Pharmacological properties of the drug Byeta
Exenatide is an incretin mimetic that enhances several of the antihyperglycemic effects of glucagon-like peptide-1. The amino acid sequence of exenatide is similar to that of human glucagon-like peptide-1. Exenatide has the ability to bind to and activate glucagon-like peptide-1 receptors in humans through cAMP and/or other intracellular signaling pathways. Exenatide enhances glucose-dependent insulin secretion from pancreatic β-cells. When blood glucose concentrations decrease, insulin secretion decreases. Exenatide inhibits excessive glucagon secretion during periods of hyperglycemia in patients with type II diabetes. However, exenatide does not increase the normal glucagon response and other hormone responses to hypoglycemia. Exenatide slows down gastric emptying. The administration of exenatide leads to a decrease in appetite. In patients with type II diabetes, therapy with exenatide in combination with metformin and/or sulfonylureas leads to a decrease in fasting blood glucose, postprandial blood glucose, and glycosylated hemoglobin (Hb1c), thereby improving glycemic control in these patients. After subcutaneous administration to patients with type II diabetes, exenatide is rapidly absorbed and reaches the mean maximum concentration in blood plasma after 2 hours. The mean maximum concentration of exenatide in blood plasma was 211 pg/ml, and AUC was 1036 pg h/ml after sc. administration of 10 mcg exenatide. AUC increases in proportion to the fluctuation of the therapeutic dose from 5 to 10 mcg, while a proportional increase in the maximum concentration in the blood plasma was not observed. The same effects are achieved with subcutaneous injection into the abdomen, thigh or shoulder. The average volume of distribution of exenatide after subcutaneous administration of a single dose is 28 L. Exenatide is eliminated primarily by glomerular filtration followed by proteolytic degradation. The average clearance of exenatide in humans is 9 L/h, and the average terminal half-life is 2.4 hours. These pharmacokinetic characteristics of exenatide are independent of dose. Gender and race do not affect the pharmacokinetics of exenatide. In patients with mild or moderate renal impairment, the clearance of exenatide was only slightly reduced. Clearance was significantly reduced (up to 84%) in patients with end-stage renal disease who were on dialysis.
Byeta - pathophysiological approach in the treatment of type 2 diabetes mellitus
The regulation of glucose homeostasis in the body is carried out by a complex multihormonal system, including pancreatic hormones and incretin hormones produced in the intestines in response to food intake.
Figure 1. Schematic illustration of the incretin effect. Oral glucose loading produces a much greater insulin response than intravenous glucose, which produces an identical plasma glucose profile.
Figure 2. Reduced incretin effect in patients with type 2 diabetes.
Figure 3. Exenatide and GLP-1 have similar degrees of ability to bind to GLP-1 receptors in vitro
Figure 4. Byeta improves the sensitivity of beta cells in patients with type 2 diabetes.
Figure 5. Weight loss with Byeta treatment
Figure 6. Similar reduction in HbA1c in the byeta and insulin glargine groups
Figure 7. Progressive weight loss with Byata treatment
It has been shown that after oral administration of glucose, a more pronounced increase in insulin secretion is observed compared to that observed after intravenous infusion of glucose, accompanied by an identical increase in glycemic levels. This effect, called the “incretin effect,” indicates the great importance of gastrointestinal signals in the hormonal regulation of glucose homeostasis (Figure 1).
Incretins belong to a family of hormones that stimulate insulin secretion in response to food intake. Up to 70% of postprandial insulin secretion in healthy people is due to the effect of incretins, which is significantly reduced in patients with type 2 diabetes and IGT.
The two most important incretin hormones are:
- glucose-dependent insulinotropic polypeptide (GIP), formerly known as gastric inhibitory polypeptide;
- glucagon like peptide (GLP-1).
Glucose-dependent
insulinotropic hormone (GIP)
GIP belongs to the glucagon-secretin family of peptides. GIP is secreted by K cells, with the highest density in the duodenum, but they are found in the mucosa of the entire small intestine. Secretion of the polypeptide is stimulated by ingested carbohydrates and fats. Usually there is a 10-20-fold increase in its plasma concentration in response to food intake.
Glucagon
-like peptide (GLP-1)
In healthy people, GLP-1 is one of the most potent stimulators of insulin secretion.
GLP-1 belongs to the glucagon-secretin superfamily of peptide hormones, which share an amino acid sequence similarity with the glucagon molecule, ranging from 21% to 48%. Although these peptides are derived from the same precursor, proglucagon, they differ significantly in their effects on essential metabolic processes. In L-cells, which are mainly located in the distal part of the gastrointestinal tract - the ileum and colon, proglucagon is cleaved not with the formation of glucagon, as in β-cells, but with the cleavage of two glucagon-like peptides from the C-terminus. These peptides, GLP-1 and GLP-2, are characterized by almost 50% homology in amino acid sequence with glucagon.
GLP-1 has a short half-life of only 60-90 seconds.
Its rapid inactivation, with the formation of inactive metabolites, occurs under the influence of dipeptidyl peptidase ΙV (DPP-IV).
Secretion of GLP-1 by the distal GI tract is controlled by neural and endocrine signals that are initiated both by the entry of food into the proximal GI tract and by direct exposure of L cells to dietary nutrients. Associated with this is the two-phase mechanism of GLP-1 secretion. The first phase of secretion (15-30 min.) is the phase of early release of GLP-1 under the combined influence of hormonal and nervous factors, the second late phase of secretion (30-60 min.) is the phase that is initiated by direct contact of food nutrients with L- cells.
Physiological
effects of GLP-1
The physiological effects of GLP-1 are realized after its interaction with specific receptors that are expressed in many organs and tissues, including the pancreas, stomach, small intestine, brain, pituitary gland, lungs, kidneys, heart. The main target organ for GLP-1 is the islets of Langerhans. The insulinotropic activity of GLP-1, which clearly depends on the level of glycemia, is realized through the interaction of GLP-1 with specific receptors located on the β-cell membrane. It should be noted that GLP-1 activates the glucokinase gene and the gene encoding the glucose transporter GLUT 2, which are responsible for the intracellular mechanism of insulin secretion.
Infusion of GLP-1 causes a decrease in blood glucose concentrations to fasting blood glucose levels. As soon as the glycemic level decreases and approaches normal values, the effect of GLP-1 on insulin secretion ceases.
Thus, a clinically important consequence of the dependence of the effects of GLP-1 on blood glucose levels is that GLP-1 cannot cause significant hypoglycemia. The action of GLP-1 promotes an adequate secretory response of β-cells in response to glucose. This important property of GLP-1 may improve the glucose sensing capacity of β-cells and their secretory response to glucose in patients with IGT. There is an inverse relationship between dietary GLP-1 secretion and increased insulin resistance.
Another important physiological effect of GLP-1 is its effect on glucagon secretion. GLP-1, through a glucose-dependent mechanism, suppresses glucagon secretion by pancreatic α-cells.
Thus, GLP-1 regulates plasma glucose concentrations primarily by modulating the secretion of both insulin and glucagon, that is, it is required for both normal glucose tolerance and adequate postprandial insulin secretion.
Recent studies have revealed the following effects of GLP-1:
- potentiates glucose-dependent insulin secretion;
- enhances insulin biosynthesis;
- increases insulin gene expression;
- increases the expression of genes important for the function of beta cells glucokinase, Glut 2, etc.);
- has a mitotic effect on beta cells and promotes the differentiation of ductal progenitor cells;
- suppresses beta cell apoptosis;
- suppresses glucagon secretion.
It is well known that the distal part of the small intestine takes part in the regulation of the stomach. GLP-1 controls the rate of gastric emptying by binding to receptors in the brain and stimulating the parasympathetic nerves. This slows gastric emptying and reduces gastric (stimulated by pentagastrin and food stimuli) and pancreatic secretions. Slowing gastric emptying by GLP-1 is promising in terms of such an aspect of the treatment of type 2 diabetes as reducing glucose excursion in the postprandial period.
Apparently, the most unexpected effect of GLP-1 is its suppression of food and water absorption. Recent evidence suggests that GLP-1 is a potent anorexigenic hormone, similar in action to leptin, and an antagonist of orexigenic hormones such as neuropeptide Y and corticoliberin. GLP-1 is involved in the processes of regulation of eating behavior, acting through central mechanisms, and contributes to the development of a feeling of satiety.
The β-cytotrophic effects of GLP-1, which have been identified in animals, are extremely important clinically. in vitro and in vivo studies
animal models have shown the cytoprotective effect of GLP-1, including an increase in the mass of β-cells, stimulation of islet neogenesis, and increased differentiation of new β-cells from precursor cells of the pancreatic duct epithelium. In addition, GLP-1 promotes the transformation of non-insulin-producing cells into insulin-secreting cells. The normal number of β-cells is maintained by a balance between proliferation and apoptosis. Recently, it was shown that one of the mechanisms for increasing β-cell mass is due to the antiapoptotic effect of GLP-1.
In type 2 diabetes, the impaired “incretin effect” is one of the pathophysiological mechanisms leading to inadequate insulin secretion. When testing with oral and intravenous glucose loading, in patients with type 2 diabetes, the “incretin effect” was almost completely absent or was significantly reduced. It is therefore likely that insufficient incretin function plays a significant role in the pathogenesis of the disease.
The mechanisms underlying the decrease in incretin effect in type 2 diabetes are different. Theoretically, an incretin defect may occur due to impaired secretion or accelerated metabolism of hormones or decreased sensitivity to them.
Studies have found in patients with type 2 diabetes, in response to food intake, a very significant impairment in GLP-1 secretion.
Administration of exogenous GLP-1 restores the normal insulin response to glucose in patients with type 2 diabetes. It is critical to note that the physiological effects of GLP-1 include effects on virtually all well-known pathophysiological disorders in type 2 diabetes, namely, β-cell dysfunction, reduced “incretin effect”; hypersecretion of glucagon, accelerated gastric emptying; increased appetite and excess body weight; progressive decrease in β-cell mass.
Incretins in the treatment of type 2 diabetes mellitus
Available data indicating incretin deficiency in type 2 diabetes provide grounds for considering endocrine-enhancing drugs as a new therapeutic principle in the treatment of diabetes. A recent study demonstrated that administration of GLP-1 to patients with type 2 diabetes can completely normalize their β-cell sensitivity to glucose, as well as partially restore the lost first phase of insulin secretion and completely restore the second phase of insulin secretion under hyperglycemic “clamp” conditions. test.
Currently, new therapeutic approaches in the treatment of type 2 diabetes are associated with modulation of the activity and level of GLP-1 through the administration of GLP-1 analogues and mimetics (exenatide, liraglutide, CJC-1131). Exenatide (Bayeta)
– GLP-1 mimetic, a synthetic form of the reptile hormone exentid-4 (Figure 3), is the most studied drug from this group (5, 6).
Exentid-4 is a peptide isolated from the salivary glands of the Gila monster lizard (Heloderma suspectum),
which has 53% homology with human GLP-1. Unlike GLP-1, the drug is resistant to DPP-IV due to the peculiarities of the amino acid sequence (glycine in the 2nd position) (10, 11, 12).
In various clinical studies, Byeta's effects have been shown to be independent of the duration and severity of diabetes mellitus (3, 6). Subcutaneous administration of Byeta is accompanied by the achievement of metabolic control and an increase in insulin sensitivity (Figure 4), a decrease in appetite, a decrease in body weight, and a decrease in glucagon and FFA levels (2, 4, 5).
In a recent study in patients with type 2 diabetes, in the group of patients receiving SC 10 mcg of Byeta, a decrease in HbA1c levels was obtained by 0.9% and by 0.6% in those receiving 5 mcg of Byeta. An HbA1c level of less than 7% was achieved in 34.2% of patients receiving 10 mcg of Byeta and in 26.7% of patients receiving 5 mcg of Byeta. In addition, in the group of patients receiving 10 mcg of Byeta, at week 30 of therapy there was a significant decrease in weight by 1.9 kg (Figure 5).
A 26-week study compared the clinical effectiveness of Byeta and insulin glargine (10). The study involved 551 patients with type 2 diabetes and poor glycemic control.
After 26 weeks, all patients showed an improvement in glycemic control, with a similar decrease in HbA1c in both the Byeta and insulin glargine groups (Figure 6).
At the same time, an additional positive effect of treatment with Byeta was a decrease in the patients’ body weight, while during treatment with insulin glargine, the patients gained weight (Figure 7).
Fasting hypoglycemia occurred significantly less frequently in patients receiving Byeta therapy.
Inappropriately elevated glucagon levels, both fasting and postprandial, are characteristic of patients with type 2 diabetes (1, 8, 10). In Kolterman's studies, a decrease in glucagon levels was demonstrated during exenatide therapy, which is a significant advantage of Byeta compared to other glucose-lowering drugs (9). The main undesirable effect is mild or moderate nausea, which goes away after one or two weeks and does not cause significant discomfort.
Thus, Bayeta (Exenatide) opens a new era in the treatment of type 2 diabetes mellitus, which can safely be called pathophysiologically based. The ease of use of the drug, effectiveness in reducing both fasting and postprandial glycemia, glycated hemoglobin and progressive weight loss distinguish Byeta from existing antidiabetic drugs.
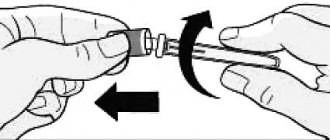
Use of the drug Byeta
Exenatide therapy should begin with a dose of 5 mcg, which is prescribed 2 times a day for a period of at least 1 month to improve tolerability. 1 month after the start of treatment, the dose of exenatide can be increased to 10 mcg 2 times a day to further improve glycemic control. Doses above 10 mcg are not recommended. Exenatide is taken at any time for 60 minutes before a morning or evening meal or before two main meals during the day, between which there is a 6-hour or greater period of time. Exenatide should not be given after meals. If an injection is missed, the next scheduled dose should be administered. Exenatide is prescribed as a subcutaneous injection into the thigh, abdomen or shoulder. If exenatide is added to sulfonylurea therapy, the dose of the latter may be reduced to prevent the risk of hypoglycemia. When exenatide is added to metformin therapy, the metformin dose may remain unchanged since the need for metformin dose adjustment due to hypoglycemia when used with exenatide is unlikely. When used daily, the dosage of exenatide does not need to be adjusted based on self-monitoring of glycemia. However, self-monitoring of blood glucose may be necessary to adjust the dose of sulfonylureas. Exenatide is prescribed with caution and with a gradual increase in dose from 5 to 10 mcg in patients over 70 years of age. Clinical data in patients over 75 years of age are limited. Patients with mild renal (creatinine clearance 50–80 ml/min) or hepatic impairment do not require exenatide dose adjustment. Patients with moderate renal impairment (creatinine clearance 30–50 ml/min) require a gradual increase in dose from 5 to 10 mcg. Exenatide is not recommended for use in patients with end-stage renal disease or severe renal impairment (creatinine clearance ≤30 mL/min). Patients with liver failure do not require dose adjustment. Exenatide has not been studied in patients under 18 years of age.
Side effects of the drug Byeta
very often (≥10%) - diarrhea, nausea, vomiting, hypoglycemia (in combination with sulfonylurea derivatives or metformin and sulfonylurea derivatives). Often (≥1% and ≤10%) - dyspepsia, gastroesophageal reflux, asthenia, tremors, loss of appetite, dizziness, headache, hyperhidrosis. Since the release of exenatide on the market, reports of the following side effects have been received: from the gastrointestinal tract : abdominal pain, belching, constipation, flatulence (infrequently), acute pancreatitis (rarely); local : reactions at the injection site (often); from the immune system : anaphylactic reaction (very rare); studies : increased international normalized ratio with concomitant use of warfarin, several reports of bleeding; metabolic and nutritional disorders : dehydration (rare) associated with nausea, vomiting and/or diarrhea; from the nervous system : dysgeusia (infrequently), drowsiness; from the skin and appendages : generalized itching and/or urticaria, macular or papular rashes, angioedema (rare); from the genitourinary system : changes in renal parameters, including acute renal failure, worsening of chronic renal failure, increased serum creatinine (rarely); immunogenicity : due to the potential immunogenic properties of the protein and peptide components in the drug, patients may develop antibodies to exenatide as a result of treatment with exenatide. In most patients who developed antibodies, antibody titers decreased over time.
Buy Byeta solution subcutaneously 250 µg/ml 1.2 ml in pharmacies
Bayeta Buy Bayeta in pharmacies DOSAGE FORMS solution for subcutaneous injection 250 µg/ml
MANUFACTURERS Baxter Pharmaceutical Solutions LL C packaged Lilly Pharma Fertigung und Distribution GmbH & Co. Kg (United States of America) Eli Lilly & Company (Germany) Eli Lilly & Company packaged Lilly Pharma Fertigung und Distribution GmbH & Co (United States of America)
GROUP Additional antidiabetic agents
COMPOSITION Active substance: Exenatide.
INTERNATIONAL NON-PROPENTED NAME Exenatide
PHARMACOLOGICAL ACTION Exenatide is a 39-amino acid amidopeptide that is a potent incretin mimetic. It causes increased glucose-dependent insulin secretion and has other hypoglycemic effects inherent in incretins, which improves glycemic control in patients with type 2 diabetes mellitus. In hyperglycemic conditions, exenatide enhances glucose-dependent insulin secretion from pancreatic beta cells. This insulin secretion ceases as blood glucose concentrations decrease and approach normal levels, thereby reducing the potential risk of hypoglycemia. In patients with type 2 diabetes mellitus due to hyperglycemia, administration of exenatide suppresses excess glucagon secretion. However, exenatide does not interfere with the normal glucagon response to hypoglycemia. The administration of exenatide leads to a decrease in appetite. In patients with type 2 diabetes mellitus, therapy with exenatide in combination with metformin and/or sulfonylureas leads to a decrease in fasting blood glucose, postprandial blood glucose, and HbAic, thereby improving glycemic control in these patients. Following subcutaneous administration to patients with type 2 diabetes mellitus, exenatide is rapidly absorbed and reaches mean maximum plasma concentrations in 2.1 hours. Exenatide is primarily eliminated by glomerular filtration followed by proteolytic degradation. The terminal half-life is 2.4 hours. These pharmacokinetic characteristics of exenatide are independent of dose. Measurable concentrations of exenatide are determined for approximately 10 hours after dosing.
INDICATIONS FOR USE Type 2 diabetes mellitus as an add-on therapy to metformin, sulfonylureas or a combination of metformin and sulfonylureas to improve glycemic control.
CONTRAINDICATIONS • Hypersensitivity to exenatide or excipients included in the drug. • Type 1 diabetes mellitus or the presence of diabetic ketoacidosis. • Severe renal failure (creatinine clearance
SIDE EFFECTS Very often - nausea, vomiting, diarrhea, hypoglycemia (in combination with metformin and sulfonylurea derivatives). Often - dyspepsia, a feeling of trembling, dizziness, headache, loss of appetite, weakness, gastroesophageal reflux, hyperhidrosis, skin reaction at the injection site. Sometimes - abdominal pain, bloating, belching, constipation, impaired taste, flatulence; Rarely - drowsiness, rash, itching, dehydration (associated with nausea, vomiting and/or diarrhea), angioedema. Extremely rare - anaphylactic reaction. Since the incidence of hypoglycemia increases when BAETA is co-administered with sulfonylureas, it is necessary to consider reducing the dose of sulfonylureas if the risk of hypoglycemia increases.
INTERACTIONS BYETA should be used with caution in patients taking oral medications that require rapid absorption from the gastrointestinal tract, as BYETA may cause delayed gastric emptying. Co-administration of the drug BAETA with HMG-CoA reductase inhibitors was not accompanied by changes in lipid composition (HDL-cholesterol, LDL-cholesterol, total cholesterol and triglycerides).
METHOD OF ADMINISTRATION AND DOSAGE The drug BYETA is injected subcutaneously into the thigh, abdomen or forearm. The starting dose is 5 mcg, administered twice daily at any time within a 60-minute period before morning and evening meals. The drug should not be administered after meals. If an injection of the drug is missed, treatment continues without changing the dose. 1 month after the start of treatment, the dose of BAYETA can be increased to 10 mcg twice a day. When BAETA is co-administered with metformin, sulfonylureas, or a combination of these two drugs, the initial dose of metformin or sulfonylureas does not change.
OVERDOSE In case of overdose (dose 10 times higher than the maximum recommended dose), the following symptoms were observed: severe nausea and vomiting, as well as a rapid decrease in blood glucose concentrations (hypoglycemia). Treatment: symptomatic, including parenteral glucose administration in case of severe hypoglycemia
SPECIAL INSTRUCTIONS The drug BYETA should not be administered after meals. Intravenous or intramuscular administration of the drug is not recommended. BAETA should not be used if particles are found in the solution, or if the solution is cloudy or colored. During therapy with BAETA, antibodies to exenatide may appear. However, this does not affect the frequency and types of side effects reported. Patients should be informed that treatment with BAETA may result in decreased appetite and/or weight loss and that no dosage modification is necessary due to these effects.
STORAGE CONDITIONS List B. At a temperature of 2-8°C. Store the drug in use in a syringe pen at a temperature of 2-8°C for no more than 30 days. Do not freeze. Protect from exposure to light. Keep out of the reach of children.
Special instructions for the use of the drug Byeta
Special Precautions for Use Exenatide should not be used in patients with type 1 diabetes or for the treatment of diabetic ketoacidosis. Exenatide is not recommended for use in patients with end-stage renal disease or severe renal impairment (creatinine clearance ≤30 mL/min). In patients with end-stage renal disease on dialysis, single doses of exenatide 5 mcg were poorly tolerated due to gastrointestinal side effects. The effect of exenatide has not been studied in patients with severe gastrointestinal diseases, including gastroparesis. Exenatide use is commonly associated with gastrointestinal side effects, including nausea, vomiting, and diarrhea. Therefore, the use of exenatide is not recommended for patients with severe gastrointestinal diseases. The combined use of exenatide with insulin, D-phenylalanine derivatives, meglitinides or alpha-glucosidase inhibitors has not been studied. Isolated cases of changes in renal parameters have been reported, including an increase in serum creatinine, worsening of chronic renal failure and acute renal failure, which sometimes required dialysis. Some of these cases were observed in patients receiving one or more drugs that affect renal function/hydration and/or in patients whose condition could lead to dehydration (nausea, vomiting, diarrhea). This is a concomitant prescription of drugs such as ACE inhibitors, NSAIDs and diuretics. Reversible changes in renal parameters were identified by initiating maintenance therapy and stopping the use of drugs that could potentially cause these events, including exenatide. Isolated cases of acute pancreatitis have been reported. The development of pancreatitis was noted when maintenance therapy was prescribed. The drug contains metacresol, which can cause allergic reactions. Several cases of increased international normalized ratio have been reported with concomitant use of warfarin and exenatide, sometimes in combination with bleeding. Hypoglycemia : When using exenatide in combination with metformin, there was no increase in the incidence of hypoglycemia compared with that when using placebo in combination with metformin. In contrast, the incidence of hypoglycemia was increased when exenatide was combined with a sulfonylurea compared with that when a sulfonylurea was used in combination with placebo. To prevent the risk of hypoglycemia associated with the use of sulfonylureas, the dose of the latter may be reduced. Exenatide did not alter the contrainsular hormone response to insulin-induced hypoglycemia in a study of healthy subjects. Exenatide is a clear, colorless liquid and should not be used if impurities are present or if the solution is colored or cloudy. Exenatide should not be prescribed during pregnancy; it is recommended to use insulin. If a woman becomes pregnant or becomes pregnant, exenatide should be discontinued. It is unknown whether exenatide is excreted in human milk, so the use of exenatide is not recommended during breastfeeding. When using exenatide in combination with a sulfonylurea, patients should be advised to take measures to prevent hypoglycemia when driving or operating complex machinery. If side effects from the central nervous system occur, you should not drive a car or operate precision machinery.
Byeta syringe pen solution for subcutaneous administration 250 µg/ml 1.2 ml/dose 60 doses
Description:
Compound
- 1 ml contains exenatide 250 mcg;
- Excipients: sodium acetate trihydrate 1.59 mg, acetic acid 1.1 mg, mannitol 43 mg, metacresol 2.2 mg, water for injection (qs up to 1 ml).
pharmachologic effect
Byeta is a hypoglycemic drug. Exenatide (exendin-4) is an incretin mimetic and is a 39-amino acid amidopeptide. Incretins, such as glucagon-like peptide-1 (GLP-1), enhance glucose-dependent insulin secretion, improve β-cell function, suppress inappropriately increased glucagon secretion, and slow gastric emptying after they enter the general circulation from the intestine. Exenatide is a potent incretin mimetic that enhances glucose-dependent insulin secretion and has other hypoglycemic effects associated with incretins, thereby improving glycemic control in patients with type 2 diabetes mellitus.
The amino acid sequence of exenatide partially corresponds to the sequence of human GLP-1, as a result of which it binds and activates GLP-1 receptors in humans, which leads to increased glucose-dependent synthesis and secretion of insulin from pancreatic β-cells with the participation of cyclic AMP and/or other intracellular signaling ways. Exenatide stimulates the release of insulin from β-cells in the presence of elevated glucose concentrations.
The chemical structure and pharmacological action of exenatide differs from insulin, sulfonylurea derivatives, D-phenylalanine derivatives and meglitinides, biguanides, thiazolidinediones and alpha-glucosidase inhibitors.
Exenatide improves glycemic control in patients with type 2 diabetes mellitus through the following mechanisms.
In hyperglycemic conditions, exenatide enhances glucose-dependent insulin secretion from pancreatic β-cells. This insulin secretion ceases as blood glucose concentrations decrease and approach normal levels, thereby reducing the potential risk of hypoglycemia.
Insulin secretion during the first 10 minutes (in response to increased glycemia), known as the “first phase insulin response,” is specifically absent in patients with type 2 diabetes. In addition, loss of the first phase of insulin response is an early impairment of β-cell function in type 2 diabetes. Administration of exenatide restores or significantly enhances both the first and second phase insulin response in patients with type 2 diabetes mellitus.
In patients with type 2 diabetes mellitus due to hyperglycemia, administration of exenatide suppresses excess glucagon secretion. However, exenatide does not interfere with the normal glucagon response to hypoglycemia.
Administration of exenatide has been shown to result in decreased appetite and reduced food intake; suppresses gastric motility, which leads to slower emptying.
In patients with type 2 diabetes mellitus, therapy with exenatide in combination with metformin, thiazolidinedione and/or sulfonylureas leads to a decrease in fasting blood glucose, postprandial blood glucose, and HbA1c, thereby improving glycemic control in these patients.
Byeta, indications for use
Monotherapy
- type 2 diabetes mellitus as monotherapy in addition to diet and exercise to achieve adequate glycemic control.
Combination therapy
- Type 2 diabetes mellitus as adjunctive therapy to metformin, a sulfonylurea, a thiazolidinedione, a combination of metformin and a sulfonylurea, or metformin and a thiazoldinedione when adequate glycemic control is not achieved.
Contraindications
- Type 1 diabetes mellitus or the presence of diabetic ketoacidosis.
- Severe renal failure (creatinine clearance less than 30 ml/min).
- The presence of severe gastrointestinal diseases with concomitant gastroparesis.
- Pregnancy.
- Lactation period (breastfeeding).
- Children under 18 years of age (the safety and effectiveness of the drug in children has not been established).
- Hypersensitivity to exenatide or excipients included in the drug.
Directions for use and doses
S/C, in the area of the thigh, abdomen or forearm.
The initial dose is 5 mcg, which is administered 2 times / day at any time during the 60-minute period before the morning and evening meals. The drug should not be administered after meals. If an injection of the drug is missed, treatment continues without changing the dose.
1 month after the start of treatment, the dose of the drug can be increased to 10 mcg 2 times a day.
When co-administered with metformin, thiazolidinedione, or a combination of these drugs, the original dose of metformin and/or thiazolidinedione may not be changed. When Byeta is combined with a sulfonylurea, it may be necessary to reduce the dose of the sulfonylurea to reduce the risk of hypoglycemia.
Use during pregnancy and breastfeeding
The drug is contraindicated during pregnancy and breastfeeding.
Side effects
Adverse reactions that occurred more often than in isolated cases are listed according to the following gradation: very often - ≥10%, often - ≥1%, but
From the digestive system: very often - nausea, vomiting, diarrhea; often - loss of appetite, dyspepsia, gastroesophageal reflux; sometimes - abdominal pain, bloating, belching, constipation, impaired taste, flatulence.
From the side of the central nervous system: often - dizziness, headache; rarely - drowsiness.
From the endocrine system: very often - hypoglycemia (in combination with sulfonylurea derivatives); often - a feeling of trembling, weakness, hyperhidrosis.
Allergic reactions: rarely - rash, itching, angioedema; extremely rarely - anaphylactic reaction.
Other: often - skin reaction at the injection site; rarely - dehydration (associated with nausea, vomiting and/or diarrhea). Several cases of increased clotting time (INR) have been reported with concomitant use of warfarin and exenatide, sometimes accompanied by bleeding.
Due to the fact that the incidence of hypoglycemia increases when Byeta is co-administered with sulfonylurea derivatives, it is necessary to consider reducing the dose of sulfonylurea derivatives when the risk of hypoglycemia increases. Most episodes of hypoglycemia were mild or moderate in intensity and were relieved by oral carbohydrate intake.
In general, side effects were mild or moderate in intensity and did not lead to treatment discontinuation. Most commonly, mild to moderate nausea reported was dose-related and decreased over time without interfering with daily activities.
special instructions
The drug should not be administered after meals.
IV or IM administration of the drug is not recommended.
Byeta ® should not be used if particles are found in the solution or if the solution is cloudy or colored.
Due to the potential immunogenicity of drugs containing proteins and peptides, the development of antibodies to exenatide is possible during therapy with Byeta ®. In most patients who produced such antibodies, their titer decreased as therapy continued and remained low for 82 weeks. The presence of antibodies does not affect the frequency and types of side effects reported.
Patients should be informed that treatment with Byeta ® may result in a decrease in appetite and/or body weight, and that due to these effects there is no need to change the dosage regimen.
Preclinical studies in mice and rats did not reveal the carcinogenic effect of exenatide. When administered to rats at a dose 128 times higher than the human dose, a numerical increase in C-cell adenomas of the thyroid gland without any signs of malignancy was noted, which was associated with an increase in the life expectancy of experimental animals receiving exenatide.
Rare cases of renal dysfunction have been reported, including an increase in serum creatinine, the development of renal failure, and aggravation of chronic and acute renal failure; in this case, hemodialysis was sometimes required. Some of these events were observed in patients receiving one or more pharmacological drugs that affect renal function/fluid metabolism and/or in the presence of other adverse events that contribute to impaired hydration, such as nausea, vomiting and/or diarrhea. Concomitant medications included ACE inhibitors, NSAIDs, and diuretics. When symptomatic therapy was prescribed and the drug that was presumably the cause of the pathological changes was discontinued, impaired renal function was restored. During preclinical and clinical studies of exenatide, no data indicating its direct nephrotoxicity were found.
Rare cases of acute pancreatitis have been reported while taking Byeta ® . Patients should be informed of the characteristic symptoms of acute pancreatitis: persistent severe abdominal pain. When symptomatic therapy was prescribed, resolution of acute pancreatitis was observed.
Before starting treatment with Byeta ®, patients should read the “Guide for using a syringe pen” attached to the drug.
Drug interactions
Byeta should be used with caution in patients taking oral medications that require rapid absorption from the gastrointestinal tract, as Byeta may cause delayed gastric emptying.
Patients should be advised to take oral drugs whose effects depend on their threshold concentration (for example, antibiotics) at least 1 hour before exenatide administration. If such drugs must be taken with food, they should be taken with meals when exenatide is not administered.
With the simultaneous administration of digoxin (0.25 mg 1 time / day) with the drug Byeta, Cmax of digoxin is reduced by 17%, and Tmax increases by 2.5 hours. However, the overall pharmacokinetic effect at steady state does not change.
During the administration of the drug Byeta, AUC and Cmax of lovastatin decreased by approximately 40% and 28%, respectively, and Tmax increased by approximately 4 hours. Co-administration of the drug Byeta with HMG-CoA reductase inhibitors was not accompanied by changes in blood lipid composition (HDL-cholesterol , LDL cholesterol, total cholesterol and triglycerides).
In patients with mild or moderate arterial hypertension stabilized by lisinopril (5-20 mg/day), Byeta did not change the AUC and Cmax of lisinopril at steady state. T maxlisinopril at steady state increased by 2 hours. There were no changes in average daily systolic and diastolic blood pressure.
The use of Byeta in combination with insulin, thiazolidinediones, D-phenylalanine derivatives, meglitinides or alpha-glucosidase inhibitors has not been studied.
Overdose
Symptoms: severe nausea and vomiting, as well as rapid development of hypoglycemia (when taking a dose 10 times higher than the maximum recommended).
Treatment: carry out symptomatic therapy, including parenteral administration of glucose in case of severe hypoglycemia.
Release form
Solution for subcutaneous administration.
Package
per package 1 syringe pen 1.2 and 2.4 ml
Storage conditions
In a place protected from light, at a temperature of 2–8 °C (do not freeze).
Best before date
2 years. The drug in use in a syringe pen should be stored at a temperature not exceeding 25°C for no more than 30 days.
Byeta drug interactions
The retarding effect of exenatide on gastric emptying may reduce the extent and rate of absorption of drugs administered orally. Exenatide should be prescribed with caution to patients receiving medications that require rapid absorption from the gastrointestinal tract. When taking drugs whose effectiveness is dependent on cutoff concentrations, such as contraceptives and antibiotics, patients should be advised to take these drugs at least 1 hour before exenatide administration. If these drugs are prescribed with food, patients should be advised to take them with a meal or snack when not taking exenatide. The AUC and maximum plasma concentration of lovastatin were decreased by approximately 40 and 28%, respectively, and the maximum half-life was prolonged by 4 hours when exenatide (10 mcg) was administered concomitantly with a single dose of lovastatin (40 mg) compared with lovastatin alone. Concomitant use of exenatide and HMG-CoA reductase inhibitors was not associated with significant changes in the lipid profile. In a study among healthy volunteers, a 2-hour prolongation of the maximum half-life of warfarin, digoxin, and lisinopril was noted when these drugs were administered 30 minutes after exenatide. No clinically significant effects on maximum plasma concentration or AUC were identified. However, there have been reports of increased international normalized ratio during combined use of warfarin and exenatide, so international normalized ratio should be monitored. Exenatide does not affect the pharmacokinetics of metformin and sulfonylurea derivatives. Proton pump inhibitors should be administered 1 hour before exenatide or 4 hours after exenatide injection. The AUC, maximum plasma concentration and maximum half-life of paracetamol were not changed when administered 1 hour before exenatide injection. No dose adjustment of paracetamol is necessary. The use of a combination of oral contraceptives (30 mcg ethinyl estradiol and 150 mcg levonorgestrel) 1 hour before the administration of exenatide (10 mcg twice daily) did not increase the AUC, maximum or minimum plasma concentrations of ethinyl estradiol or levonorgestrel. Administration of oral contraceptives 30 minutes after exenatide did not change the AUC, but decreased the maximum plasma concentration of ethinyl estradiol by 45% and levonorgestrel by 27–41% and delayed the maximum half-life by 2–4 hours due to delayed gastric emptying. No dose adjustment of oral contraceptives is necessary.
Storage conditions for the drug Byeta
Store in a dark place at 2–8 °C, do not freeze. The exenatide pen syringe should be stored in the refrigerator after each use. However, exenatide can be stored at 25°C for up to 7 days during the 30-day dosing period. The syringe pen must be disposed of within 30 days after the first use. Do not store an exenatide pen with a needle attached.
List of pharmacies where you can buy Byeta:
- Moscow
- Saint Petersburg