n=6264), titrated to achieve a fasting blood glucose (FBG) concentration of ≤5.3 mmol, or to receive standard care (n =6273).
The first endpoint of the study was the time to the first occurrence of cardiovascular death, the first occurrence of nonfatal myocardial infarction, or the first nonfatal stroke, and the second endpoint was the time to the first occurrence of any of the above complications or to a revascularization procedure (coronary, carotid, or peripheral arteries). , or before hospitalization for the development of heart failure. Secondary endpoints were all-cause mortality and a composite measure of microvascular outcomes.
The ORIGIN study showed that treatment with insulin glargine, compared with standard hypoglycemic therapy, did not change the risk of cardiovascular events or cardiovascular mortality; There were no differences in any of the endpoints, all-cause mortality, or the composite microvascular outcome measure.
At baseline, the median HbAlc value was 6.4%. Median HbAlc values during treatment ranged from 5.9-6.4% in the insulin glargine group and 6.2-6.6% in the standard treatment group throughout the observation period.
In the group of patients receiving insulin glargine, the incidence of severe hypoglycemia was 1.05 episodes per 100 patient-years of therapy, and in the group of patients receiving standard hypoglycemic therapy - 0.30 episodes per 100 patient-years of therapy. The incidence of non-severe hypoglycemia in the group of patients receiving insulin glargine was 7.71 episodes per 100 patient-years of therapy, and in the group of patients receiving standard hypoglycemic therapy - 2.44 episodes per 100 patient-years of therapy. In a 6-year study, 42% of patients in the insulin glargine group did not experience any hypoglycemia. The median change in body weight from outcome at the last treatment visit was 2.2 kg higher in the insulin glargine group than in the standard care group.
Use of the drug Lantus
Inject s/c into the area of the anterior abdominal wall, deltoid muscle or thigh once a day, at the same time. The dose is set individually. To administer the drug, you must use only syringes graduated at 100 IU! Lantus should not be administered intravenously, since administration at the usual dose for subcutaneous administration can lead to the development of severe hypoglycemia. Lantus should not be mixed with any other insulin or diluted as this may alter the timing/pattern of action of the drug and lead to the formation of a precipitate. In patients with type II diabetes mellitus, Lantus can be used simultaneously with oral hypoglycemic agents; in this case, the average initial dose of Lantus is 10 IU/day, subsequently from 2 to 100 IU/day. Switching from other insulins. When switching from intermediate-acting insulin or from long-acting insulin to Lantus, there may be a need to adjust the dose of basal insulin, as well as change the dosage regimen of oral hypoglycemic agents and short-acting insulin analogues. In order to reduce the risk of developing nocturnal or early morning hypoglycemia, patients who are switching from double human insulin to Lantus once daily should reduce the dose of basal insulin by 20–30% during the first weeks of treatment. This reduction in the dose of basal insulin should be temporarily compensated by increasing the dose of insulin administered with meals. At the end of the preparatory period, insulin doses are adjusted again. As with the use of other insulin analogues, in patients who receive high doses of insulin, due to the presence of antibodies to human insulin, the response to insulin may improve when treated with Lantus SoloStar, which requires dose adjustment. This is especially important to consider in overweight patients when changing their lifestyle. Lantus is administered subcutaneously once a day, at the same time, in an individually selected dose. The syringe pen allows you to administer the drug in a single dose range from 2 to 40 IU. The drug should not be administered intravenously, since administration of the usual dose in this case can lead to the development of severe hypoglycemia. There are no clinically significant differences in plasma insulin or glucose levels after administration of the drug to the anterior abdominal wall, deltoid muscle or thigh. The injection site can be changed in a circle. The drug can be used only if the solution upon visual examination is transparent and colorless (or practically colorless), without particles visible to the eye. Immediately before injection, it is necessary to remove the air bubble from the syringe. Mixing the drug with other products is not allowed, as this may lead to the formation of sediment. Each time you inject, you should use a new needle for the syringe pen. After the injection, the needle must be removed and the syringe pen must be stored without a needle. There is no need to shake the pen before use. Before use, the syringe pen must be kept for 1–2 hours at room temperature. To attach the needle, remove the protective label from the needle container without removing the outer and inner needle caps. Carefully attach the needle and its outer cap exactly to the transparent reservoir (by screwing or pressing, depending on the type of needle). Do not attach the needle at an angle as this may cause it to break or cause insulin to leak out of the system and result in incorrect dosing. When attaching, do not press the needle too hard. Make sure the dose button is pressed. A safety test must be performed before each injection. For the first safety test, the dose should be 8 units of insulin using a new, previously unused pen. Make sure the dose indicator points to 8. If it does not, use a new pen. Pull out the dose button as far as possible. Do not return the dose switch if the dose button is pulled out. For a pen that has already been used, set the dose indicator to number 2 by rotating the dosing switch. The dosing switch can be rotated in any direction. Pull out the dose button. Check whether the number on the button corresponds to the dose selected on the dosing switch. Black marks indicate the number of units. The last thick line visible on the button (only the top part is visible) indicates the charged dose. To see the last thick line, you can rotate or tilt the pen. Remove the inner and outer needle caps. Holding the pen with the needle up, lightly tap the insulin container with your fingertip so that air bubbles rise up towards the needle. Press the dose button all the way to release the dose. You may feel a clicking sound that will stop when you press the dose button all the way. If insulin appears at the tip of the needle, the device is working properly. If insulin does not appear at the tip of the needle, repeat the instructions above. If a drop of insulin does not appear even after repeating the safety test, check the device for air bubbles. If they are present, repeat the safety test until they disappear. If there are no air bubbles, the needle may become clogged; in this case it should be replaced. After inserting the needle, press the dose button all the way. Leave the needle in the skin for at least 10 seconds. The dose button must remain pressed until the needle is removed. After removal, the needle is unscrewed by rotating the cap. The needle can only be used once. Checking the reservoir for remaining insulin The scale on the transparent reservoir indicates the amount of insulin remaining in the syringe pen. This scale is not intended to indicate insulin dosage. If the black plunger is near the 40 mark at the beginning of the color stop, this means that the remaining insulin volume in the pen is approximately 40 IU. The end of the colored stopper indicates that the pen contains approximately 20 IU of insulin. If the insulin level in the reservoir is low, you can check the insulin level using the dose button. You should not use a pen unless you are sure there is enough insulin left in it for the next dose. For example, if the dose indicator is set to 30 IU, but the dose button is pulled out no more than 12 IU, this means that the pen can only deliver 12 IU of insulin. In this case, the missing 18 IU can be injected using a new pen, or a new pen can be used to inject the full dose of 30 IU of insulin.
Lantus SoloStar, 5 pcs., 3 ml, 100 U/ml, solution for subcutaneous administration
PC.
Adults and children over 2 years old.
General recommendations
Lantus® SoloStar® should be administered subcutaneously once a day at any time of the day, but every day at the same time.
In patients with type 2 diabetes mellitus, Lantus® SoloStar® can be used both as monotherapy and in combination with other hypoglycemic drugs.
Target values for blood glucose concentrations, as well as the dose and timing of administration or administration of hypoglycemic drugs should be determined and adjusted individually.
Dose adjustments may also be necessary, for example, if the patient changes in weight, lifestyle, changes in the timing of insulin dosing, or other conditions that may increase the susceptibility to developing hypo- or hyperglycemia (see "Special Instructions"). Any changes in insulin dosage should be made with caution and under medical supervision.
Lantus® SoloStar® is not the insulin of choice for the treatment of diabetic ketoacidosis. In this case, preference should be given to intravenous administration of short-acting insulin.
In treatment regimens that include basal and prandial insulin injections, 40–60% of the daily insulin dose is typically administered as insulin glargine to meet basal insulin requirements.
In patients with type 2 diabetes mellitus using oral hypoglycemic drugs, combination therapy begins with a dose of insulin glargine 10 units once a day, and subsequently the treatment regimen is adjusted individually.
Monitoring blood glucose concentrations is recommended in all patients with diabetes.
Switching from treatment with other hypoglycemic drugs to Lantus® SoloStar®
When transferring a patient from a treatment regimen using intermediate-acting or long-acting insulin to a treatment regimen using Lantus® SoloStar®, it may be necessary to adjust the amount (doses) and time of administration of short-acting insulin or its analogue during the day or change the doses of oral hypoglycemic drugs .
When transferring patients from a single daily administration of isophane insulin to a single daily administration of Lantus® SoloStar®, the initial doses of insulin usually do not change (i.e., the number of units/day of Lantus® SoloStar® equal to the number of IU/day is used insulin isophane).
When transferring patients from twice daily administration of isophane insulin to a single administration of Lantus® SoloStar® before bedtime in order to reduce the risk of hypoglycemia at night and early morning, the initial daily dose of insulin glargine is usually reduced by 20% (compared to the daily dose insulin isophane), and then it is adjusted depending on the patient's response.
Lantus® SoloStar® should not be mixed with other insulin preparations or diluted. It is necessary to ensure that the syringes do not contain residues of other drugs. Mixing or diluting may change the time profile of insulin glargine.
When switching from human insulin to Lantus® SoloStar® and during the first weeks after it, careful metabolic monitoring (control of blood glucose concentrations) under medical supervision is recommended, with correction of the insulin dosage regimen if necessary. As with other human insulin analogues, this is especially true for patients who, due to the presence of antibodies to human insulin, require the use of high doses of human insulin. In such patients, when using insulin glargine, there may be a significant improvement in the response to insulin administration.
With improved metabolic control and the resulting increase in tissue sensitivity to insulin, it may be necessary to adjust the insulin dosage regimen.
Mixing and dilution
The drug Lantus® SoloStar® cannot be mixed with other insulins. Mixing may change the time/action ratio of Lantus® SoloStar® and may result in precipitation.
Special patient groups
Children.
The drug Lantus® SoloStar® can be used in children over 2 years of age. Use in children under 2 years of age has not been studied.
Elderly patients.
In elderly patients with diabetes mellitus, it is recommended to use moderate initial doses, slowly increase them and use moderate maintenance doses.
Mode of application
The drug Lantus® SoloStar® is administered as a subcutaneous injection. Not intended for intravenous administration. A long duration of action of insulin glargine is observed only when it is administered into the subcutaneous fat. IV administration of the usual subcutaneous dose may cause severe hypoglycemia. Lantus® SoloStar® should be injected into the subcutaneous fat of the abdomen, shoulders or thighs. Injection sites should be alternated with each new injection within the recommended areas for subcutaneous administration of the drug.
As with other types of insulin, the extent of absorption, and therefore the onset and duration of action, may vary due to exercise and other changes in the patient's condition.
Lantus® SoloStar® is a clear solution, not a suspension. Therefore, resuspension before use is not required.
If the Lantus® SoloStar® syringe pen malfunctions, insulin glargine can be removed from the cartridge into a syringe (suitable for insulin 100 IU/ml) and the necessary injection can be made.
Instructions for use and handling of the SoloStar® pre-filled syringe pen
Before first use, the syringe pen must be kept at room temperature for 1–2 hours.
Before use, you should inspect the cartridge inside the syringe pen. It should only be used if the solution is clear, colorless, contains no visible solids, and has a consistency similar to water.
Empty SoloStar® syringe pens should not be reused and must be destroyed.
To prevent infection, the prefilled pen should only be used by one patient and not shared with another person.
Handling the SoloStar® syringe pen
Before using the SoloStar® syringe pen, you should carefully read the information on use.
Important information on using the SoloStar® syringe pen
Before each use, carefully attach a new needle to the pen and perform a safety test. Only needles compatible with SoloStar® should be used.
Special precautions must be taken to avoid needle-related accidents and the possibility of transmitting infection.
Under no circumstances should you use the SoloStar® syringe pen if it is damaged or if you are not sure that it will work properly.
It is always necessary to have a spare SoloStar® syringe pen available in case of loss or damage to the previous copy of the SoloStar® syringe pen.
Storage instructions
You should study the section “Storage Conditions” regarding the rules for storing the SoloStar® syringe pen.
If the SoloStar® syringe pen is stored in the refrigerator, you should remove it from there 1–2 hours before the intended injection so that the solution reaches room temperature. Injecting chilled insulin is more painful.
The used SoloStar® syringe pen must be destroyed.
Exploitation
The SoloStar® syringe pen must be protected from dust and dirt.
The outside of the SoloStar® syringe pen can be cleaned by wiping it with a damp cloth.
Do not immerse the SoloStar® syringe pen in liquid, rinse or lubricate it, as this can damage the SoloStar® syringe pen.
The SoloStar® syringe pen accurately doses insulin and is safe to use. It also requires careful handling. Situations in which damage to the SoloStar® syringe pen may occur should be avoided. If there is a suspicion that the SoloStar® syringe pen you are using is damaged, you should use a new syringe pen.
Stage 1: Insulin control
It is necessary to check the label on the SoloStar® pen to ensure that it contains the appropriate insulin. For Lantus®, the SoloStar® syringe pen is gray with a purple button for injection. After removing the cap of the syringe pen, the appearance of the insulin contained in it is controlled: the insulin solution should be transparent, colorless, free of visible solid particles and resemble water in consistency.
Stage 2. Connecting the needle
It is necessary to use only needles that are compatible with the SoloStar® syringe pen.
For each subsequent injection, always use a new sterile needle. After removing the cap, the needle must be carefully installed on the syringe pen.
Stage 3: Carrying out the safety test
Before each injection, a safety test must be performed to ensure that the pen and needle are working properly and that air bubbles have been removed.
Measure out a dose equal to 2 units.
The outer and inner needle caps must be removed.
With the syringe pen facing upward, gently tap the insulin cartridge with your finger so that all air bubbles are directed towards the needle.
Fully press the injection button.
If insulin appears at the tip of the needle, the pen and needle are working correctly.
If no insulin appears at the needle tip, then step 3 can be repeated until insulin appears at the needle tip.
Stage 4. Dose selection
The dose can be set with an accuracy of 1 unit, from the minimum dose (1 unit) to the maximum (80 units). If it is necessary to administer a dose exceeding 80 units, 2 or more injections should be given.
The dosage window should show "0" after completion of the safety test. After this, the required dose can be set.
Stage 5. Dose administration
The patient should be informed about the injection technique by a healthcare professional.
The needle must be inserted under the skin.
The injection button must be pressed fully. It is held in this position for another 10 s until the needle is removed. This ensures that the selected dose of insulin is administered completely.
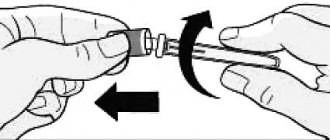
Stage 6: Removing and discarding the needle
In all cases, the needle should be removed and discarded after each injection. This prevents contamination and/or infection, air from entering the insulin container, and insulin leakage.
Special precautions must be taken when removing and discarding the needle. Recommended safety precautions for removing and disposing of needles (such as one-handed capping techniques) should be followed to reduce the risk of needle-related accidents and infection.
After removing the needle, you should close the SoloStar® syringe pen with the cap.
Side effects of the drug Lantus
Hypoglycemia is the most common complication of insulin treatment (especially when used in high doses). Severe hypoglycemia can lead to neurological impairment and pose a threat to the patient's life. The following side effects that were observed during clinical studies of the drug are presented by organ system in order of decreasing frequency of their manifestations (very often - 1/10; often - 1/100, but ≤1/10; rarely - 1/1000, but ≤ 1/100; very rarely - 1/10000, but ≤1/1000; sometimes - ≤1/10000) and decreasing significance. From the side of metabolism: very often - hypoglycemia. Severe hypoglycemia, especially repeated hypoglycemia, can lead to damage to the nervous system. Prolonged or severe hypoglycemia can be life-threatening. In many patients, symptoms of hypoglycemia are preceded by symptoms of adrenergic counterregulation (activation of the sympathoadrenal system in response to hypoglycemia); The more significant and rapid the decrease in plasma glucose levels, the more pronounced the symptoms of counterregulation. From the immune system: rarely - allergic reactions. Sometimes immediate allergic reactions to insulin develop. Such reactions to insulin (including insulin glargine) or to the components of the drug (generalized skin reactions, angioedema, bronchospasm, hypotension and shock) can threaten the patient's life. The use of insulin preparations can lead to the appearance of antibodies to it. Clinical studies have shown cross-formation of antibodies to human insulin and insulin glargine. The presence of antibodies to insulin may require dose adjustment. From the sensory organs: very rarely - dysgeusia. From the side of the organ of vision: rarely - visual impairment. A pronounced change in the level of sugar in the blood plasma can cause a temporary deterioration in vision due to a temporary change in turgor and refraction of the lens of the eye. Deterioration of vision is associated with refractive error. Rarely - retinopathy. Long-term improvement in glycemia reduces the risk of progression of diabetic retinopathy. Rapidly increasing the intensity of insulin therapy after previous unsuccessful glycemic control increases the risk of progression of diabetic retinopathy. In patients with proliferative retinopathy, especially those who have not undergone photocoagulation, severe hypoglycemic conditions can lead to amaurosis. From the skin and subcutaneous tissue: often - lipohypertrophy, rarely - lipoatrophy, which lead to a slowdown in local absorption of insulin. Constantly changing the injection site can reduce the severity of these phenomena or prevent them. It is possible to develop transient hyperemia of the skin at the injection site (in 3–4% of patients), which disappears during further treatment over a period of several days to several weeks. From the musculoskeletal system: very rarely - myalgia. General and local reactions: often - reactions at the injection site (hyperemia, pain, itching, urticaria, swelling or inflammation). Most local reactions usually resolve within a few days or weeks. In some cases, the prescription of insulin drugs leads to sodium and water retention in the body and the appearance of peripheral edema if previous glycemic control was not adequate.
Special instructions for the use of Lantus
Lantus is not the insulin of choice for the treatment of diabetic ketoacidosis. In such cases, intravenous administration of simple insulin is recommended. Before initiating dose adjustments in the event of insufficient control of plasma glucose levels or a tendency to episodes of hypoglycemia or hyperglycemia, it is necessary to check the patient's compliance with the proposed treatment regimen, the site of administration, the correct administration technique, and other important factors. Hypoglycemia. Due to the peculiarities of the pharmacokinetics of Lantus (a more constant supply of basal insulin), the development of hypoglycemia is more likely in the early morning hours than at night. With extreme caution and subject to constant glycemic control, the drug is used in those patients in whom hypoglycemia is particularly severe, for example in patients with severe stenosis of the coronary arteries or cerebral vessels (risk of severe cardiac or cerebral complications of hypoglycemia), as well as in patients with proliferative retinopathy that did not undergo photocoagulation (risk of transient amaurosis). Patient compliance with drug administration and nutrition, correct administration of insulin, and knowledge of the symptoms of hypoglycemia are important to reduce the risk of developing severe hypoglycemia. Risk factors for the development of hypoglycemia include: changing the injection site, increasing sensitivity to insulin (for example, after eliminating stress), intense or prolonged physical activity, concomitant diseases, vomiting, diarrhea, skipping meals, drinking alcohol, some uncompensated endocrine diseases (hypothyroidism, insufficiency functions of the pituitary gland or adrenal glands), simultaneous use of certain medications. In some conditions, symptoms that are precursors of hypoglycemia may change, lose their severity, or be absent altogether: a long history of diabetes mellitus, mental illness, autonomic neuropathy, the combined use of certain other drugs, switching from animal insulin to human insulin, as well as elderly patients or gradual development of hypoglycemia or with a marked improvement in glycemic control. In this case, it is possible to develop severe hypoglycemia (with possible loss of consciousness) even before the patient realizes the fact of hypoglycemia. If the level of glycosylated hemoglobin is normal or reduced, it is necessary to take into account the possibility of repeated, latent (especially at night) episodes of hypoglycemia. Accompanying illnesses . In the presence of concomitant disease, intensive monitoring of the patient's metabolism is necessary. In many cases, determination of ketones in urine is indicated; it is necessary to frequently adjust the insulin dose. The need for insulin often increases. Patients with type 1 diabetes mellitus should regularly consume carbohydrates, at least in small quantities, and also in case of vomiting, etc. You should never skip insulin injections completely. Impaired liver or kidney function. Due to insufficient experience, the effectiveness and safety of Lantus in patients with impaired liver function or moderate and/or severe renal impairment have not been established. In patients with impaired renal function, insulin requirements may decrease due to decreased insulin metabolism. In elderly patients, decreased renal function may lead to a persistent decrease in insulin requirements. In patients with severe liver dysfunction, insulin requirements may be reduced due to decreased gluconeogenesis and slower insulin metabolism. During pregnancy and breastfeeding . There is no clinical experience based on clinical studies of the use of insulin glargine during pregnancy. Preclinical studies did not reveal any direct teratogenic or embryotoxic effects on the course of pregnancy, as well as on childbirth and development in the postpartum period. Therefore, caution must be exercised when prescribing the drug. During pregnancy, including for patients with gestational diabetes, it is important to control glycemic levels. The need for insulin may be reduced in the first trimester of pregnancy and increased in the second and third trimesters. Immediately after birth, the need for insulin decreases rapidly (the risk of hypoglycemia increases), so it is important to carefully monitor plasma glucose levels. During breastfeeding, insulin dosage and diet adjustments are also required. Children. The effectiveness and safety of using Lantus in children has been proven only for use in the evening. Lantus is not used in children under the age of 6 years, since the effectiveness and safety of the drug in children of this age category have not been proven. The ability to influence reaction speed when driving vehicles and operating machinery. In the case of inadequate selection of the dose or replacement of the drug, as well as in the case of irregular administration or irregular food intake, excessive fluctuations in the level of glucose in the blood plasma are possible, primarily in the direction of hypoglycemia, which can negatively affect the ability to drive vehicles, especially in the initial stages. period of treatment, as well as while taking alcohol or drugs that act on the central nervous system.
Lantus SoloStar solution 100IU/ml-3ml N5 spray pen s/c
Method of administration and dosage Subcutaneously for adults and children over 6 years of age, Lantus® SoloStar® should be used only subcutaneously 1 time per day, always at the same time. Lantus® SoloStar® should be injected into the subcutaneous fat of the abdomen, shoulders or thighs. Injection sites should be alternated with each new injection within the recommended areas for subcutaneous administration of the drug.
The dose of Lantus® SoloStar® and the time of day for its administration are selected individually. In patients with type 2 diabetes mellitus, Lantus® SoloStar® can be used both as monotherapy and in combination with other hypoglycemic drugs.
Switching from treatment with other hypoglycemic drugs to Lantus® SoloStar® When replacing a treatment regimen with intermediate-acting or long-acting insulins with a treatment regimen with Lantus® SoloStar®, it may be necessary to adjust the daily dose of basal insulin, and there may also be a need to change concomitant antidiabetic therapy (doses and administration regimens of additionally used short-acting insulins or their analogues or doses of oral hypoglycemic drugs).
When transferring patients from twice daily administration of isophane insulin to a single administration of Lantus® SoloStar® in order to reduce the risk of hypoglycemia at night and early morning, the daily dose of basal insulin should be reduced by 20-30% in the first weeks of treatment. During this period, the dose reduction, at least in part, should be compensated by increasing the doses of short-acting insulin, followed by individual adjustment of the dosage regimen.
Lantus® SoloStar® should not be mixed with other insulin preparations or diluted. It is necessary to ensure that the syringes do not contain residues of other medications. Mixing or diluting may change the time profile of insulin glargine. Mixing with other insulins may cause precipitation.
As with the use of other human insulin analogues, in patients receiving high doses of insulin, due to the presence of antibodies to human insulin, when switching to Lantus® SoloStar®, an increase in the response to insulin administration may be observed. During the transition to Lantus® SoloStar® and in the first weeks after it, careful monitoring of blood glucose levels and, if necessary, correction of the insulin dosage regimen are required.
If metabolic regulation improves and the resulting increase in tissue sensitivity to insulin may require further adjustment of the dosage regimen. Dose adjustment may also be required, for example, if there is a change in the patient’s body weight, lifestyle, time of day for drug administration, or if other circumstances arise that increase the susceptibility to the development of hypo- or hyperglycemia.
The drug should not be administered intravenously. Intravenous administration of the usual dose intended for subcutaneous administration may cause severe hypoglycemia.
The duration of action of the drug Lantus® SoloStar® depends on the localization of the site of its subcutaneous administration.
Lantus drug interactions
Hypoglycemia may develop with simultaneous use of Lantus with oral hypoglycemic agents, ACE inhibitors, disopyramide, fibrates, fluoxetine, MAO inhibitors, pentoxifylline, propoxyphene, salicylates and sulfonamides. The effectiveness of Lantus can be reduced by GCS, danazol, diazoxide, glucagon, isoniazid, estrogens and progesterone, phenothiazine derivatives, somatropin, sympathomimetics (epinephrine, salbutamol, terbutaline), thyroid hormones, atypical antipsychotics (clozapine, olanzapine), protease inhibitors. β-adrenergic blockers, clonidine, lithium salts, pentamidine or alcohol can potentiate or weaken the hypoglycemic effect of insulin. When used simultaneously with insulin, β-adrenergic receptor blockers, clonidine, guanethidine, and reserpine, their effects can significantly decrease or disappear, as well as weaken the symptoms of adrenergic counterregulation. Lantus cannot be mixed with other drugs. The syringe for administering Lantus should not contain trace amounts of other drugs.